Migraine

Migraine
Pathophysiology
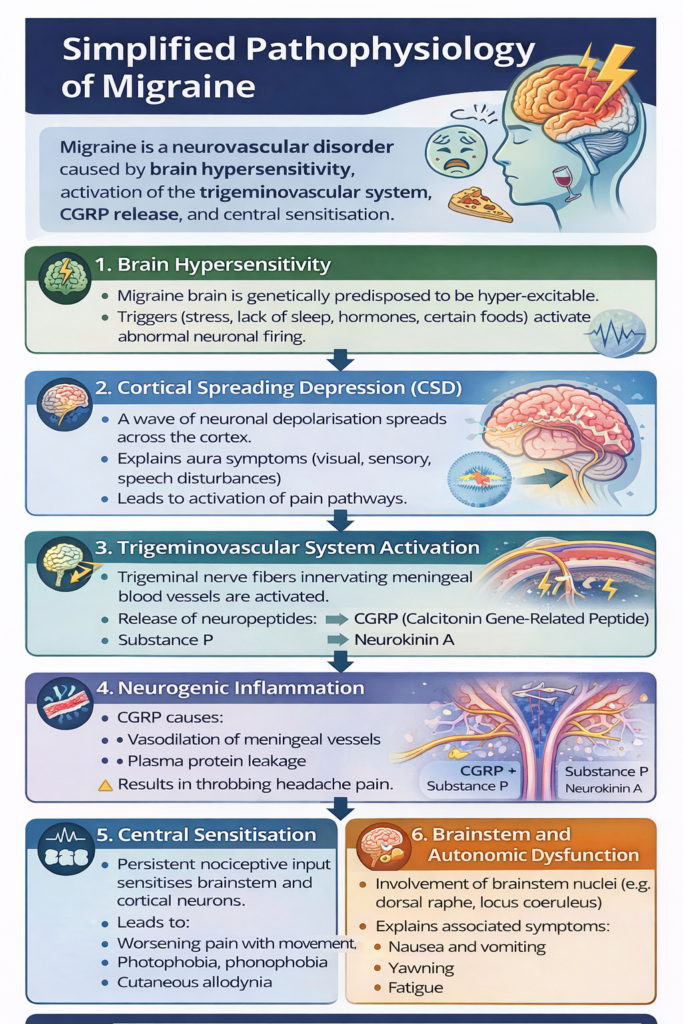
CSD = Cortical spreading depression CGRP = Calcitonin gene-related peptide
Migraine triggers


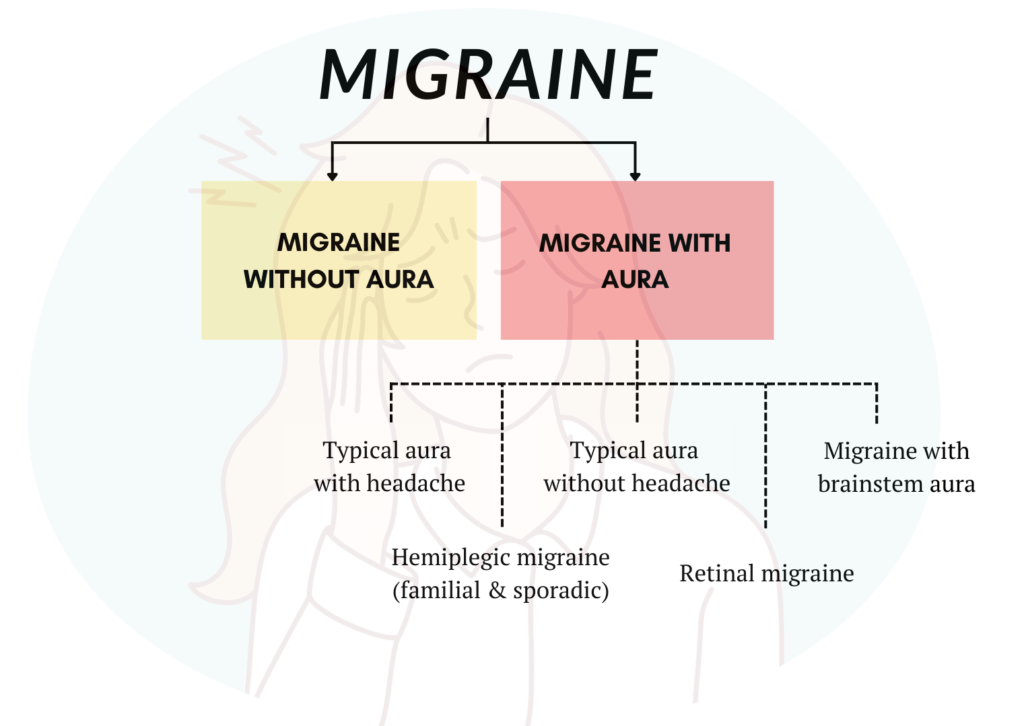
Classification
A. Episodic
- Low frequency: <10 headache days per month
- High frequency: 10 – 14 headache days per month
B. Chronic
- 15 or more headache days per month for more than 3 months
C. With our without aura
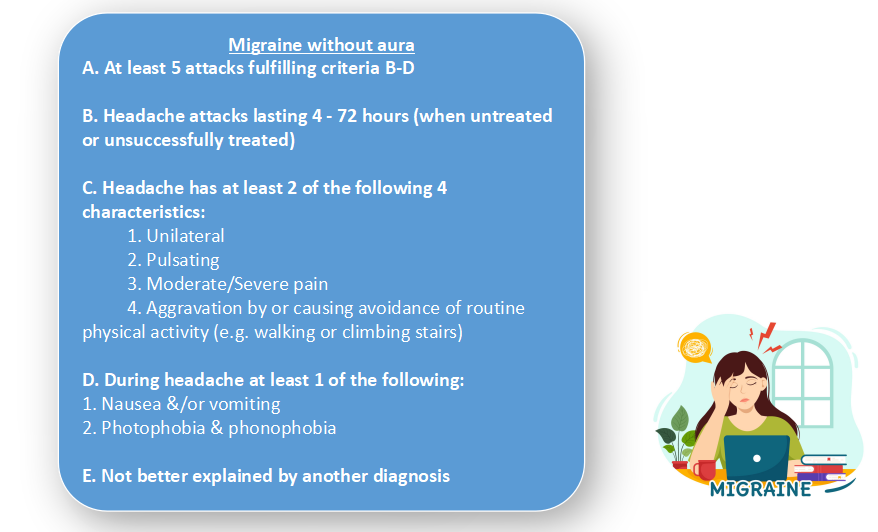
Diagnostic criteria
Migraine without aura
Migraine with aura
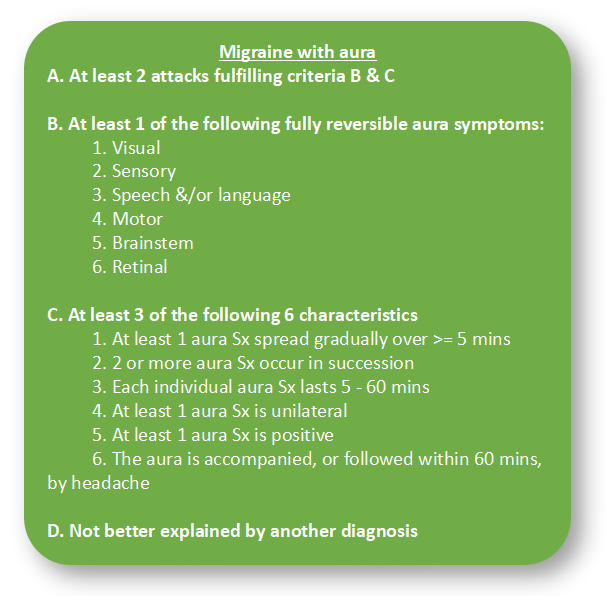
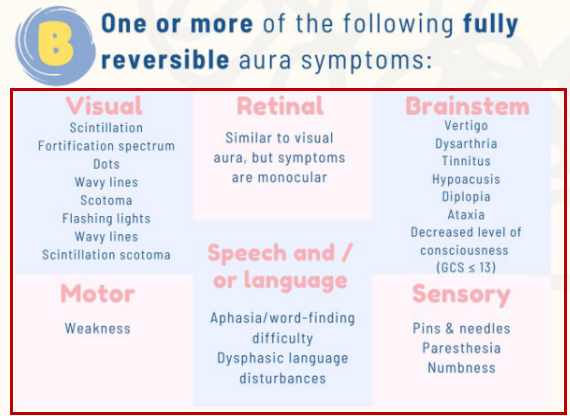
Image from Neudrawlogy
It is important to note that different presentation of aura symptoms may mimic stroke.
4 Phases of Migraine
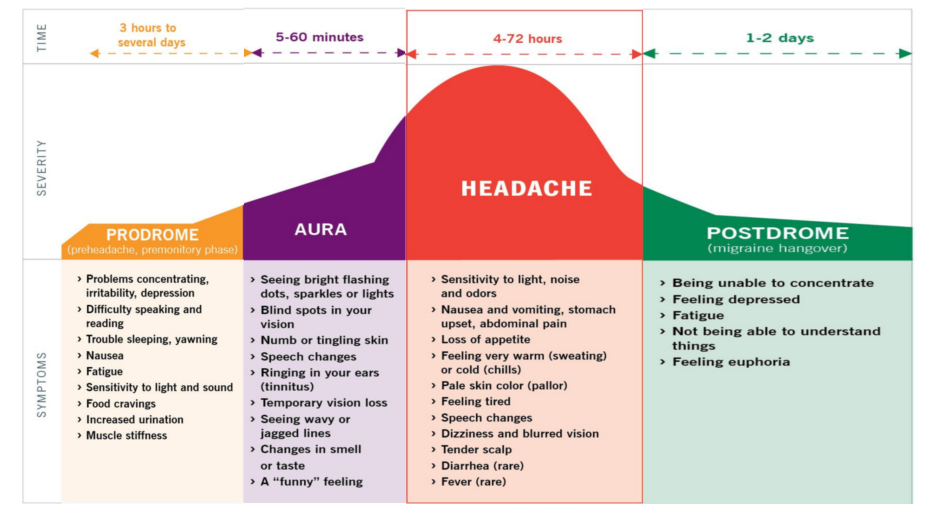
Migraine attacks often progresses through 4 phases – prodrome, aura, headache, and postdrome – although not all patients experience every phase.
Early recognition, especially during the prodrome, enables timely treatment that may lessen the severity or abort the attack.
Understanding the phases also helps with differentiation migraine from other conditions.
🚩Red flags of headache
Mnemonic: SNOOP
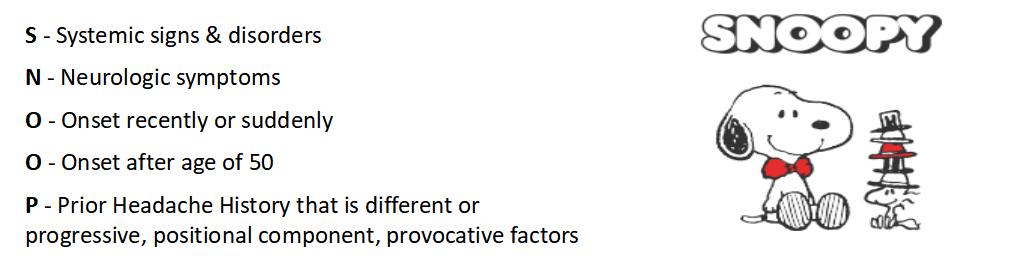
Presence of red flags prompt further assessment TRO other more sinister causes.
Treatment of migraine

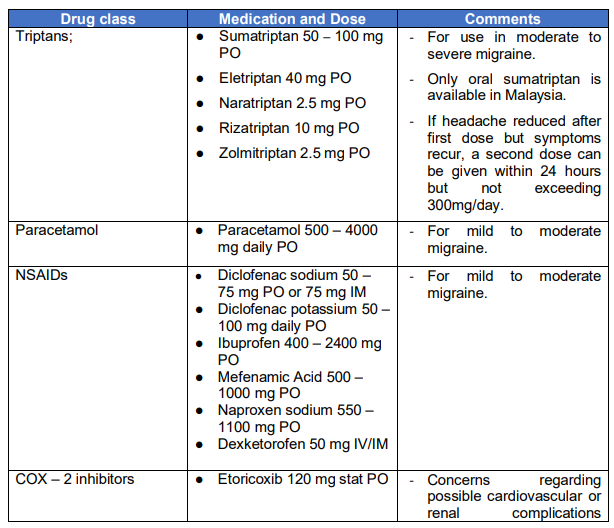
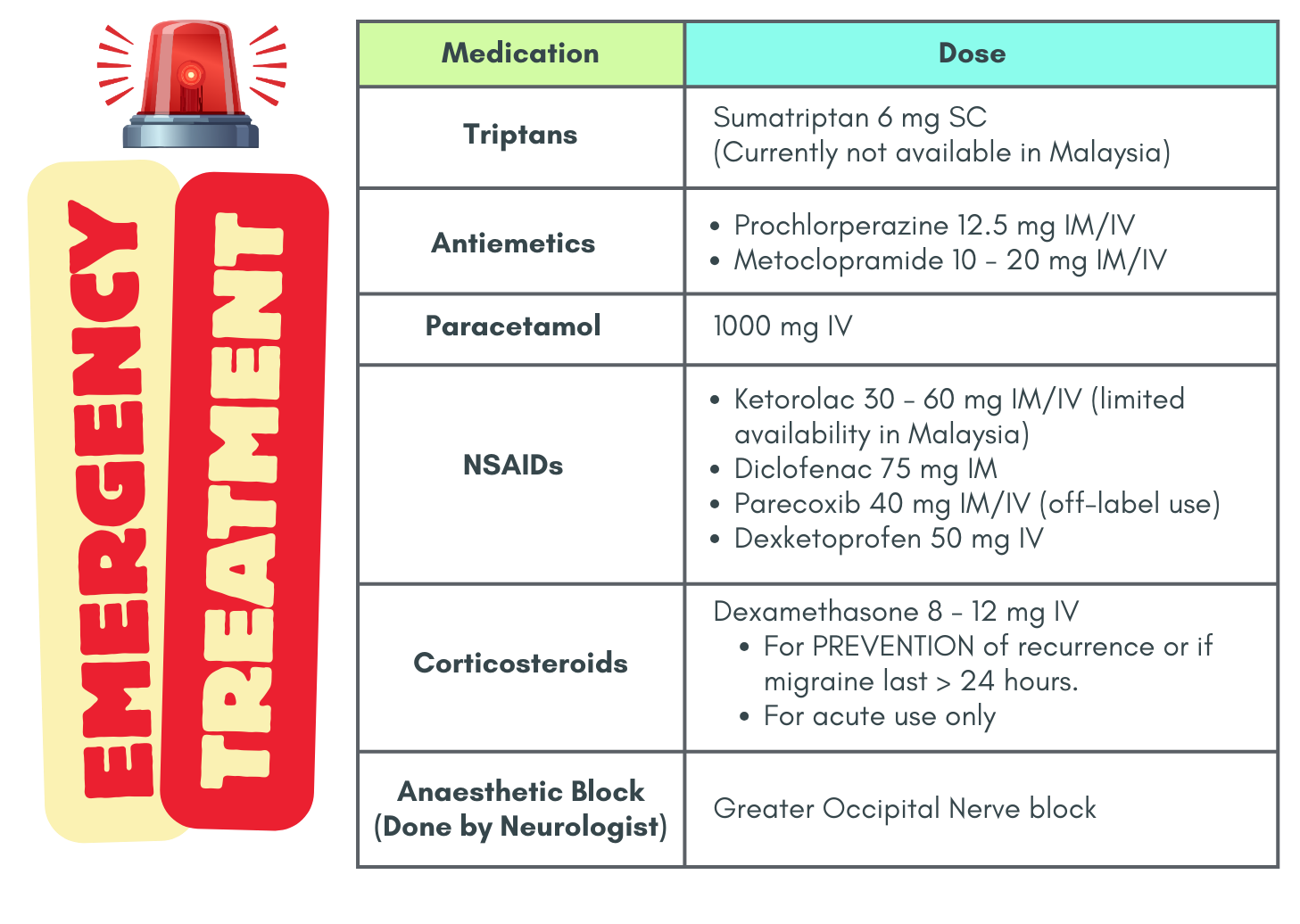
Management of Migraine in emergency settings
For patient who are having severe pain, not responding to usual analgesics
Identification of any red flag symptoms
For rapid effect & relief, IV or IM route is preferred. Always consider the presence of allergies & co-morbid illnesses.
Additional notes
Regarding antiemetics
- Can be considered 1st line & is useful for relief of nausea.
- Adverse events may include akathisia & drowsiness
- Adequate hydration with IV fluids is recommended, especially with repeated vomiting.
Combinations of the above medication may be useful, though evidence is lacking.
No indication for tramadol or other opioids unless unable to tolerate other medications (e.g. due to allergy). Caution when using due to risk of inducing nausea & sedation.
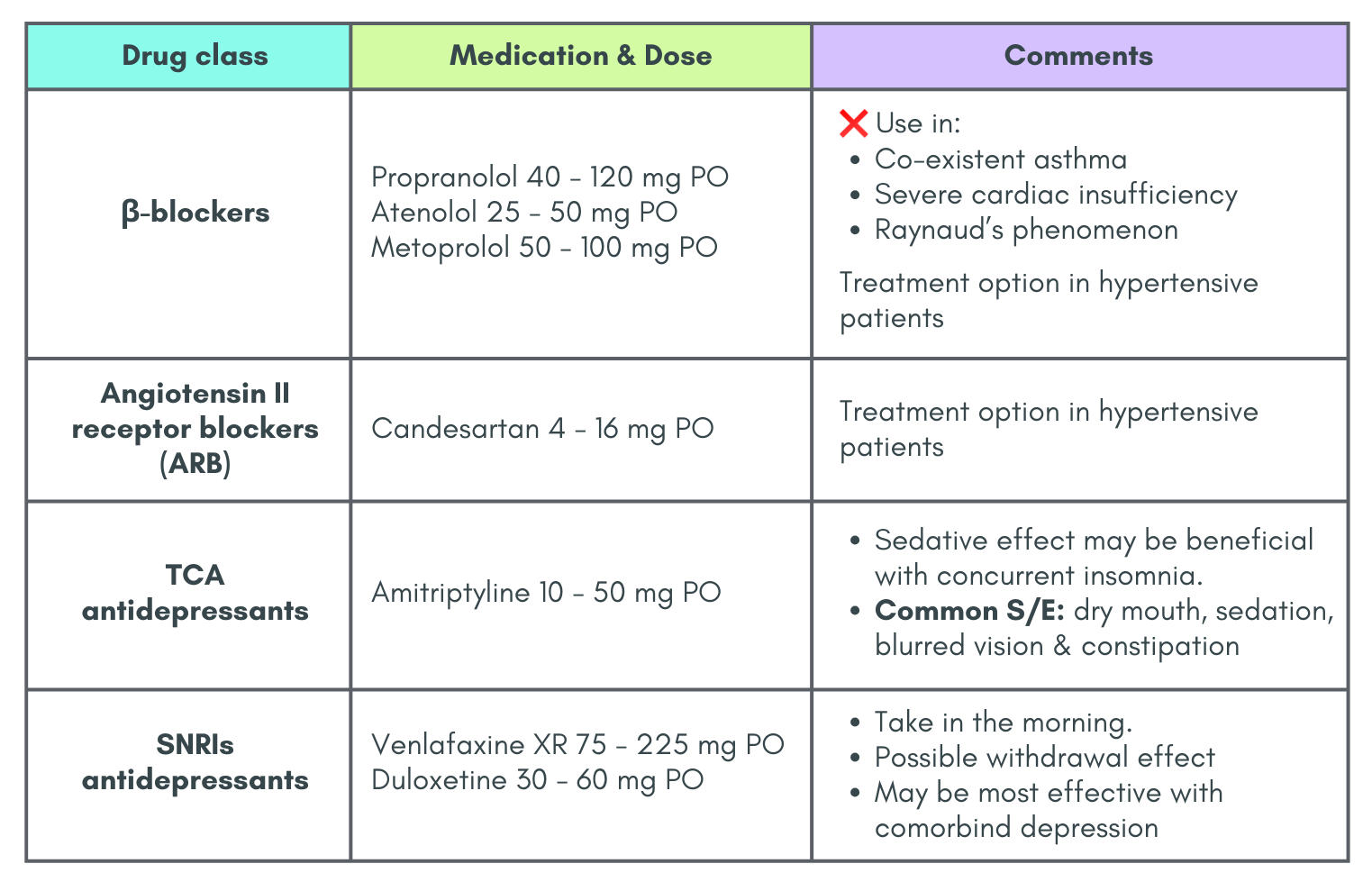
Preventive therapy
Indications:
- Attacks significantly interfere with pt’s daily routines despite acute treatment.
- Frequent attacks (≥ 4 monthly headache days)
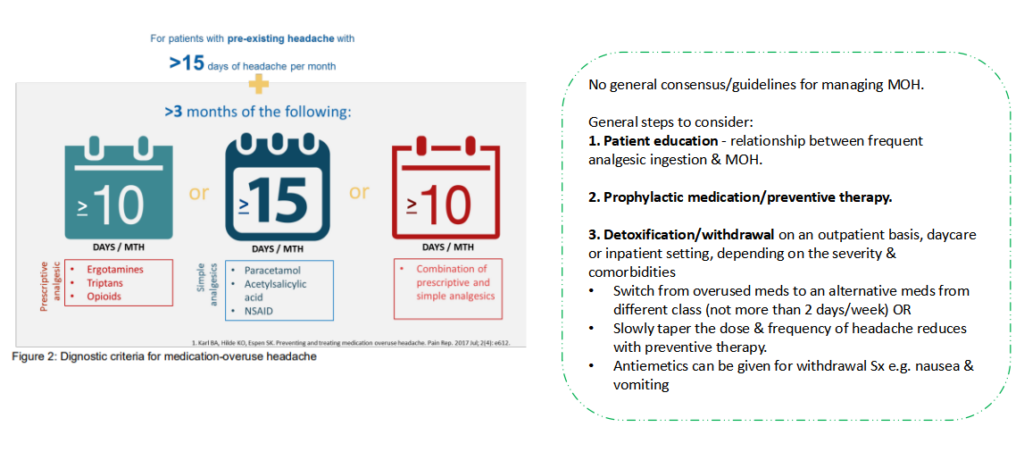
- Contraindication to, failure of, or overuse of acute treatments (Medication Overuse Headache), with overuse defined as:
– 10 or more days per month for ergot derivatives, triptans, opioids, combination analgesics, & a combination of drugs from different classes that are not individually overused.
– 15 or more days per month for non-opioid analgesics, PCM, & NSAIDs - Side effects with acute treatment
- Patient preference
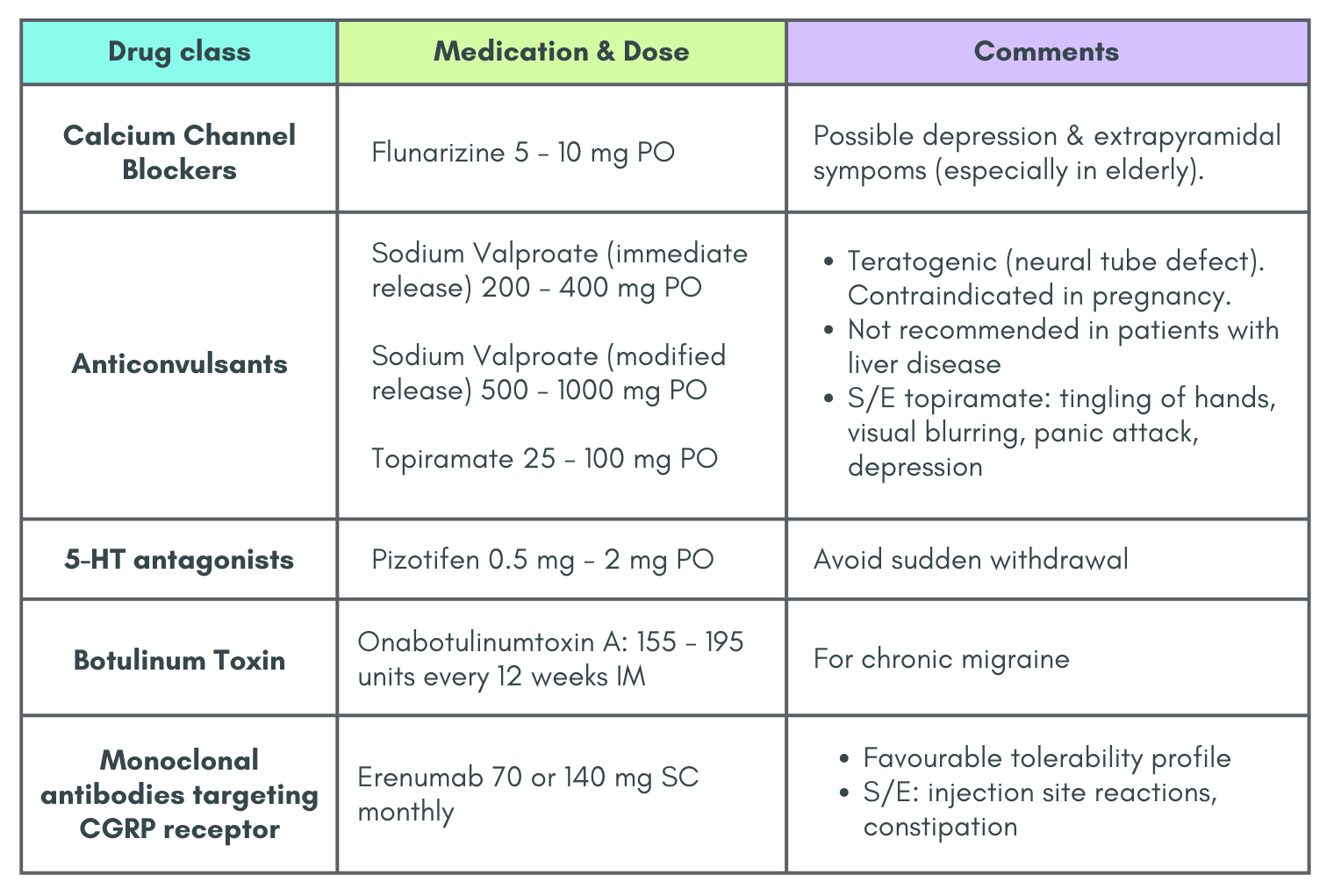
Drug Therapy for Prophylaxis of Migraine
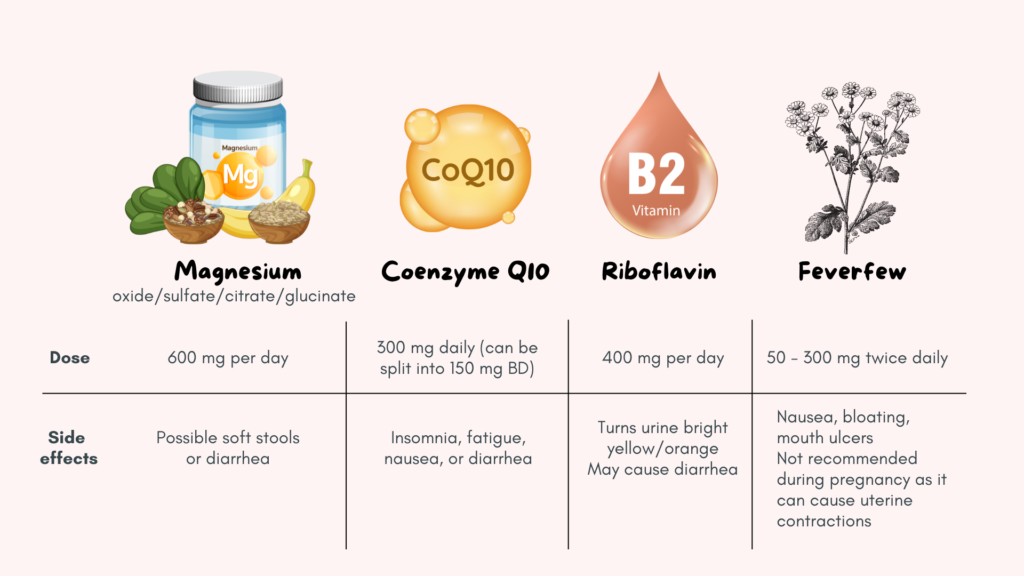
Supplements to consider for migraine prevention
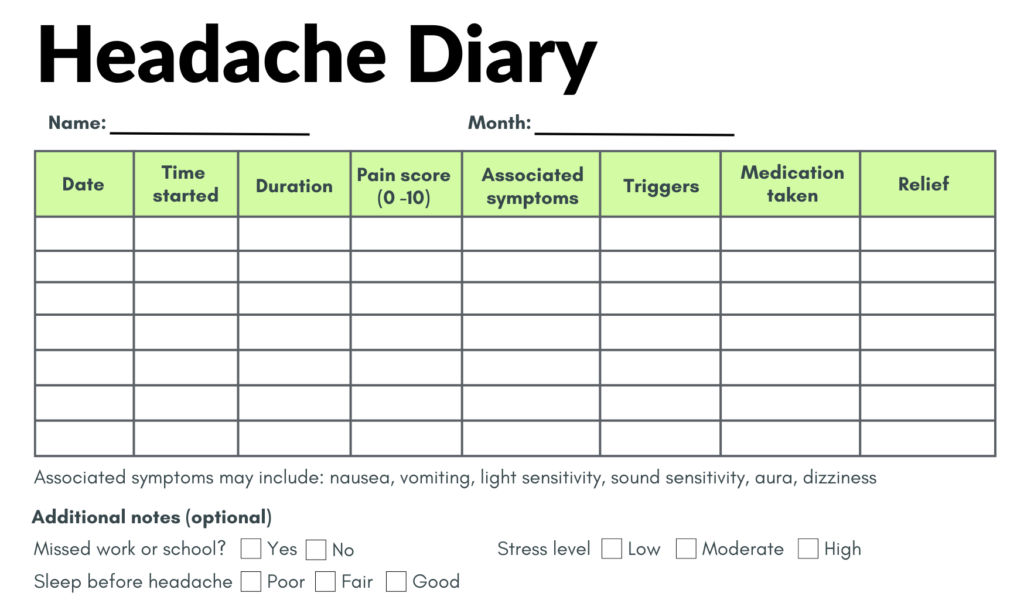
Headache diary
A headache diary is an important tool for migraine management as it helps in:
- Identifying migraine triggers
- Recognizing phases of migraine – for timely treatment
- Determining frequency of attacks
Below is an example of an headache diary. This template need not be followed strictly and may be modified to suit the patient’s preferences and convenience. There are various templates available online which is just one search away =)
Complications of migraine
1. Status migrainous: Debilitating migraine > 72 hours
Diagnostic criteria:
- Headache criteria fulfilling criteria B & C (as mentioned above)
- Occurring in a patient with migraine ± aura, & typical of previous attacks except for its duration & severity.
- Both of the following characteristics:
– Unremitting for > 72 hours
– Pain &/or associated symptoms that are debilitating - Not better accounted for by another ICHD-3 diagnosis
2. Persistent aura without infarction: Aura symptoms > 1 week without evidence of infarction on imaging
3. Migrainous infarction
One or more aura symptoms occurring in association with an ischaemic brain lesion in the appropriate territory demonstrated by neuroimaging, with onset during course of a typical migraine with aura attack.
Diagnostic criteria:
- Migraine attack fulfilling criteria B & C.
- Occurring in a patient with migraine + aura and typical of previous attacks except that one or more aura symptoms persists > 60 mins.
- Neuroimaging demonstrates ischemic infarction in relevant area.
- Not better accounted by another ICHD-3 diagnosis.
4. Migraine-aura triggered seizure
Seizure triggered by an attack of migraine with aura, occurring during or within 1 hour after a migraine attack.
Special issues in Migraine
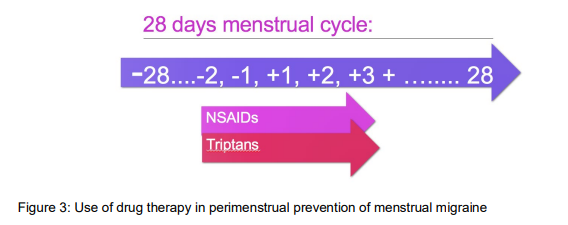
A. Menstrual migraine
Caused by oestrogen withdrawal trigger & release of uterine prostaglandins during menses –> excitability & neurogenic inflammation
Attacks of migraine ± aura occurring on day 1 or 2 of menstruation in at least 2 out of 3 menstrual cycles
Short term perimenstrual prevention (‘mini-prophylaxis’)
- Either NSAIDs (if no contraindication; i.e. naproxen sodium 550 mg BD with GI protection) or triptans (sumatriptan 25 mg TDS or frovatriptan 2.5 OD) or combinations can be given premenstrually, especially for women with regular cycle.
- Start 2 days prior or at onset of menstrual migraine for a total duration of 5 days.
B. Migraine, stroke & hormonal contraceptives
Migraine with or without aura in presence with 2 vascular risk factors are associated with stroke in younger women of < 55 y/o.
COC should be used cautiously in clinical practice for women of reproductive age with high migraine prevalence.
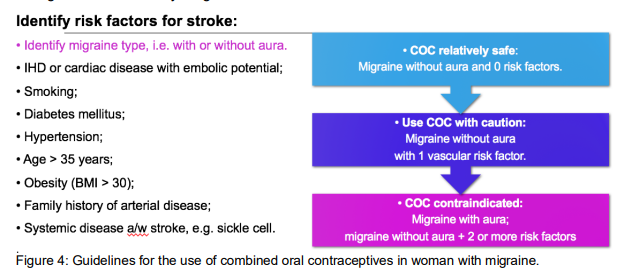
If a young woman who is already taking the COC pill develops new persisting headache/new-onset migraine aura/dramatic increase in headache frequency & intensity/unusual & prolonged auras, the COC should be stopped.
C. Migraine and pregnancy
Have high suspicion if the women developed the first presentation of migraine with aura during pregnancy or if there is a change in the usual migraine symptoms.
Important differentials to consider: pre-eclampsia, cerebral venous thrombosis, AV malformation

Though ibuprofen may be used for short term in pregnancy (as listed above), in my opinion it is best to consult O&G or neurologist first.
Medication overuse headache
References
- Merican, J. S., Goh, K. J., Wan Sulaiman, W. A., Chan, P. H., Puvanarajah, S. D., Tai, M. L. S., & Chee, K. Y. (2021). Consensus guidelines on the management of headache 2021. Malaysian Society of Neurosciences.
- Mayans, L., & Walling, A. (2018). Acute Migraine Headache: Treatment Strategies. American family physician, 97(4), 243–251.
- Rajapakse T, Pringsheim T. Nutraceuticals in migraine: A summary of existing guidelines for use. Headache. 2016;56(4).
