Asthma
Special groups
1. Pregnancy & Breastfeeding 🤰
Newly diagnosed case may be based on clinical history that are consistent with asthma & there are no alternative diagnosis found.
Treatment can be started during pregnancy, with confirmatory tests deferred until after delivery.
GINA questionnaire & ACT are useful for assessing and monitoring asthma control.
Risk factor for asthma exacerbation in pregnancy include:
- Severe asthma
- Multiparity
- Black ethnicity
- Depression & anxiety
- Current smoking
- Age > 35 years
- Obesity
Poor symptom control and exacerbations are linked to adverse outcomes for both mother (maternal pre-eclampsia) and baby (pre-term delivery, low birth weight, increased perinatal mortality).
During pregnancy, patients with asthma should be monitored every 4 – 6 weeks.
Treatment:
- Same as non-pregnant patients for both during stable state & exacerbations.
- ICS is safe & should be initiated & continued if already being used.
- Inhaled B2-agonists & LTRA are safe
- OCS can be used in exacerbation when needed.
- Step-down treatment should be deferred until after delivery
Management of acute exacerbation: Treat aggressively with SABA, oxygen, & early administration of systemic corticosteroids – to prevent fetal hypoxia.
Regarding breastfeeding
Asthma patients should be encouraged to continue their asthma medications during breastfeeding
Occupational asthma
All working-age adults with new or worsening asthma symptoms, reappearance of childhood asthma or unexplained airflow obstruction should be asked about their occupation.
Diagnosis:
- PEFR (to diagnose & monitor) – A variability of ≥ 20% on workdays compared to off days is suggestive of work-related asthma.
- Other diagnostic modalities – specific IgE assays, skin prick test & specific inhalation challenge tests
Treatment include: Identification of occupational sensitizers, work relocation or hazard substitution.
Patient with suspected occupational asthma should be referred to a specialist for further evaluation – economic & legal implications
Confirmed cases should be notified using WEHU-L1 (JKKP7) form to the Department of Occupational Safety & Health.
Exercise-Induced Bronchoconstriction (EIB) 🏃♂️🚴♀️🏊♀️
Definition: acute, transient & reversible airway narrowing that occurs during or after exercise.
Diagnosis is based on:
- Typical clinical symptoms AND
- Demonstration of reversible airflow limitation, via exercise or surrogate challenges (e.g. bronchoprovocation test like mannitol challenge) – Post-exercise fall in FEV1 of > 10% measured 30 mins after exercise cessation.
Patients with well-controlled EIB can exercise safely with proper management, including
- Gradual warm-up prior to exercise.
- Use of SABA or ICS-SABA as reliever PRN prior to exercise with regular daily ICS regimen to help reduce EIB.
Asthma-COPD
Cough and wheezing are common features in both Asthma and COPD, and often times it can be hard to differentiate between the two. Nevertheless, effort should be made to come to the correct diagnosis as the management for both are different.
The table below provides some clues in differentiating Asthma, COPD and also Asthma-COPD overlap.
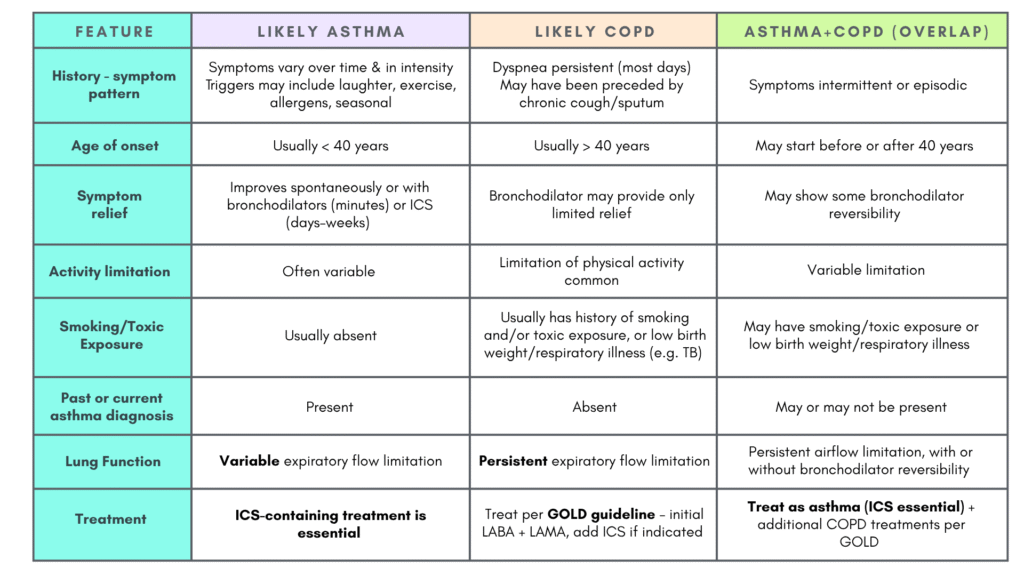
General treatment advice in addition to the above mentioned treatment for Asthma/COPD/Asthma + COPD (overlap):
- Treatment of modifiable risk factors including advice about smoking cessation.
- Treatment of comorbidities
- Non-pharmacological strategies including physical activity, & for COPD or asthma-COPD overlap, pulmonary rehabilitation & vaccinations
- Appropriate self-management strategies
- Regular follow-up
Referral
Indications for referral include:
- Persistent symptoms &/or exacerbations despite treatment
- Diagnostic uncertainty
- Atypical or additions SSx e.g. hemoptysis, significant weight loss, night sweats, fever, signs of bronchiectasis, or other structural lung disease – requires prompt early referral
- When chronic airways disease is suspected but syndromic features of either asthma or COPD are few.
- Patients with comorbidities that may interfere with the assessment & management of their airway disease, especially cardiovascular disease.
Summary
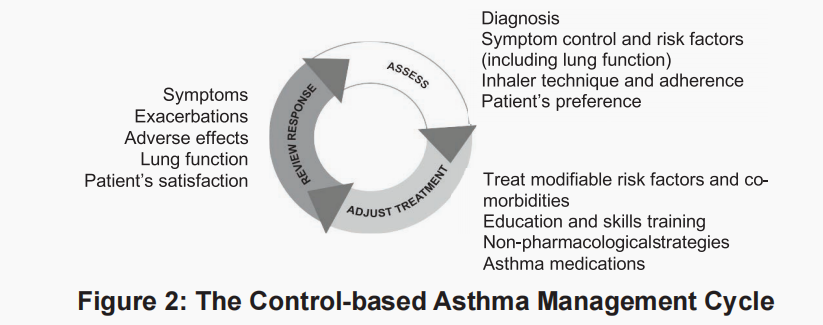
This asthma management cycle (GINA guideline) generally sums up all the important points while managing an asthma patient, which include:
- Assess
- Adjust treatment
- Review response
Topics that can be included in asthma education are:
- Asthma diagnosis
- Rationale for treatment, and differences between reliever & maintenance treatment (if prescribed)
- Potential side-effects of medication
- Prevention of symptoms & flare-ups: Importance of anti-inflammatory treatment
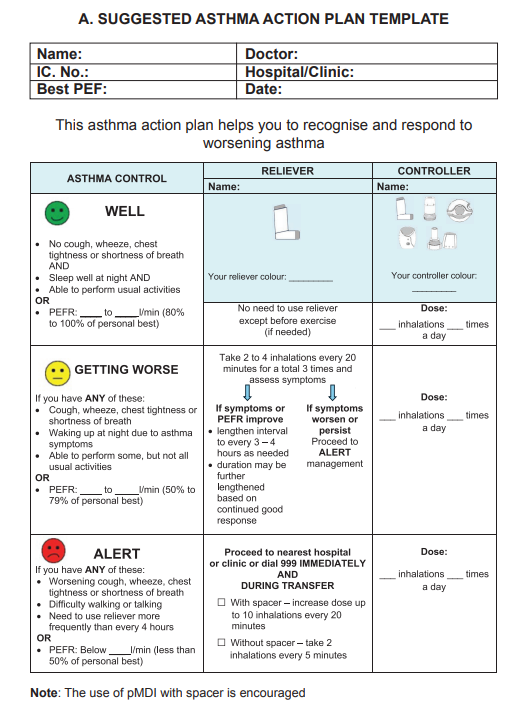
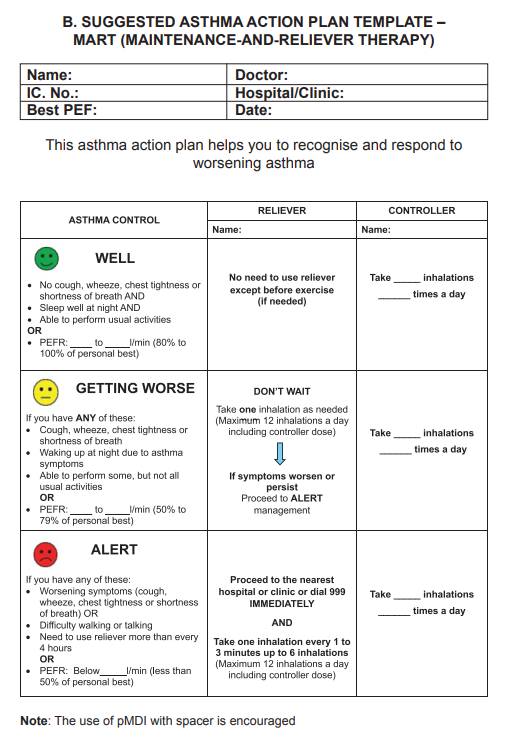
- How to recognize worsening asthma & what actions to take; how and when to seek medical attention (Asthma Action Plan)
- Management of comorbidities
Asthma Action Plan
Our Malaysia CPG guideline has done an excellent job in providing a well-prepared suggested asthma action plan template tailored to patients on either MART therapy or separate reliever and controller regimens.
References
- Malaysian Health Technology Assessment Section (MaHTAS), Medical Development Division, Ministry of Health Malaysia. (2024). Management of asthma in adults (2nd ed.). Putrajaya, Malaysia: Ministry of Health Malaysia. https://www2.moh.gov.my/moh/resources/Penerbitan/CPG/Respiratory/e-CPG_Management_of_Asthma_in_Adults_%28Second_Edition%29_-_11_4_25.pdf
- Global Initiative for Asthma. (2024). Global strategy for asthma management and prevention (2024 update)
