Hypertension

Hypertension
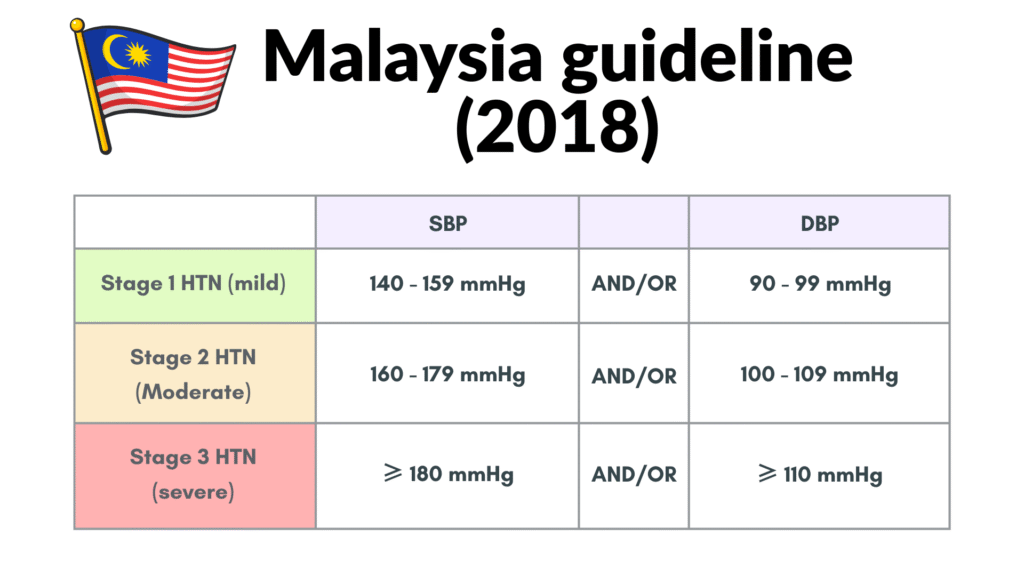
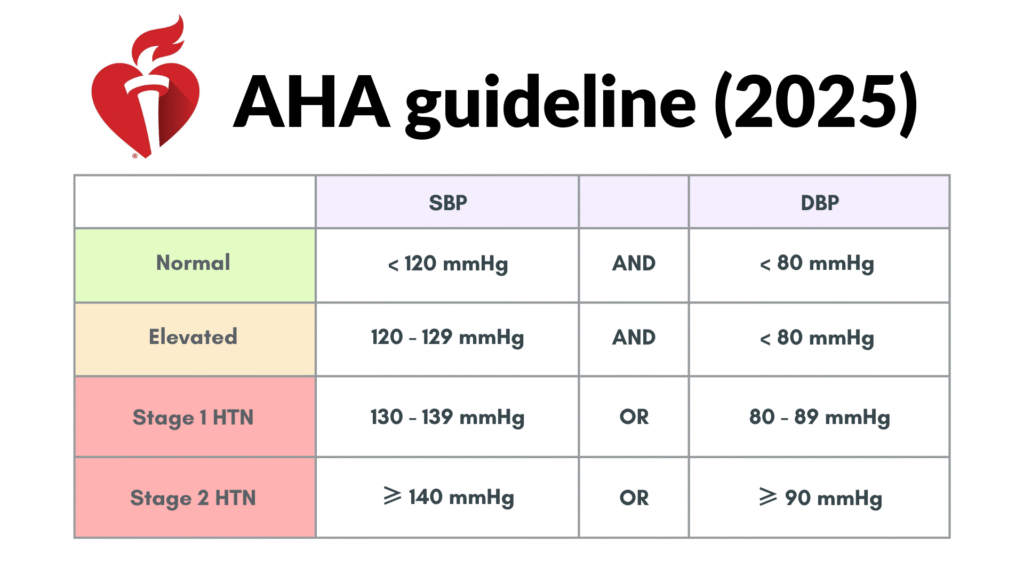
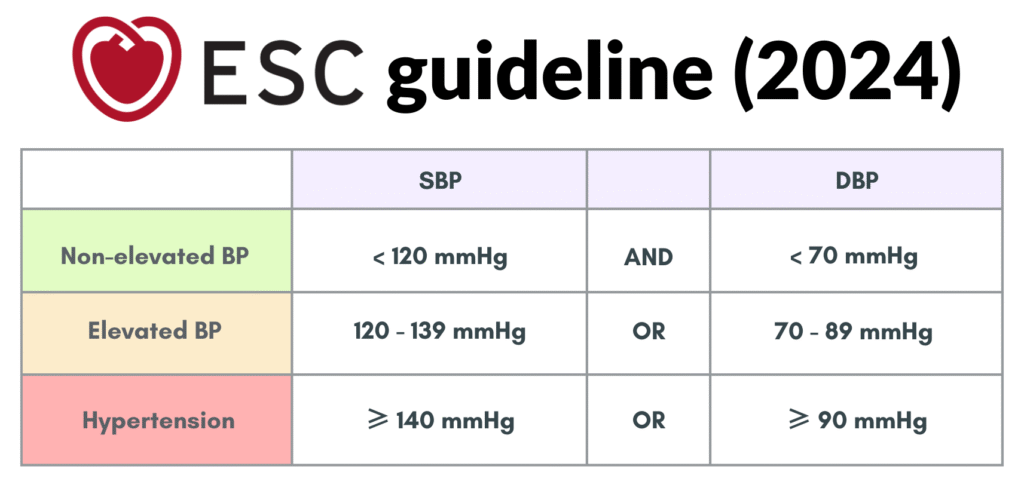
BP categories
This post will mainly discuss on hypertension based on Malaysia CPG guideline, ESC guideline & AHA guideline.
It is important to note that these blood pressure (BP) values mentioned above are based on BP measured during clinical consultation (Office BP).
Both the ESC and AHA guidelines include an “Elevated BP” category (AHA: 120–129/<80 mmHg; ESC: 120–139/70–89 mmHg).
The Malaysian guideline, however, begins hypertension staging at ≥140/90 mmHg and does not define a separate elevated range.
Although not explicitly stated as a category in the Malaysian guideline, the concept of “elevated” BP remains clinically relevant and will be discussed further.
It is also important to note that Systolic BP increases progressively with age, while diastolic BP rises until around 50 years, stabilizes for roughly a decade, and then decreases.
DBP is the primary cardiovascular risk marker before age 50, after which SBP becomes more predictive.
BP measurement
BP measurement can be divided into:
- Office BP – measured at clinics
- Out-of-office BP – includes Home BP Monitoring (HBPM) & Ambulatory BP Monitoring (ABPM)
Office BP should be based on an average of ≥2 BP measurements obtained on ≥2 separate occasions to minimize error & provide a more accurate estimation.
HBPM involves patient measuring BP at home over days – weeks using a validated electronic device.
Situations where HBPM is useful:
- Initial evaluation of BP
- Confirming diagnosis of hypertension
- Detecting isolated office (white coat) hypertension
- Identifying masked hypertension (normal office BP, with elevated home BP)
- Monitoring response to treatment
- Diagnosing true resistant hypertension
- Supporting treatment adherence
- Improving overall BP control
In terms of HBPM, mean SBP > 135 mmHg &/or DBP > 85 mmHg should be considered as elevated.
ABPM involves using a device to measure BP automatically over 24 hours, with readings i.e. every 15 – 30 minutes during the day and 30 – 60 minutes at night. Though it can be useful in selected clinical situations, most risk estimates and treatment benefits are primarily based on office BP readings. ABPM rarely changes treatment decisions and its high cost limits widespread use.
Measuring blood pressure
Proper BP measurement matters, as errors can misclassify patients.
General preparation
- Avoid 🚭smoking, ☕caffeine, 🍝 food or 🏃♂️exercise for at least 30 mins.
- 💺Sit quietly for at least 1 min with back & arm supported and legs uncrossed.(e.g. resting on the table)
- Use the correct bladder cuff size with arm placed at heart level.

🏥 For clinic/office BP
- Take at least 2 readings, 1 – 2 mins apart, in the same arm & position.
- If difference > 10 mmHg –> Take a 3rd reading.
- Average the last 2 readings.
- At first visit:
– Measure BP in both arms, & the higher reading is taken as the BP measurement.
– If such a difference is recorded, all subsequent BP readings should use the arm with the higher reading.
– Assess also for any orthostatic/postural hypotension.
🏠 For HMBP
- Minimum 3 days (ideally 7 days)
- Should be measured at about the same time
– 🌅 In the morning (before drug intake if on treatment) &
– 🌆 Evening (before meal) - Take 2 readings each time, at least 1 min apart
- Record readings immediately in a logbook/device memory
- Interpretation of HMBP:
– Disregard readings from day 1
– Average the remaining BP measurements (at least 3 days)
– Mean home SBP > 135 mmHg &/or DBP > 85 mmHg should be considered as elevated.
Diagnosis of HTN (ESC)
Out-of-office BP measurement is preferred for confirming HTN.
If initial screening office BP is:
A) 120 – 150/70 – 99
- Measurement of HBPM is recommended to confirm.
- If not, repeat office BP measurement on at least 2 visits
B) SBP > 160 mmHg &/or DBP > 100 mmHg
- Re-evaluate within days – weeks (≤ 1 month), preferably with HBPM
C) > 180/110 mmHG
- Exclude hypertensive emergencies first.
- If excluded, consider prompt confirmation (≤ 1 week) prior to starting treatment.
Approach to newly diagnosed HTN
Evaluation should have 3 objectives, assessed through history, physical examination, lab investigations and other diagnostic tests:
- To exclude secondary cause of hypertension
- To ascertain the presence of target organ damage or complications
- To assess lifestyle & other CV risk factors or coexisting conditions that may affect prognosis & guide treatment.
Secondary cause of hypertension
The secondary causes of hypertension can be:
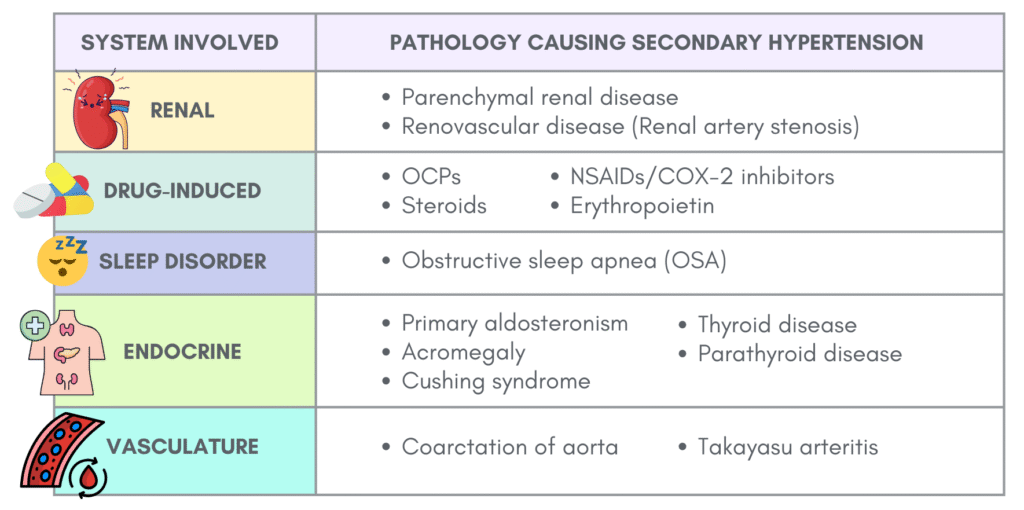
Regarding renovascular disease (renal artery stenosis)
Refers to a narrowing of the renal artery (usually by > 75%) that can result in a hemodynamically significant restriction of blood flow.
Atherosclerotic disease (90%) is the most common cause.
Nonatherosclerotic disease—most often fibromuscular dysplasia—is less common, typically affecting younger, otherwise healthy women.
Regarding primary aldosteronism
Excess aldosterone causes volume expansion, sodium retention, potassium loss, suppressed renin, hypertension, and cardio-renal damage.
Hypokalemia occurs in only 20–50% of primary aldosteronism cases—screening should not depend on potassium levels alone.
Causes of excess aldosterone:
- ~ 2/3: Bilateral adrenal hyperplasia
- ~ 1/3: Unilateral aldosterone overproduction (adenoma, less commonly unilateral hyperplasia, rarely carcinoma)
Suspect and investigate for secondary hypertension if there are features of:
- Treatment resistant hypertension or Stage 2 HTN (AHA guideline)
- Sudden or early onset (<30 years old) hypertension
- Worsening BP in well-controlled patients
- Diastolic HTN in older adults (≥ 65 years old)
- Target organ damage disproportionate to BP severity or duration
- Accelerated/Malignant HTN
- Unprovoked/excessive hypokalemia
- Insomnia or daytime sleepiness
- Concomitant adrenal nodule
- History of early-onset stroke (< 40 years old)
- Family h/o primary aldosteronism
Ascertain presence of Target Organ Damage (TOD) or complications (TOC)
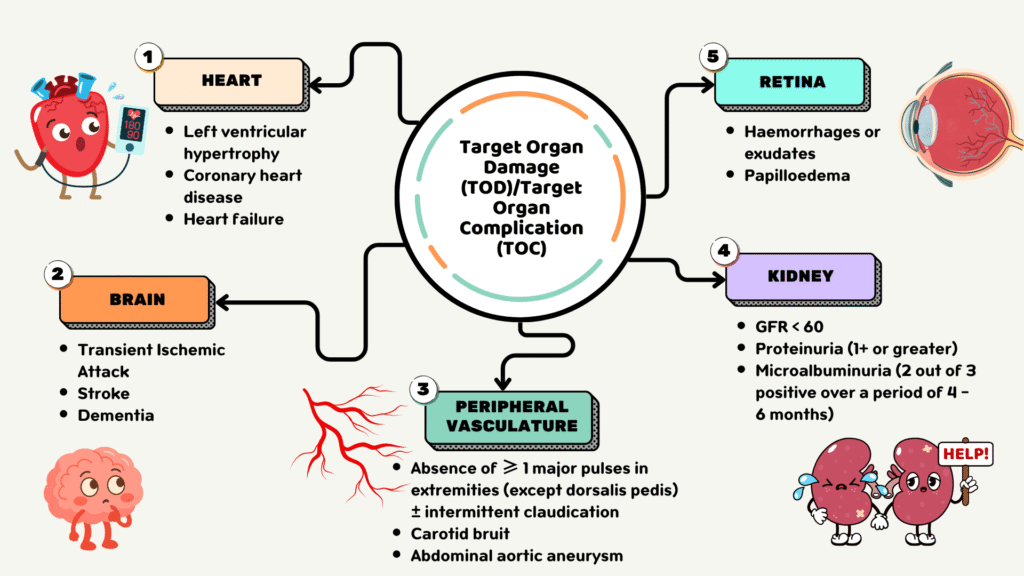
Target Organ Damage (TOD) = LVH, retinopathy, proteinuria
Target Organ Complication (TOC) = Heart failure, renal failure
Investigations 🔍
Initial investigations for newly diagnosed hypertension aims to screen for any secondary causes, determine presence of risk factors, TOD and TOC.
Basic tests should include:
- FBC
- Blood glucose or HbA1c
- Lipid profile
- Renal function tests – creatinine, eGFR, serum electrolytes
- Uric acid
- Urinalysis (dipstick: albuminuria/microalbuminuria & microscopic hematuria)
- ECG – can provide important information on subclinical CVD (e.g. LVH)
- TSH (if indicated)
Optional testing
Mainly for further CVD risk stratification & detection of target organ damage – particularly useful for those in the “Elevated BP” category.
These tests include:
- Cardiac biomarkers (eg, high-sensitivity troponin [hs-cTn], B-type natriuretic peptide [BNP])
- Echocardiography
- Coronary artery calcium may be helpful
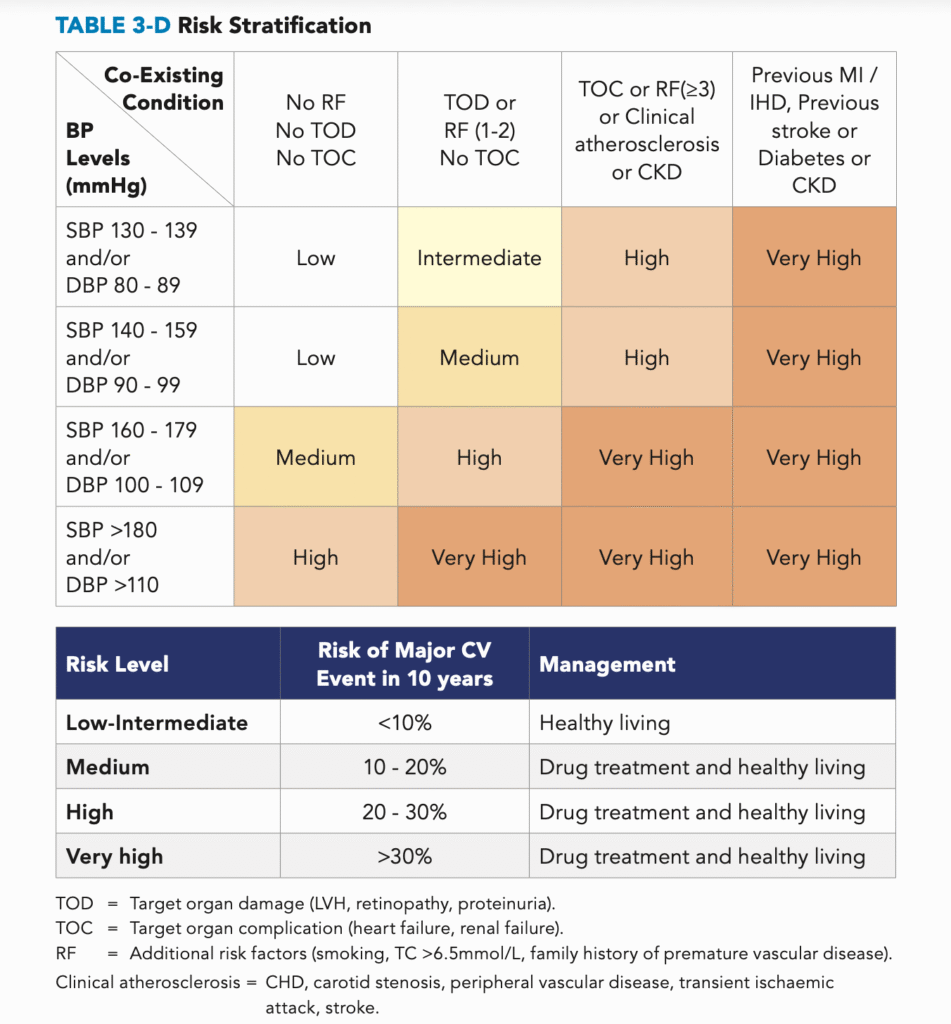
Risk stratification
Following initial clinical evaluation & investigations, the patient should be risk stratified to guide treatment.
Important co-existing CV risk factors that should be taken into consideration during risk stratification include:
- DM
- Dyslipidemia
- Cigarette smoking
- Microalbuminuria/proteinuria
- eGFR < 60
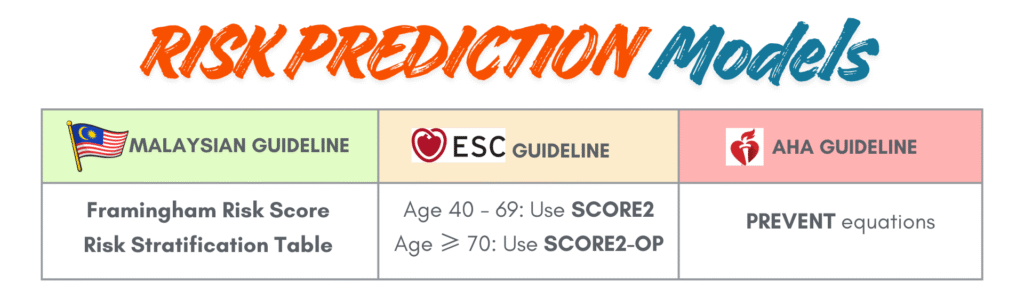
There are few tools available for risk stratification according to different guidelines.
Malaysia CPG recommends the use of either the Framingham General Cardiovascular Risk Score or the Risk Stratification Table.
In addition to the SCORE2 & SCORE2-OP, ESC guideline also recommends using the SCORE2-Diabetes to risk stratify diabetic patient with hypertension.
Risk Stratification Table
Non-pharmacological management
Lifestyle modifications should must be encouraged to all hypertensive patients regardless of their CV risks.
These include:
1. Weight reduction (especially if overweight/obese) – improves BP, glucose & lipid metabolism
- Target 5–10% loss of initial body weight or ≥3 kg/m² BMI reduction.
- There is evidence that showed a reduction of 1kg in weight relates to 1 mmHg reduction in SBP.
2. Heart-Healthy diet
- DASH (Dietary Approach to Stop Hypertension) or Mediterranean diet – rich in fruits, vegetables, whole grains, low-fat dairy; low in saturated fat
3. Reduce salt intake: ≤2 g/day (≈5 g salt or 1 tsp); ideal ≤1.5 g/day.
4. Increase dietary potassium intake – by taking diets rich in fruits & vegetables
- Aim 3.5 – 5 g/day (AHA guideline)
- For advanced CKD patients, restrict to < 2.4g/day. Consider monitoring for potassium levels if patients are on potassium-sparing medication, e.g. ACEi, ARBs, or spironolactone. (ESC guideline)
5. Physical activity & exercise
- Aerobic: ≥150 min/week moderate intensity or ≥75 min/week vigorous intensity.
- Resistance: 2–3 sessions/week.
– Dynamic: 2–3 sets of 10–15 reps at 40–60% 1 repetition maximum
– Isometric: 3 sets of 1–2 min (e.g., hand-grip, plank, wall sit). - Avoid high-intensity exercise if resting SBP >200 mmHg or DBP >110 mmHg.
6. Stress management – meditation, breathing exercises or yoga
7. Reduce alcohol consumption
- Even small doses of alcohol increases HTN risk.
- Aim for abstinence or ≤1 drink/day (women), ≤2 drinks/day (men); <100 g/week of pure alcohol.
8. Smoking cessation
💊Pharmacological treatment
Initiation of pharmacological treatment
- ESC & AHA guideline recommend to start pharmacological treatment for SBP ≥ 140/DBP ≥ 90 mmHg regardless of cardiovascular risks.
- In contrast, Malaysia guideline recommends for stage 1 (mild) HTN (SBP 140 – 159/DBP 90 – 99) with low CV risk, trial of non-pharmacological treatment can be started for 3 – 6 months before initiating pharmacological treatment. However, for those with moderate or high CV risk, immediate initiation of antihypertensive medications is recommended.
First line pharmacological agents
- ACE inhibitors (ACEi)/ARBs
- Calcium channel blockers (CCBs)
- Thiazides (HCTZ) and Thiazide-like diuretics (e.g. chlorthalidone & indapamide)
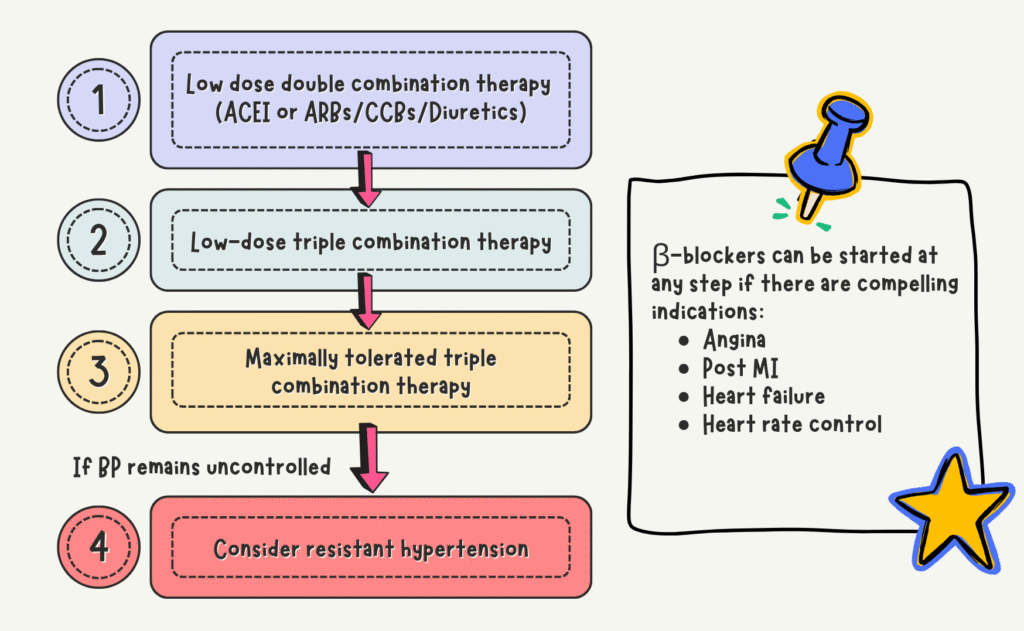
Regarding β-blockers
Not considered as first-line under ESC & AHA guidelines due to:
- Less effective than ACEi/ARBs/CCBs for stroke prevention
- ↑ Risk of new-onset diabetes when combined with diuretics (in predisposed patients)
Can be added if there are compelling indications: Angina, heart failure, post-MI, heart rate control.
Preferred β-blockers: 2nd gen (cardioselective) and especially 3rd gen (vasodilating).
Nevertheless, Malaysia guideline still consider β-blockers as part of first line and may be used in younger patients who are:
- Intolerant/contraindicated to start ACEi/ARBs
- Women of child-bearing potential
- Patients with evidence of increased sympathetic drive
Initial treatment strategy
Can be either :
a) Combination therapy – preferred ✅
Upfront low-dose combination therapy (using 2 first-line agents from different classes) is recommended for most patients except for a few which will be discussed below under monotherapy.
Avoid using ACEi + ARBs together
Single pill combination (SPC) is recommended to improve adherence.
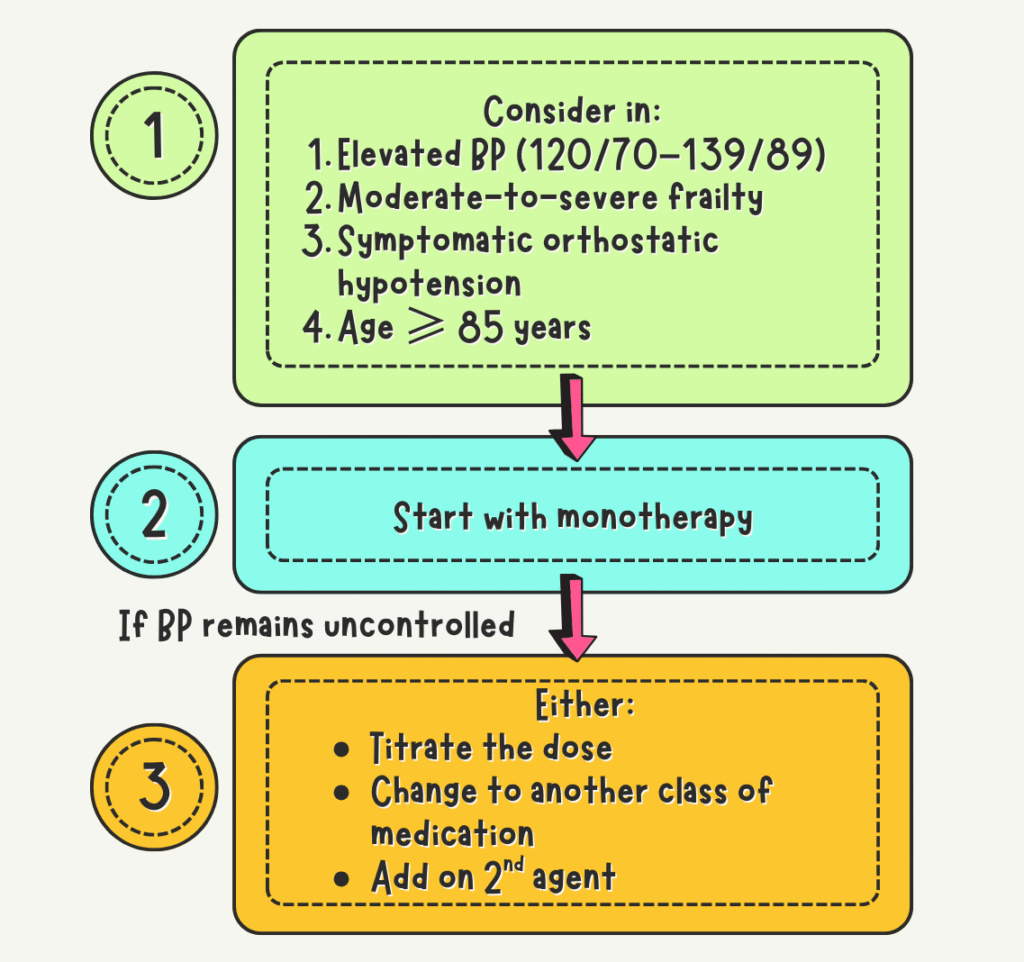
b) Monotherapy with stepped-care approach
This is preferred in:
- Elevated BP category (SBP 120 – 139/DBP 70 – 89)
- Moderate-to-severe frailty
- Symptomatic orthostatic hypotension
- Age ≥ 85 years old
Can also be considered for SBP 140 – 159/DBP 90 – 99 with low CV risk (Malaysia CPG)
Start with single agent, then either titrate the dose/change to another class of medication/add on a 2nd agent.
Stepped-care remains a reasonable option if well-executed.
Spironolactone
Effective add‑on for resistant HTN after first‑line optimization; use if eGFR ≥ 45
For patients with CKD stage ≥4, use chlorthalidone or loop diuretics instead (AHA guideline)
Others
Used only if all other therapies fail; caution due to adverse effects
These include:
- Alpha-blockers
- Hydralazine
- Minoxidil
- Other potassium-sparing diuretics
- Centrally acting agents
New therapies – awaiting more supporting evidence (ESC)
- Angiotensin receptor-neprilysin inhibitor (ARNi) sacubitril/valsartan
- SGLT2 inhibitors
- GLP-1 agonists
- New non-steroidal MRAs, e.g. finerenone
- Dual endothelin receptor antagonist – aprocitentan
- Zilebesiran – an investigational RNA interference agent administered subcutaneously –> inhibits hepatic angiotensinogen synthesis.
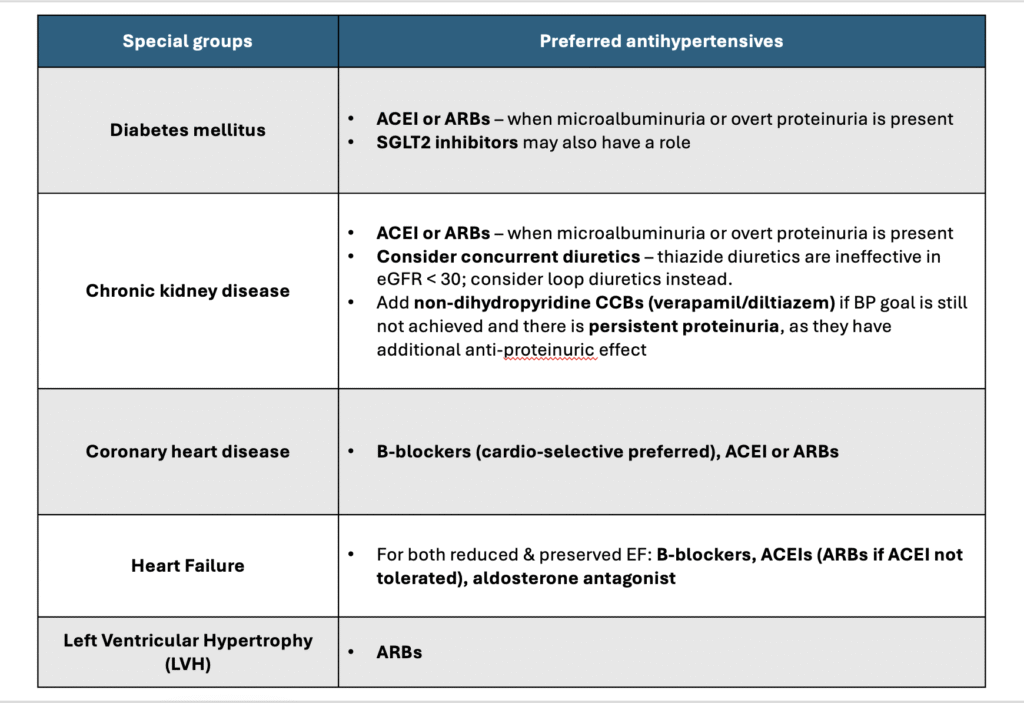
Preferred agents in special groups
🎯Target BP
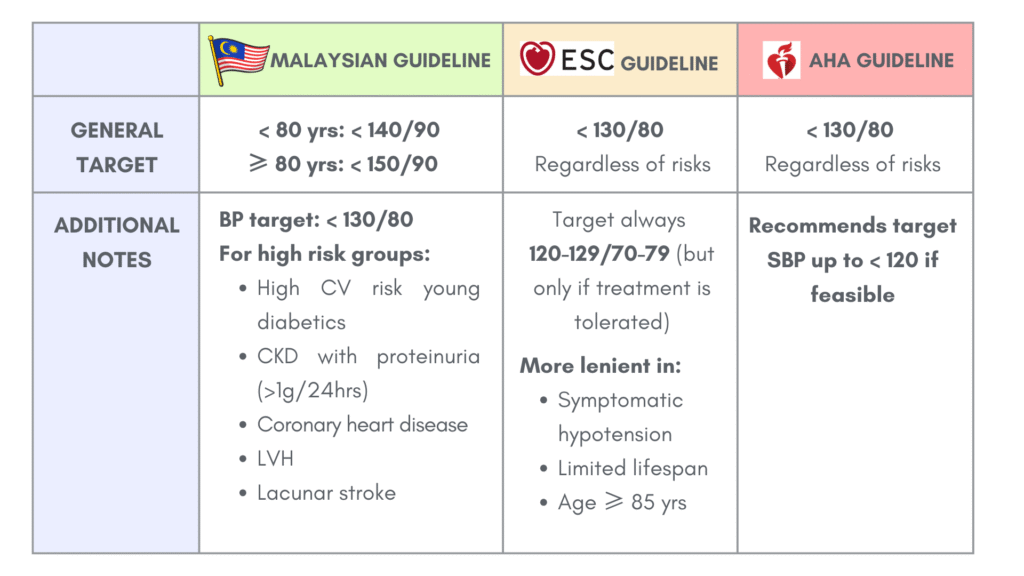
These are based on office BP.
The ESC & AHA guidelines aims for BP target of < 130/80 regardless of the CV risks. Nevertheless, individualization of BP target should be considered in those who are unable to tolerate treatment side effects, have limited life expectancy , or other clinical features that warrant a less intensive approach.
The Malaysia guideline on the other hand aims for < 140/90 (for < 80 yrs); < 150/90 (for ≥ 80 yrs); < 130/80 (for high risk groups)
Follow up
Achievement of target BP should be based on an average of ≥2 readings at ≥2 visits, not on an individual BP measurement.
The BP-lowering effect of the medications is typically evident within 1–2 weeks, but full response may take longer. Reassess after 1–3 months to evaluate treatment efficacy, tolerability, and safety.
During follow up, assess for:
- BP control
- Treatment adverse effects
- CV risks (including new-onset & pre-existing one)
- Complications of HTN.
For high & very high CV risk patients, aim to achieve target BP within 3 – 6 months.
Once target BP is achieved, follow up every 3 – 6 months (at least twice yearly – bare minimum)
Avoid repeat prescriptions without clinical review.
Resistant hypertension
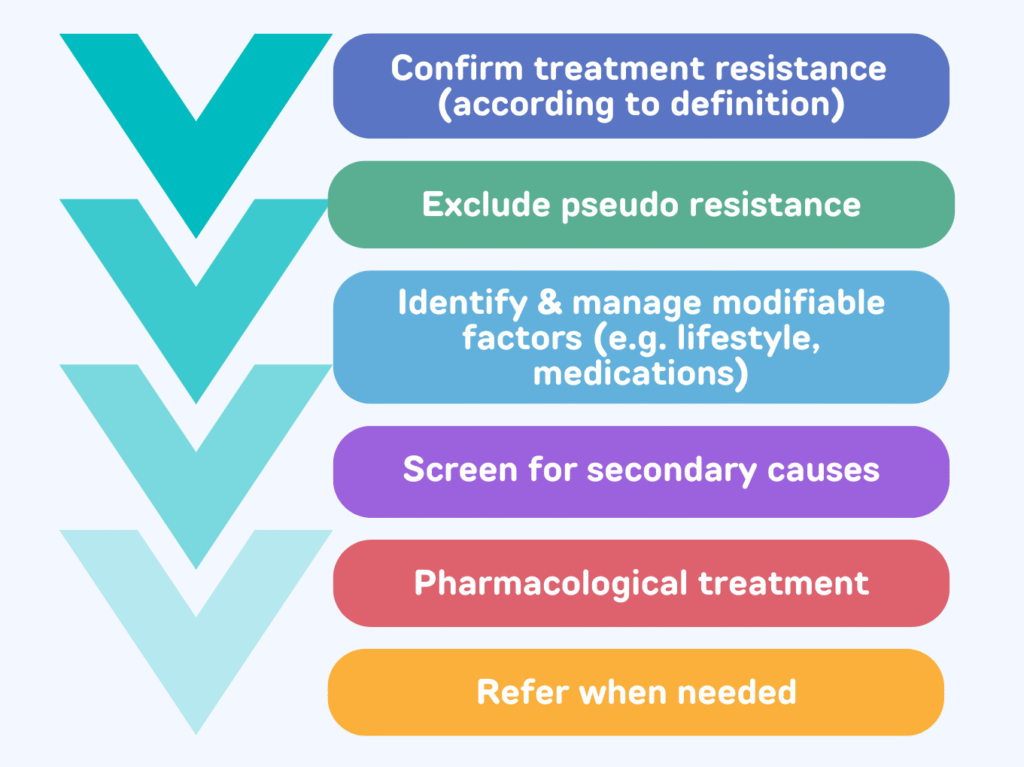
General approach to resistant hypertension
Defined as (AHA guideline):
- Target BP not achieved despite on maximally tolerated dose of ≥ 3 antihypertensives (ACEi or ARB + CCB + Thiazide-like diuretics)
- Target BP achieved but require ≥ 4 medications (ACEi or ARB + CCB + Thiazide-like diuretics + additional medications)
Common causes:
- Behavioral factors – overweight/obesity, physical inactivity, excess daily dietary sodium, excess habitual alcohol consumption
- Drug-induced
- Undetected secondary hypertension (more likely to be present in resistant HTN)
Before diagnosing resistant hypertension, pseudo-resistant must be ruled out first.
Causes of pseudo-resistant include:
- Poor adherence to treatment
- White-coat phenomenon (Confirmation with HBPM plays an important role)
- Poor BP measurement method
- Marked brachial artery calcification (Osler phenomenon)
- Clinician inertia – inadequate doses, inappropriate combinations of BP-lowering drugs.
- Munchausen syndrome (rare)
Pharmacological treatment
Maximize diuretics – replace thiazide-type diuretics with chlorthalidone or indapamide.
Add spironolactone or equivalent dosage of eplerenone if eGFR ≥ 45
Use chlorthalidone or loop diuretics in CKD stage ≥4
Add agents with different MOA – Beta blockers, central sympatholytic drugs or nondihydropyridine CCB for elevated heart rate.
Add dual endothelin-receptor antagonist (e.g. aprocitentan) or vasodilators (e.g. hydralazine or minoxidil, only if already on beta blocker or loop diuretics)
Referral
For suspected or known case of secondary hypertension
If BP remains uncontrolled >6 months of treatment.
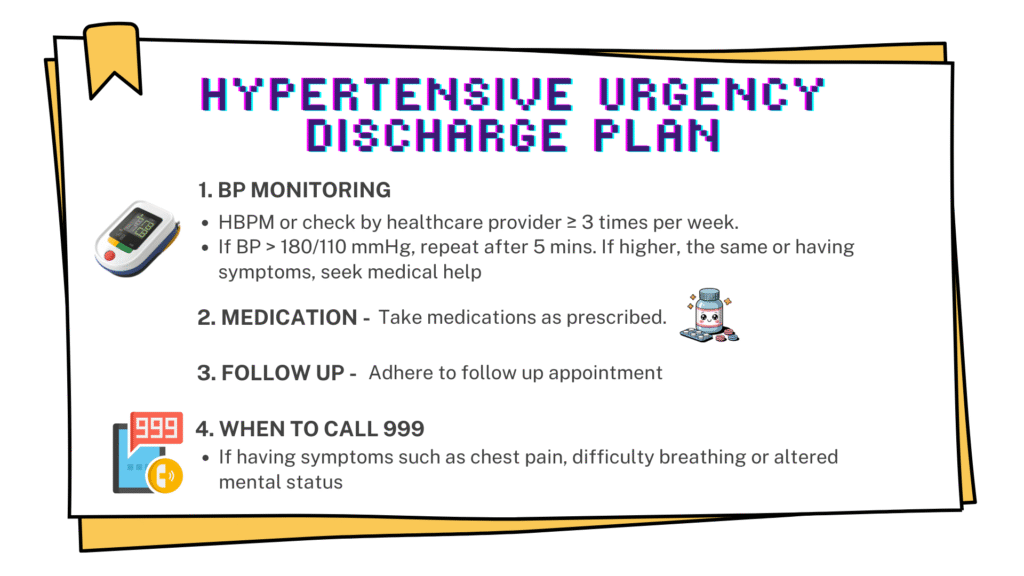
Severe hypertension (≥180/110) without target organ damage/complications
Also known as “hypertensive urgency”.
Management
ESC & AHA (Similar Recommendations)
- No aggressive BP lowering and no IV antihypertensives.
- Manage as outpatient by:
– Restarting or adjusting oral medications &
– Early follow-up to ensure BP control
Malaysia CPG (more structured on-site protocol)
- Rest in quiet room & observe — check BP every 30 min for 2 hours
– If BP decreases → discharge with meds + urgency plan
– If no improvement → start meds (captopril / nifedipine / labetalol) & Monitor every 30 min for 1 hour
– If still no improvement → admit or refer for further care
Hypertensive emergency is not discussed here & may be included in another post.
What about SBP 120 – 139/DBP 70 – 89?
Although the ESC & AHA guidelines categorize this BP range differently, but the treatment approach is similar.
Decision for BP-lowering therapy is based on:
1. Are there high-risk comorbidities ? If yes –> treat
These include:
- Moderate/Severe CKD
- Established CVD (CAD, stroke, PAD, HF)
- Hypertension-mediated organ damage
- Diabetes Mellitus (ESC recommend to use SCORE2-diabetes to guide decision)
- Familial hypercholesterolemia
2. No high-risk comorbidities ? –> Calculate 10-Year CVD risk (Framingham/SCORE2/PREVENT). If significant, start treatment.
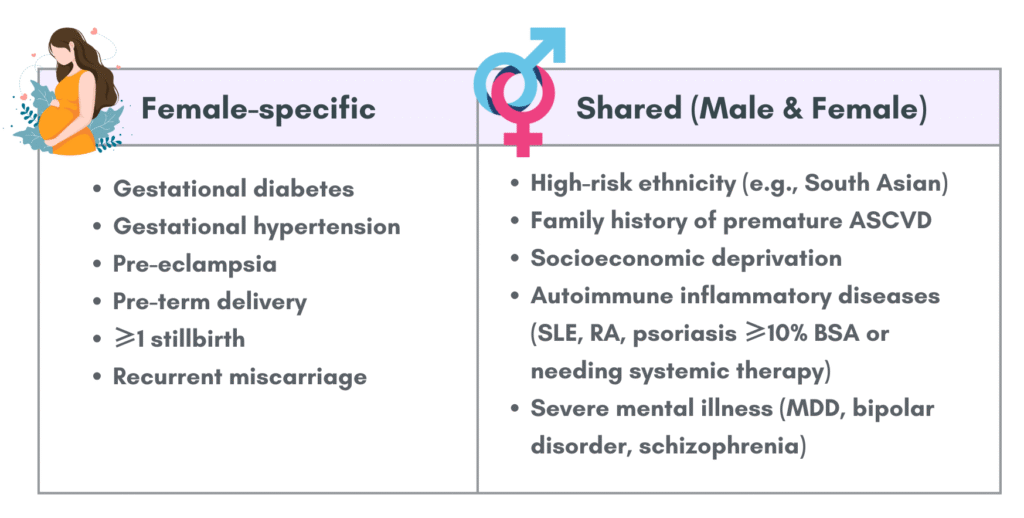
3. If borderline 10-Year CVD risk –> Consider these non-traditional risk factors that may up-classify the patient to high risk.
4. Still uncertain ? –> Use additional risk-stratifying tests, which include:
- Coronary artery calcium scores
- Cardiac biomarkers – high-sensitivity troponin, B-type natriuretic peptide (If elevated, may represent markers of HMOD)
- Carotid or femoral plaque
- Arterial stiffness
Where BP-lowering therapy is indicated in the elevated BP group with CVD risk
Start with lifestyle measures to reduce BP first.
After 3 months of lifestyle measures, consider starting pharmacological treatments if BP remains ≥ 130/80 mmHg.
Aim BP 120 – 129/70 -79
Exercise caution when considering treating persons with elevated BP and :
- Moderate-to-severe frailty
- Symptomatic orthostatic hypotension
- Age ≥ 85 years
References
- Writing Committee Members*, Jones, D. W., Ferdinand, K. C., Taler, S. J., Johnson, H. M., Shimbo, D., Abdalla, M., Altieri, M. M., Bansal, N., Bello, N. A., Bress, A. P., Carter, J., Cohen, J. B., Collins, K. J., Commodore-Mensah, Y., Davis, L. L., Egan, B., Khan, S. S., Lloyd-Jones, D. M., Melnyk, B. M., … Williamson, J. D. (2025). 2025 AHA/ACC/AANP/AAPA/ABC/ACCP/ACPM/AGS/AMA/ASPC/NMA/PCNA/SGIM Guideline for the Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Hypertension (Dallas, Tex. : 1979), 82(10), e212–e316. https://doi.org/10.1161/HYP.0000000000000249
- McEvoy, J. W., McCarthy, C. P., Bruno, R. M., Brouwers, S., Canavan, M. D., Ceconi, C., Christodorescu, R. M., Daskalopoulou, S. S., Ferro, C. J., Gerdts, E., Hanssen, H., Harris, J., Lauder, L., McManus, R. J., Molloy, G. J., Rahimi, K., Regitz-Zagrosek, V., Rossi, G. P., Sandset, E. C., Scheenaerts, B., … ESC Scientific Document Group (2024). 2024 ESC Guidelines for the management of elevated blood pressure and hypertension. European heart journal, 45(38), 3912–4018. https://doi.org/10.1093/eurheartj/ehae178
- Ministry of Health Malaysia. (2018). Clinical Practice Guidelines: Management of Hypertension (5th ed.). Ministry of Health Malaysia
