Chronic Hepatitis B
Chronic Hepatitis B
Definition 📖
Chronic infection: Presence of HBsAg for > 6 months.
Chronic hepatitis: As above + signs of active viral activity (deranged LFT + elevated HBV DNA)
Screening 🔍
🎯 Targeted populations:
- Family members/household contacts of HBsAg positive person
- Blood donors
- Healthcare workers
- Foreign workers
- Pregnant women
Other high risk groups that should be considered for screening
- IVDU
- Men who have sex with men
- Person with HIV
- Persons seeking evaluation for STD
- Persons in prison/correctional facilities
- Indigenous populations
- Individuals with elevated AST/ALT of unknown aetiology
- Persons with chronic liver disease/ESRF
- Persons with multiple sexual partners
- Transgender
Diagnosis (serological)
Diagnosis of HBV infection is accomplished by HBsAg
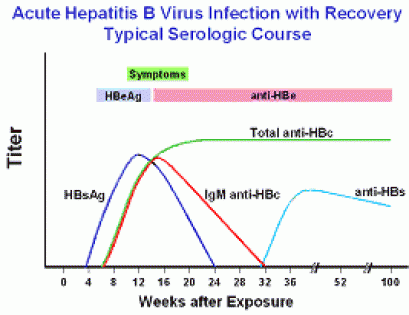
Acute hepatitis with recovery
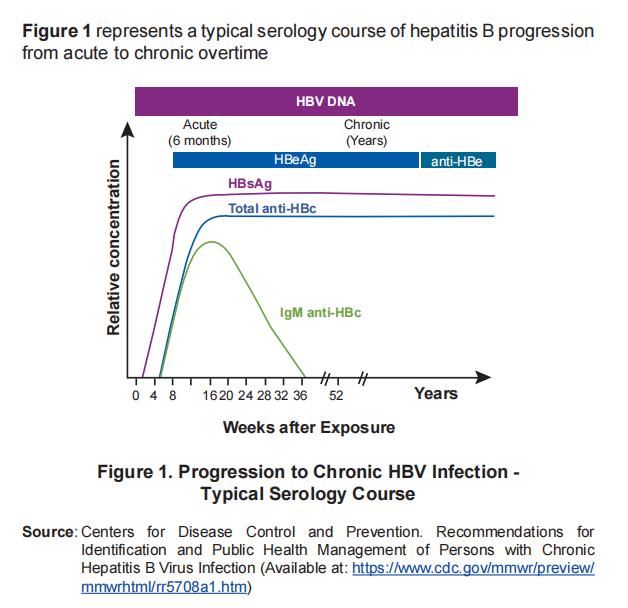
Acute hepatitis progressing to chronic hepatitis
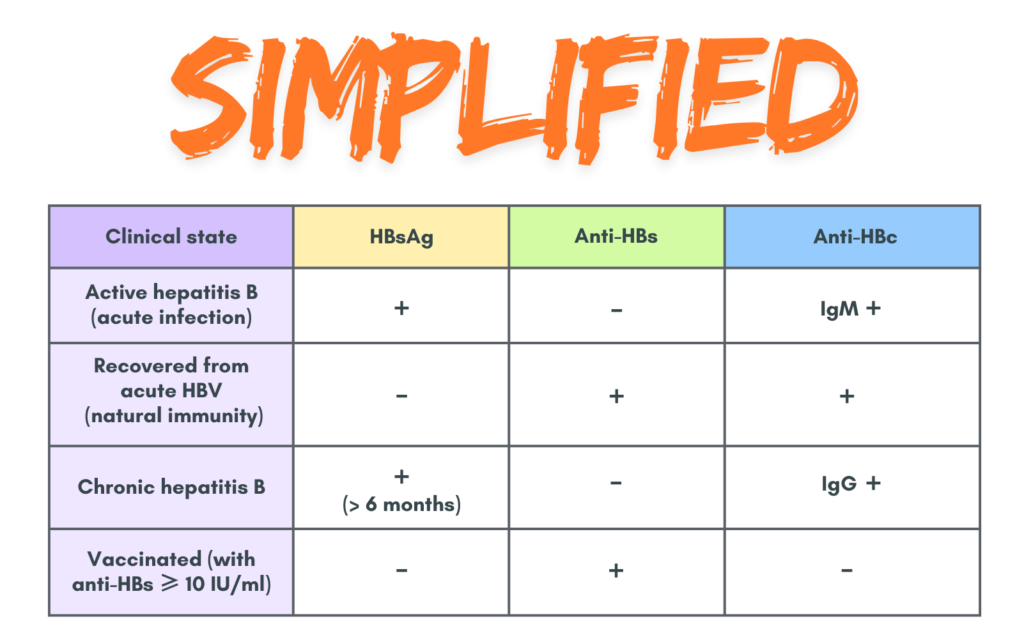
What does the serology tell us?
- Active hepatitis B = HBsAg & IgM anti-HBc +ve, Anti-HBs -ve
- Recovering from acute hep B (natural immunity) = HBsAg -ve, Anti-HBs & Anti-HBc +ve
- Chronic hepatitis B = HBsAg +ve > 6 months
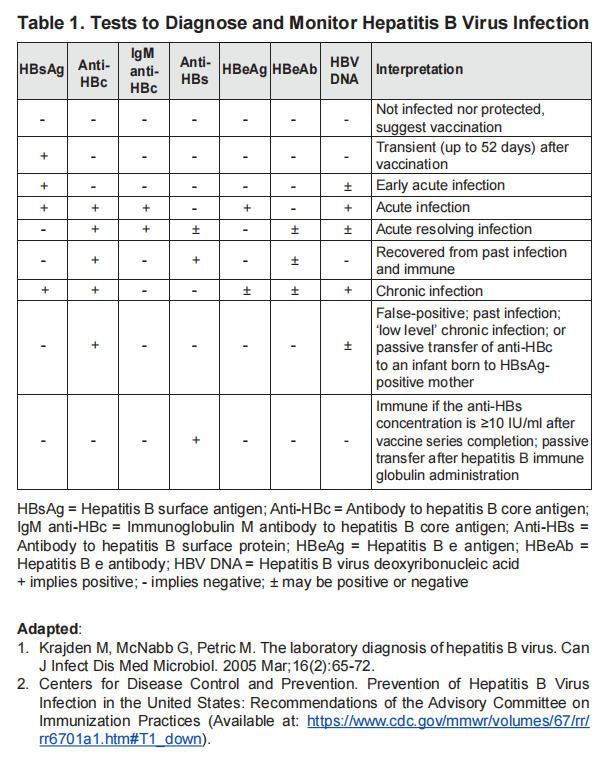
Investigation to include for chronic infection
- HBeAg & HBeAb
- HBV DNA detection and level measurement
- FBC, RP, LFT, INR
- Co-infections with HIV & Hepatitis C
- Co-morbidities & other liver-related disease based on clinical judgement
Initial assessment of CHB patient
Should include:
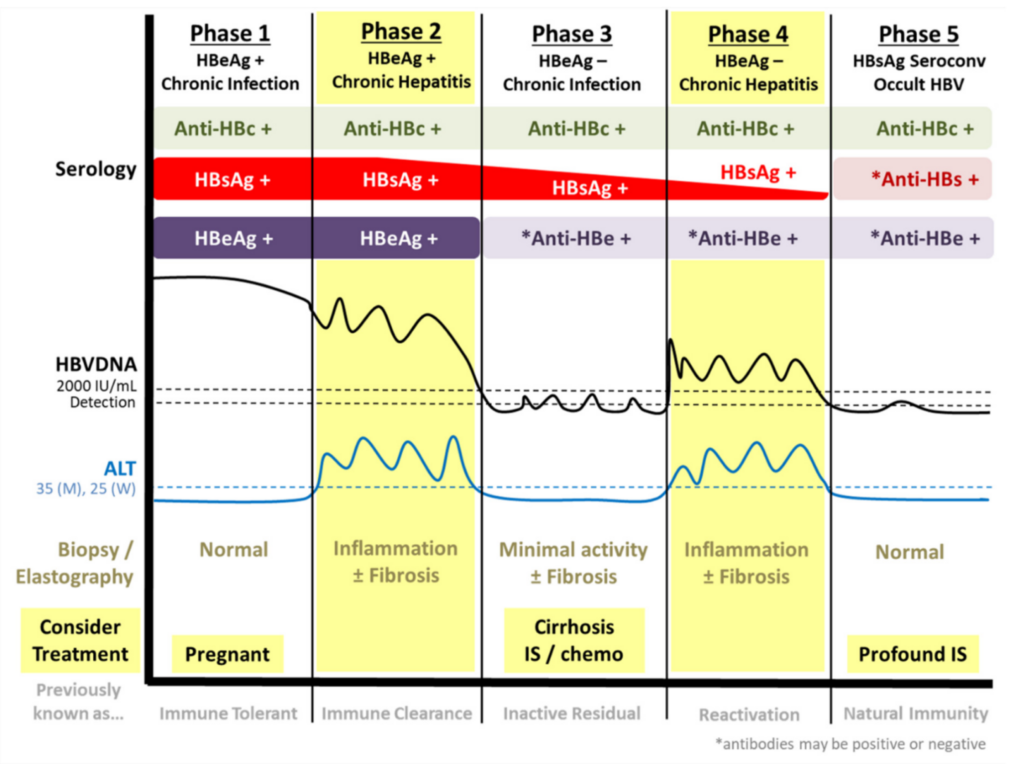
- Phase of infection
- Degree of liver fibrosis/cirrhosis
- Presence of co-infection (HIV, Hepatitis C)
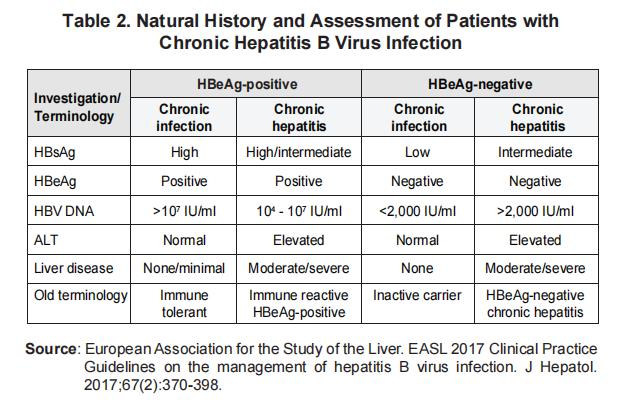
Phase of infection
Can be divided in to HBeAg +ve and HBeAg -ve. Under each can be subdividided into chronic infection or chronic hepatitis.
As mentioned before, chronic hepatitis is when HBSAg is +ve accompanied with deranged LFT and elevated HBV DNA
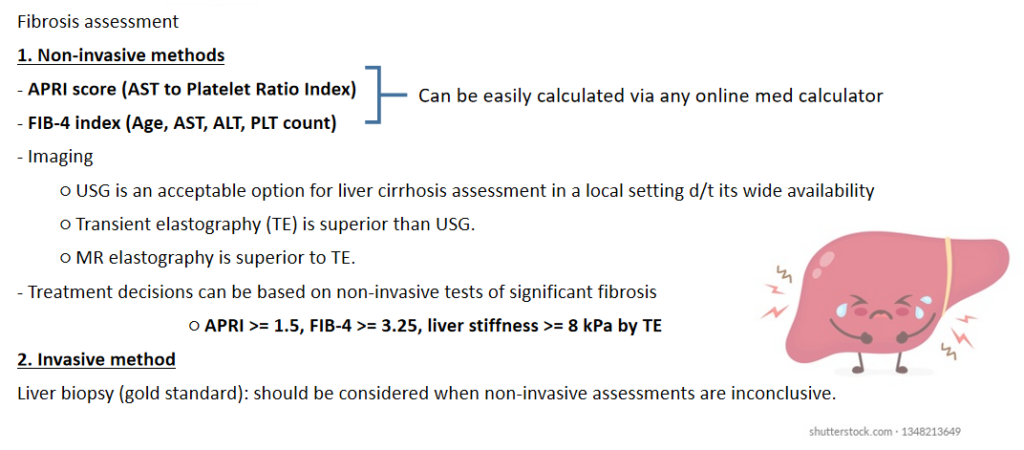
Degree of liver fibrosis or cirrhosis
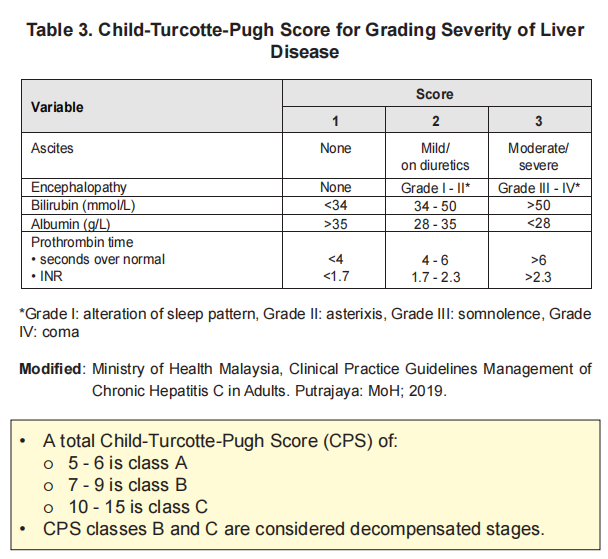
Assessment for compensated & decompensated cirrhosis: Child-Pugh score
Treatment
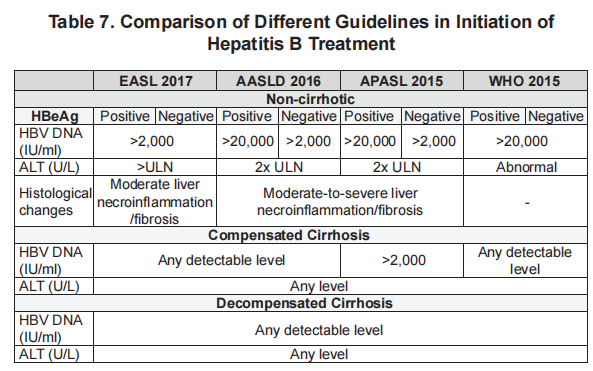
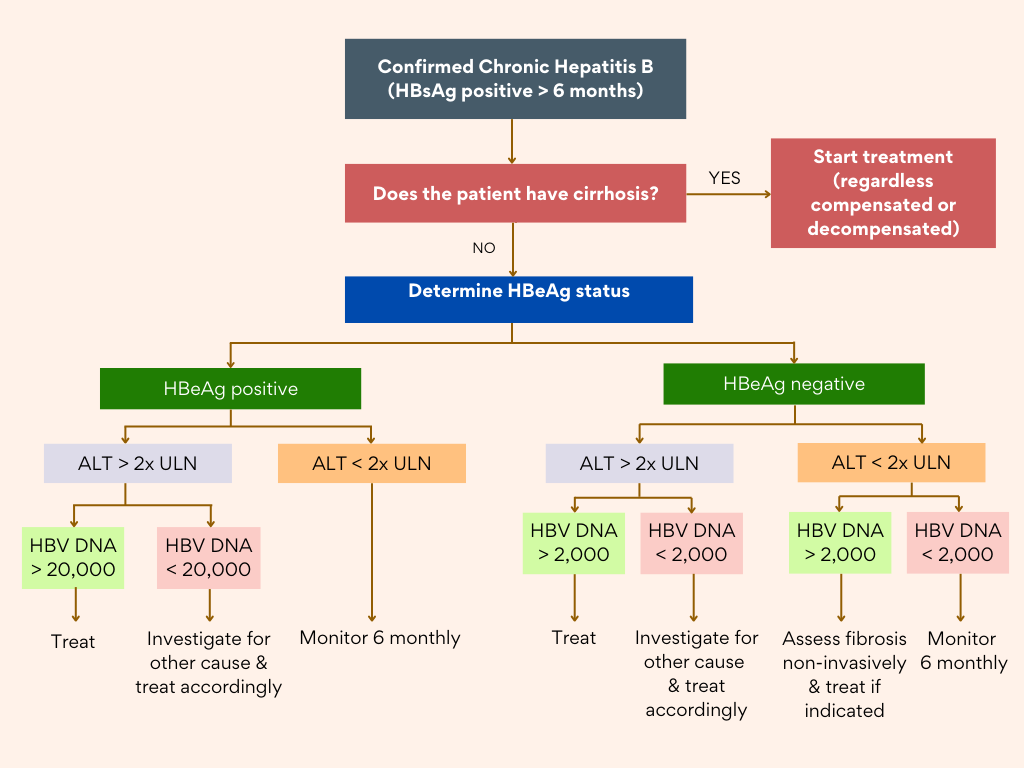
Not all CHB patient require antiviral treatment.
Treatment indications are mainly based on 3 parameters:
- Those with high ALT levels – Liver disease activity
- Evidence of significant fibrosis/cirrhosis (APRI, FIB-4, Fibroscan) – Liver disease activity
- Evidence of active viral replication (HBV DNA should be above a designated threshold) – Viral activity
Treatment in special groups
A. Acute hepatitis B
Short term illness that occurs within the first 6 months after exposure to HBV.
Diagnosis: HBsAg & IgM anti-HBc positive
Most cases of acute HBV hepatitis (95%) do not require specific treatment as they will fully recover spontaneously unless in severe infection.
Only those with severe acute Hep B should be treated with NAs & considered for liver transplantation.
Characteristics of severe acute Hep B:
○ Coagulopathy – INR > 1.5
○ Protracted course i.e. persistent Sx or marked jaundice > 4 weeks; total bilirubin > 3 mg/dL (or direct bilirubin > 1.5 mg/dL)
○ Sign(s) of acute liver failure – encephalopathy or ascites
B. Hepatitis B Flare
Definition: abrupt rise of ALT levels to > 5 times the ULN in CHB.
May occur spontaneously, during or after antiviral, & in the setting of immunosuppression &/or chemotherapy.
Clinical spectrum: Asymptomatic; Symptomatic; Overt acute hepatitis; Hepatic decompensation or failure.
Flares in cirrhotic pt always require immediate antiviral treatment.
In non-cirrhotic pt with decreasing HBV DNA may be followed by HBV &/or HBeAg loss with remission (may be observed for 3 – 6 months first for any indication of treatment)
I’ve included only acute hepatitis B and hepatitis B flare as I think these would be more relevant in primary care setting. Nevertheless there are other groups like pregnancy, co-infection with HIV and Hepatitis C which are included in our Malaysia CPG guidelines, for those who would like to know more about it.
Monitoring CHB patients not on treatment
6 monthly for ALT (& AST for APRI), HBsAg, HBeAg, & HBV DNA levels (where HBV DNA testing is available)
Non-invasive tests (APRI score or FibroScan) to assess for the presence of cirrhosis, in those without cirrhosis at baseline.
Surveillance for HCC with USG ± AFP every 6 months should be done for patients with:
– Liver cirrhosis
– High-risk for HCC (Men > 40 y/o & Women > 50 y/o)
– 1st degree family member with a h/o HCC
– Hep D virus
Prevention 💉
Standard vaccination schedule (0, 1 & 6 months) was more effective than rapid vaccination schedule (0, 1 & 2 months)
IM deltoid was more effective than IM gluteal injection.
Vaccination is advised to all adults who are at high-risk, immunocompromised or seeking protection from HBV infection.
Anti-HBs levels:
At least 10 mIU/mL = protective
1 – 9.9 mIU/mL = non-protective
< 1 = undetectable
Anti-HBs & Anti-HBc +ve = immunity from natural virus protection
Anti-HBs only = Immunity from vaccine
Algorithm on Management
References
Malaysia Health Technology Assessment Section, Medical Development Division, Ministry of Health Malaysia. (2022). Management of chronic hepatitis B in adults: Clinical practice guidelines. Putrajaya: Ministry of Health Malaysia.
