Liver Function Test
Liver Function Test
An assessment of liver function typically involves interpretating:
- Alanine aminotransferase (ALT)
- Aspartate aminotransferase (AST)
- Alkaline phosphatase (ALP)
- Gamma-glutamyl transferase (GGT)
- Bilirubin: total, conjugated (direct) & unconjugated (indirect)
- Prothrombin time (PT), International Normalized Ratio (INR)
- Albumin
- Limited value (not specific for liver injury): Lactate dehydrogenase, Serum globulins, Serum total proteins
These markers should be interpreted based on the reference value of the laboratory in which the test is done as different lab may have different reference ranges.
Aminotransferases – markers of hepatocellular injury
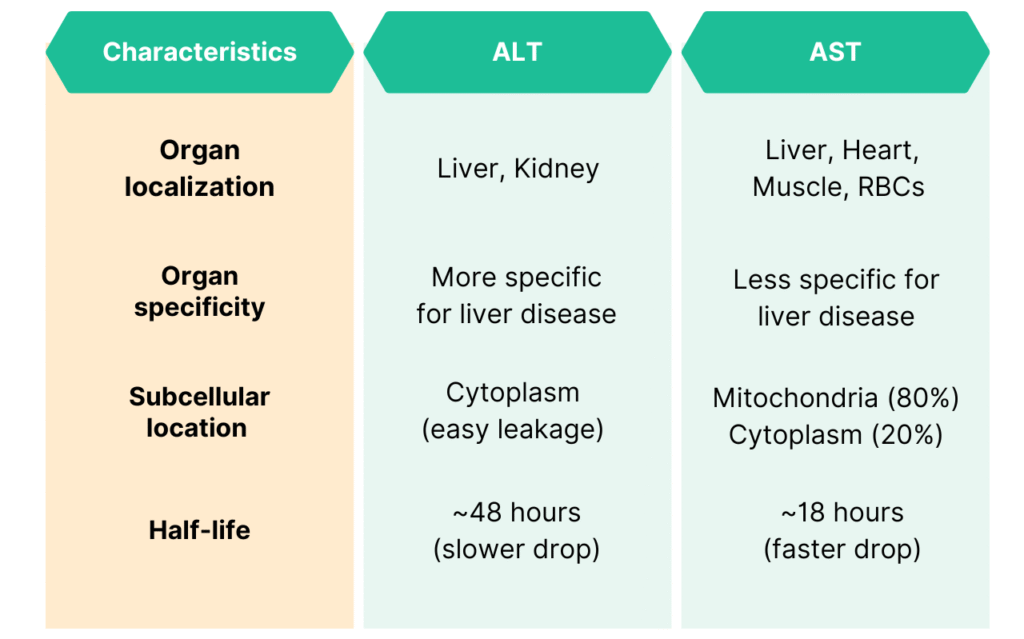
Aspartate Aminotransferases (AST)
- Located primarily in the mitochondria with a relatively low concentration in the cytoplasm.
- Can be found in the liver, cardiac & skeletal muscle, kidneys, brain, pancreas, lungs, leucocytes & red cells.
- Not as sensitive & specific for liver as ALT (as it can be found in other organs also as mentioned).
- AST is released after more severe injury to the hepatocyte, especially when there is injury to the mitochondria (e.g. due to alcohol)
- Elevated AST may be seen also in ischemic heart disease, hemolysis & muscle injury
Alanine Aminotransferase (ALT)
- A cytosolic enzyme which is found in high concentrations in the liver.
- Being located in the cytoplasm of the hepatocytes, it is released into the circulation even with minor injury, making it a more sensitive marker of liver injury.
- ALT levels are usually higher than AST in most liver disease.
ALT vs AST
Hepatocellular injury & not necessarily cell death triggers the release of these enzymes into circulation.
Their levels do not correlate well with disease severity or outcome.
There are also some factors that may affect the levels of these transaminases, e.g.
- Age & gender
- Nutritional status (high BMI)
- Food intake (food can increase ALT/AST level)
- Exercise (muscle)
- Delay in sample processing (AST may be released from the RBCs)
Cholestasis markers
Alkaline phosphatase (ALP)
- Present in high concentration in the microvilli of the bile canaliculus. Can also be found in other tissues e.g. bone, intestine & placenta.
- Benign transient hyperphosphatasemia can lead to significantly increased plasma ALP (often to several thousand IU/L)
– This is a benign condition and the markedly elevated ALP often return to normal in 6 – 8 weeks.
– Transient hyperphosphatasemia is often associated with concurrent infections, especially GIT infections. - During growth, elevated levels of ALP may be seen in children & adolescent due to the increased osteoblastic activity.
- An unexplained high ALP should always be confirmed with a repeat fasting sample.
- Increased level up to 2 or 3 fold may be normal in the 3rd trimester of pregnancy due to the placental isoenzyme.
Gamma-glutamyltransferase (GGT)
- More specific for biliary disease compared to ALP as it is not present in bone.
- Often interpreted to identify the organ source of an isolated serum ALP elevation, e.g. raised ALP and GGT = Liver is the source; whereas raised ALP with normal GGT = source may be from the bone
- GGT levels increased more (around 12 fold) when compared to ALP (around 3 fold) in obstructive liver disease, thus making it slightly more sensitive in obstructive assessment.
- Other possible cause of raised GGT (other than obstruction) includes:
– Obese individuals (due to steatosis)
– Liver disease that cause fibrosis &/or fibrosis e.g. alcoholic cirrhosis, PSC, PBC, hemochromatosis, etc.
– Space-occupying lesion, including malignancy - Granulomatous disease e.g. TB & sarcoidosis
Synthetic Function Tests
Albumin
- Synthesized by the hepatic parenchymal cells.
- Half-life: 21 days
- In an individual with liver disease, fall in serum albumin reflects decreased synthesis.
- Acute liver disease: Serum albumin levels often normal
- Chronic liver disease: Reduced serum albumin levels
- Low serum albumin with normal liver function may be due to:
– Malnutrition: poor protein intake
– Protein loss: nephrotic syndrome, malabsorption or protein-losing enteropathy
Prothrombin time (PT)
- Measures the rate of conversion of prothrombin to thrombin which requires coagulation factors.
- All coagulation factors are synthesized by the liver, except for factor VIII.
- In an individual with liver disease, prolonged PT reflects reduced liver function.
- Is a specific marker of liver failure but not liver injury.
- Useful for monitoring degree of liver dysfunction.
- Delayed PT with normal liver function may be due to:
– Warfarin treatment
– Consumptive coagulopathy, e.g. DIC
– Vitamin K deficiency
Serological tests – Mainly used in diagnosis of autoimmune liver disease
a) Autoimmune hepatitis
- Type 1: Anti-nuclear antibody (ANA), Smooth muscle antibody (SMA)
- Type 2: Anti-liver kidney microsomal antigen type-1 (anti-LKM1), anti-liver cytosol type 1 (anti-LC1)
b) Primary biliary cirrhosis (PBC)
- Anti-mitochondrial antibodies (AMA), disease-specific ANA
c) Sclerosing cholangitis
- Primary sclerosing cholangitis (PSC), mostly affects adult men: atypical perinuclear anti-neutrophil cytoplasmic antibody (p-ANCA), also termed perinuclear anti-neutrophil nuclear antibodies (p-ANNA)
- Autoimmune sclerosing cholangitis (childhood disease): serological features resemble type 1 AIH
Others
Alpha-fetoprotein (AFP) – Used as a tumor marker to detect & monitor primary hepatocellular malignancies, e.g. hepatoblastoma & HCC.
CA 19-9: Useful in monitoring the activity of PSC which may progress to cholangiocarcinoma.
Serum ferritin: to identify hemochromatosis (keep in mind that ferritin is also an acute phase reactant which may be elevated in other illnesses as well.)
Interpreting the markers
The R Ratio
This ratio may be helpful to determine the pattern of liver injury, whether is hepatocellular, cholestatic or mixed.
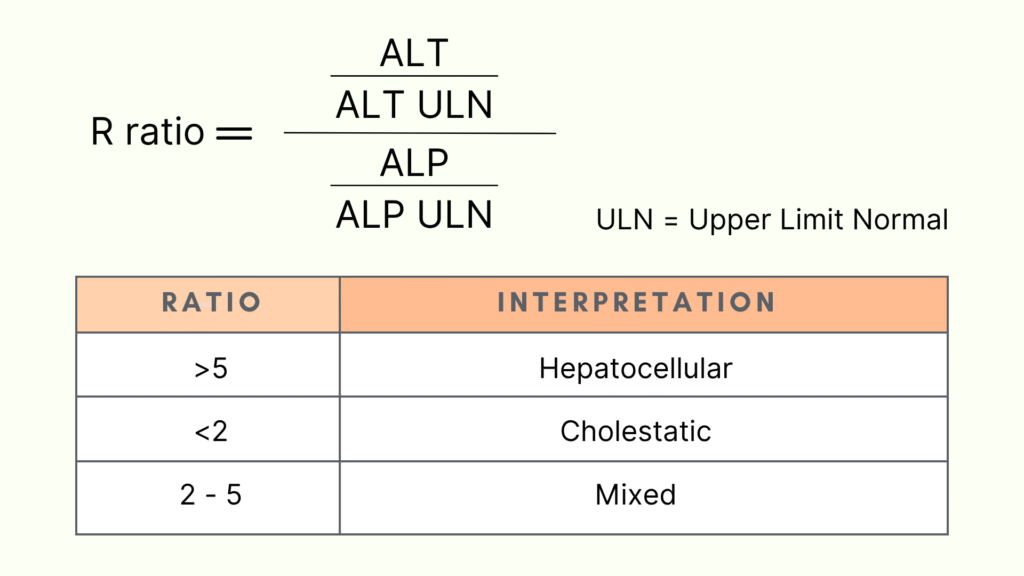
Type of liver injury
Hepatocellular pattern – AST & ALT are elevated & out of proportion to ALP
a) ALT-predominant
Acute/chronic viral hepatitis, steatohepatitis, acute Budd-Chiari syndrome, ischemic hepatitis, autoimmune, hemochromatosis, medications/toxins, autoimmune, alpha1-antitrpsin deficiency, Wilson disease, Celiac disease
b) AST-predominant
Alcohol-related, steatohepatitis, cirrhosis, non-hepatic (hemolysis, myopathy, thyroid disease, exercise)
Cholestatic pattern – Raised ALP + GGT + bilirubin out of proportion to AST & ALT
a) Hepatobiliary causes
Bile duct obstruction, primary biliary cirrhosis, primary sclerosing cholangitis, medication-induced, infiltrating diseases of the liver (sarcoidosis, amyloidosis, lymphoma, etc), cystic fibrosis, hepatic metastasis, cholestasis
b) Non-hepatic causes
Pregnancy, chronic renal failure, lymphoma or other malignancies, congestive heart failure, childhood growth, infection or inflammation.
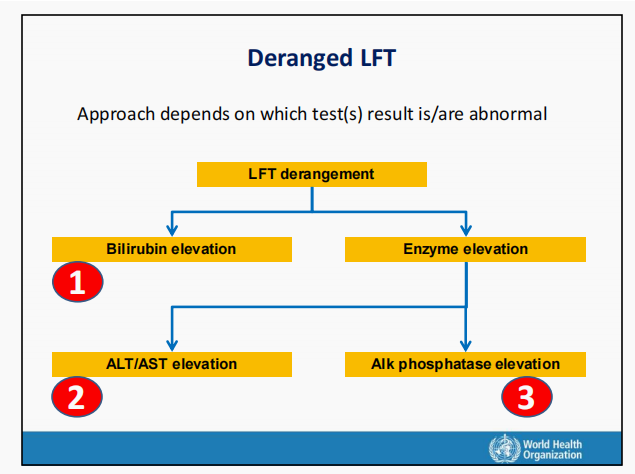
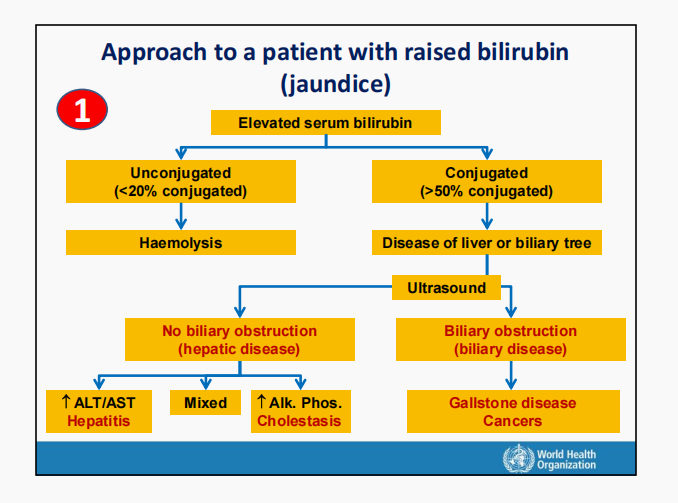
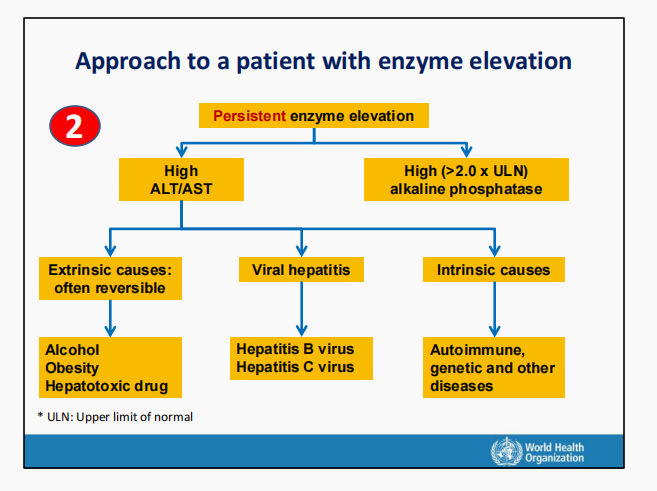
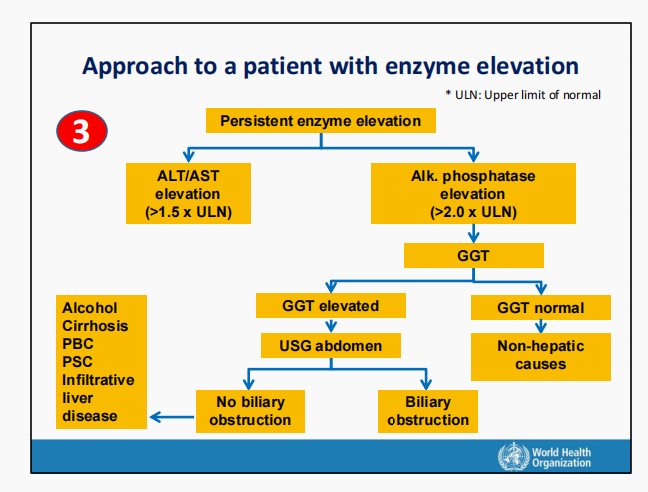
Flowchart
Below is the flowcharts that i found in one of the WHO training modules which i believe will be helpful in our clinical practice.
The first step is to note the LFT derangement, whether it is bilirubin elevation or enzyme elevation.
- If bilirubin is elevated, then is it unconjugated or conjugated bilirubinemia.
- If enzyme is elevated, then is it AST/ALT elevation or ALP with or without GGT elevation.
These can guide us to the probable diagnosis and to investigate accordingly.
References
- SEARO Regional Office for the South East Asia (RGO), WHO South-East Asia, WHO Western Pacific. (2020, July 28). Training Modules on Hepatitis B and C Screening, Diagnosis and Treatment, Session 4 Interpretation of Liver Function Tests. World Health Organization. https://www.who.int/publications/i/item/9789290227472
- Lala V, Zubair M, Minter DA. Liver Function Tests. [Updated 2023 Jul 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482489/
