Cellulitis and Erysipelas
Cellulitis and Erysipelas
Cellulitis
Causative agents
The most common causative agent is Group A beta hemolytic streptococci (though groups B, C, F or G can also cause cellulitis)
Staph. aureus is less common, & is usually associated with an open wound, previous penetrating trauma and sites of illicit drug injection.
Other circumstances (Cellulitis – stat pearl):
- Animal bites – Pasteurella multocida
- Water immersion injuries – VIbrio vulnificus
- Diabetic patients – Pseudomonas aeruginosa
- Immunocompromised patients – Pseudomonas aeruginosa, Cryptococcus
Risk factors
Breakdown in skin barriers – injuries, surgical incision, insect/animal bites, IV site puncture, fissures between toes
Comorbidities – DM, venous insufficiency, peripheral arterial disease, lymphedema, immune deficiency/compromise
Clinical presentation
Cardinal signs of inflammation: pain, erythema, swelling, warmth
With or without systemic inflammatory response syndrome (SIRS) – fever, tachycardia, tachypnea, abnormal white cell count.
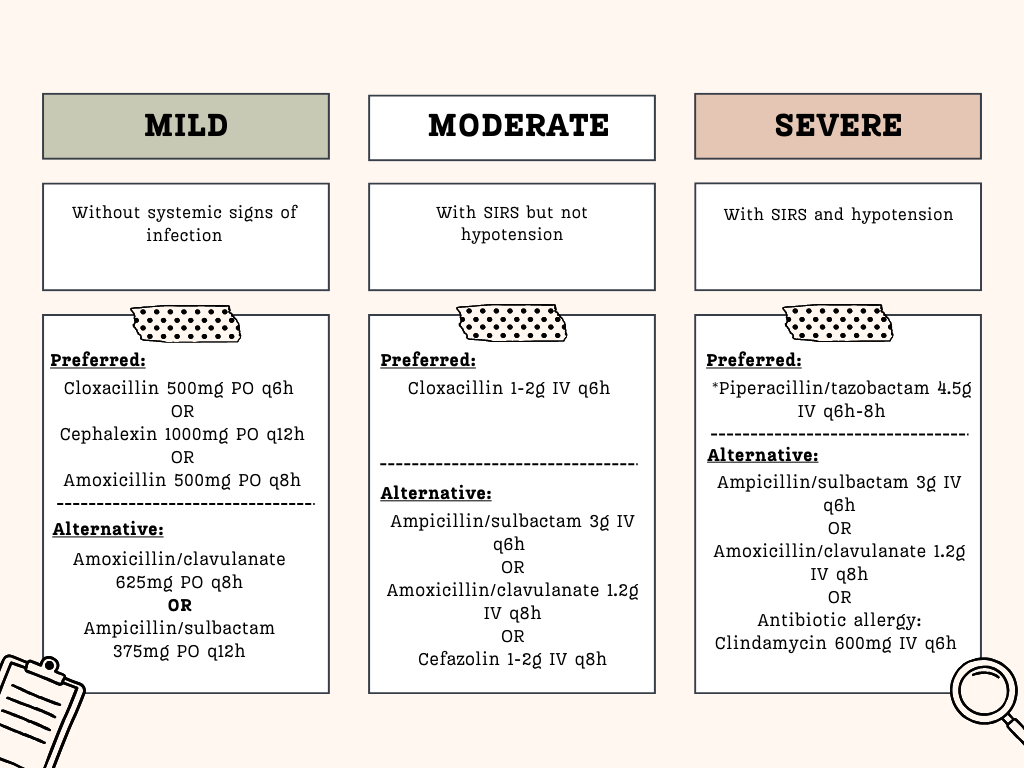
Classification of severity (Malaysia NAG):
- Mild – without systemic signs of infection
- Moderate – with SIRS but no hypotension
- Severe – with SIRS and hypotension
Workup
Generally not required in uncomplicated cases.
Blood cultures should be done in the following circumstances:
- Moderate to severe disease
- Cellulitis of specific anatomic sites (face/ocular involvement)
- Pt with malignancy who are receiving chemotherapy
- Neutropenia or severe cell-mediated immunodeficiency
- Animal bites
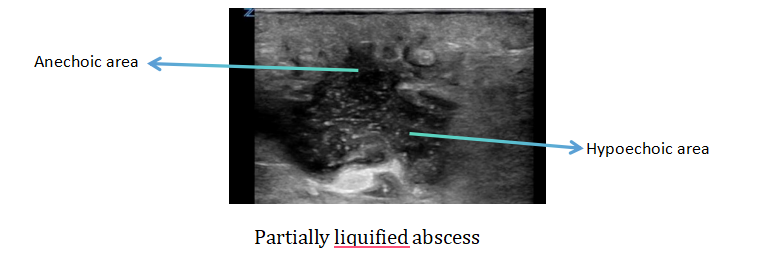
USG may be useful to detect any occult abscess
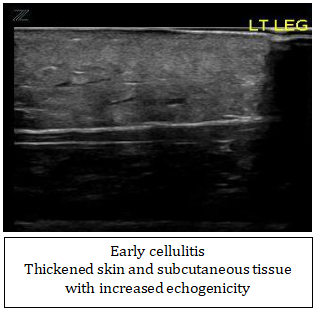
Some USG findings on cellulitis (Best assessed with linear probe)
Early changes: Thickened, hyperechoic skin and subcutaneous tissue
Later: “Cobblestone” appearance – Hyperechoic fat lobules separated by anechoic fluid-filled areas (Note that “cobblestone appearance may also be seen in fluid overload conditions, e.g. heart failure, renal failure, etc.)
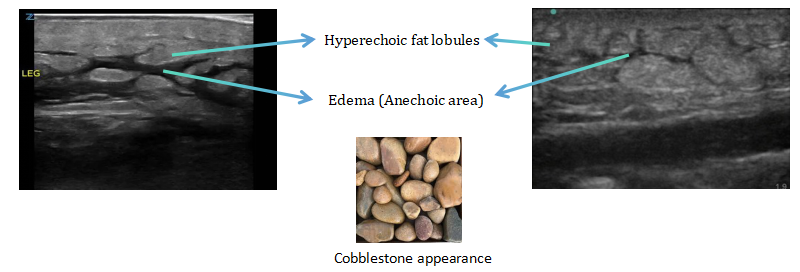
Lookout for any abscess among the “cobblestone” especially if clinically suspicious (e.g. septic looking, pain out of proportion, worsening cellulitis etc)
Side note: If you are interested in further exploring the application of USG in primary care settings, you may consider getting this ebook which covers mainly on USG HBS and KUB and also some other common conditions encountered in primary care =) [USG at the Point of Care – Focusing on HBS & KUB].
Management
In lower limb cellulitis, treat also fissuring, scaling or maceration if present in the interdigital toe spaces to eradicate pathogen colonization, which reduces risk of recurrent infection (IDSA guideline).
MRSA
MRSA is an unusual cause of cellulitis.
Coverage of MRSA can be considered in conditions like:
- Infection at site of illicit drug injection
- Purulent drainage
- Concurrent MRSA infection elsewhere in the body
Treatment options for MRSA
- IV – vancomycin, daptomycin, linezolid or telavacin.
- Oral therapy – doxycycline (100 mg BD), clindamycin (300 mg PO 6 hrly), or Trimethorpim/sulfamethoxazole [SMX-TMP] 160/800 mg BD [NAG]
- If oral therapy is required for coverage of both MRSA & streptococci, consider – clindamycin alone, or combination of beta lactam (e.g. penicillin, cephalexin or amoxicillin) with doxycycline or SMX-TMP.
[Commonly used amoxicillin/Augmentin are effective against MSSA, but less so against MRSA]
For recurrent cellulitis (IDSA)
Identify and treat predisposing conditions e.g. oedema, obesity, venous insufficiency, eczema, toe web abnormalities (including tinea pedis).
If still having 3 to 4 ep. of recurrent cellulitis despite controlling the predisposing conditions, consider starting:
- Oral penicillin – Phenoxymethylpenicillin (Penicillin V) 250mg PO q12h (500mg PO q12h if BMI ≥ 33) OR
- If penicillin allergy: consider starting Clarithromycin 250mg PO q24h OR Erythromycin ethylsuccinate 400mg PO q12h
Antibiotic prophylaxis can be continued for 1 year and then reassess to decide whether further prophylaxis are needed(NAG). Treatment may be continued as long as the predisposing factors persist (IDSA).
Erysipelas
Share many similarities with cellulitis, including the causative agents and risk factors.
Mainly caused by group A beta hemolytic streptococcus (Streptococcus pyogenes), less commonly Staph aureus, Strep pneumoniae, Klebsiella pneumoniae, Yersinia enterocolitica, and Haemophilus influenza.
Common site of involvement: the lower limbs, secondly followed by the face.

Erysipelas vs Cellulitis
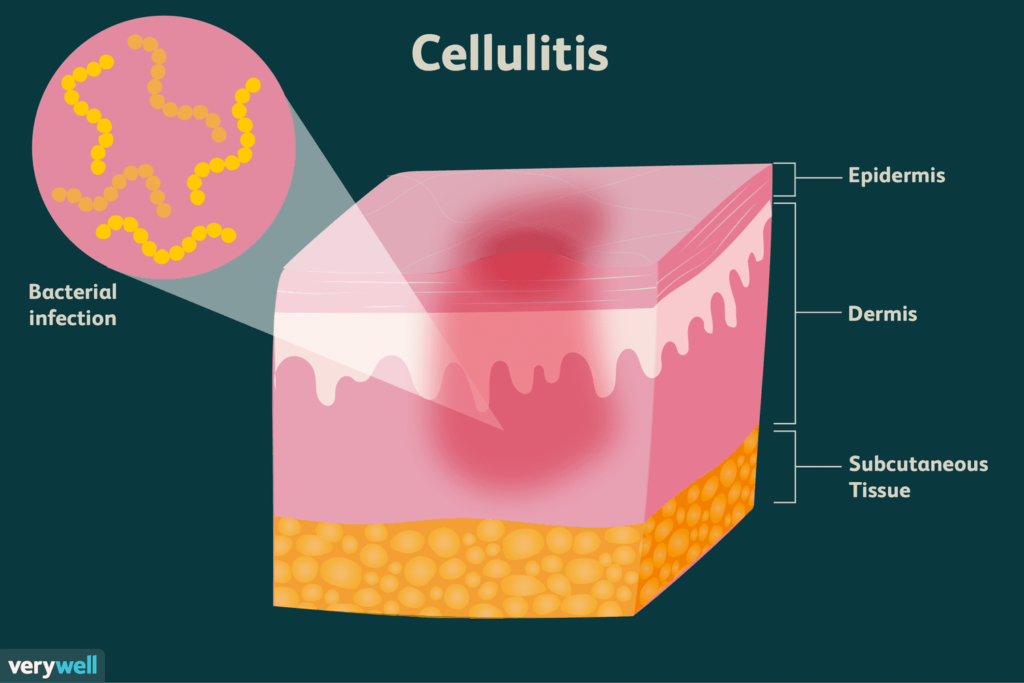
They are both bacterial skin infection, where erysipelas mainly involves the superficial dermis and possibly the superficial lymphatics, and cellulitis involves the deeper dermis and may extend up to the subcutaneous tissue.
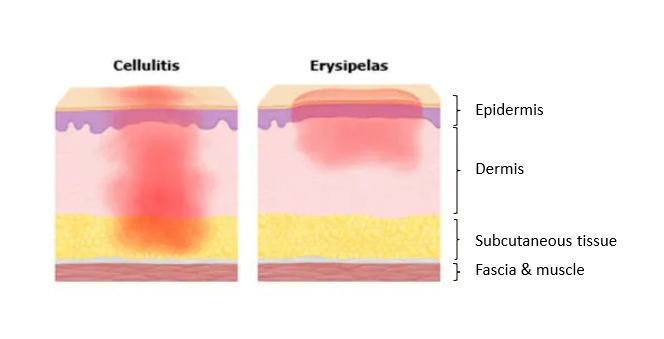
In terms of clinical presentation, both manifest with the cardinal signs of inflammation, where the difference lies in for erysipelas the area involved appears demarcated as compared to cellulitis which appears more ill-defined.


Image obtained from Dermatology Atlas (http://www.atlasdermatologico.com.br/disease.jsf?diseaseId=132).
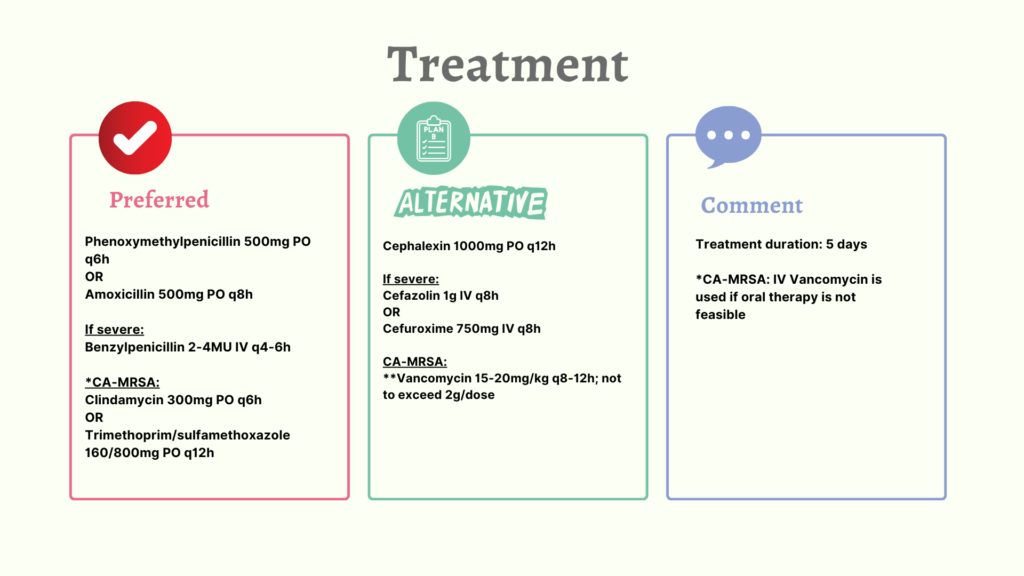
Management of erysipelas (NAG)
References
- Pharmaceutical Services Programme, Ministry of Health Malaysia. (2024). National antimicrobial guideline (NAG) 2024(4th ed.)
- Stevens, D. L., Bisno, A. L., Chambers, H. F., Dellinger, E. P., Goldstein, E. J., Gorbach, S. L., Hirschmann, J. V., Kaplan, S. L., Montoya, J. G., Wade, J. C., & Infectious Diseases Society of America (2014). Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America, 59(2), e10–e52. https://doi.org/10.1093/cid/ciu444
