Asthma
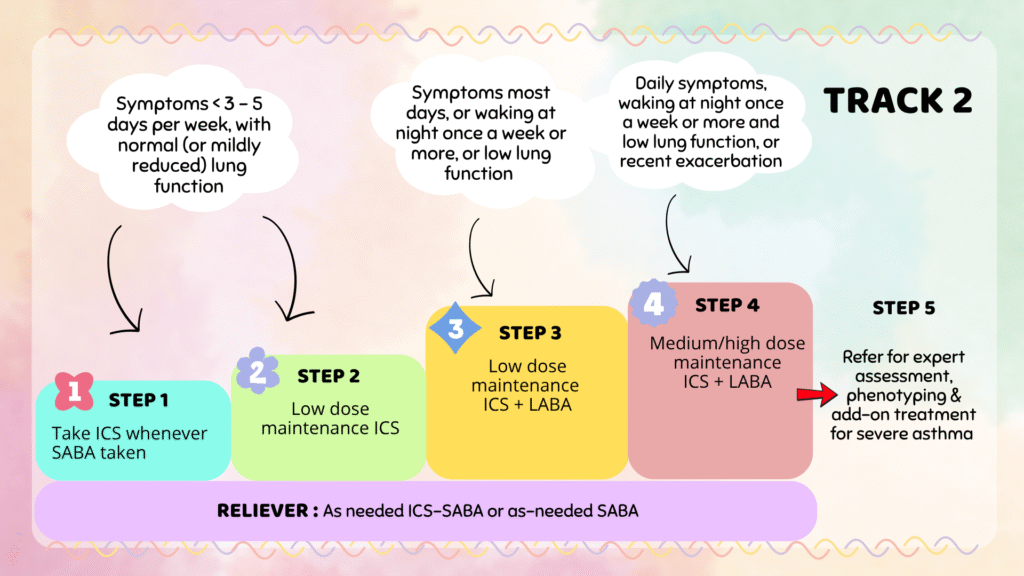
Initiating treatment, stepping up & stepping down
Included here are both from our CPG guideline & GINA guideline. You may consider following either one that you are more familiar or comfortable with.
Both advocate the same principle of including ICS treatment in all asthma patients. The difference is that GINA guideline has 2 track whereas our CPG guidelines don’t, instead it is presented as an algorithm.
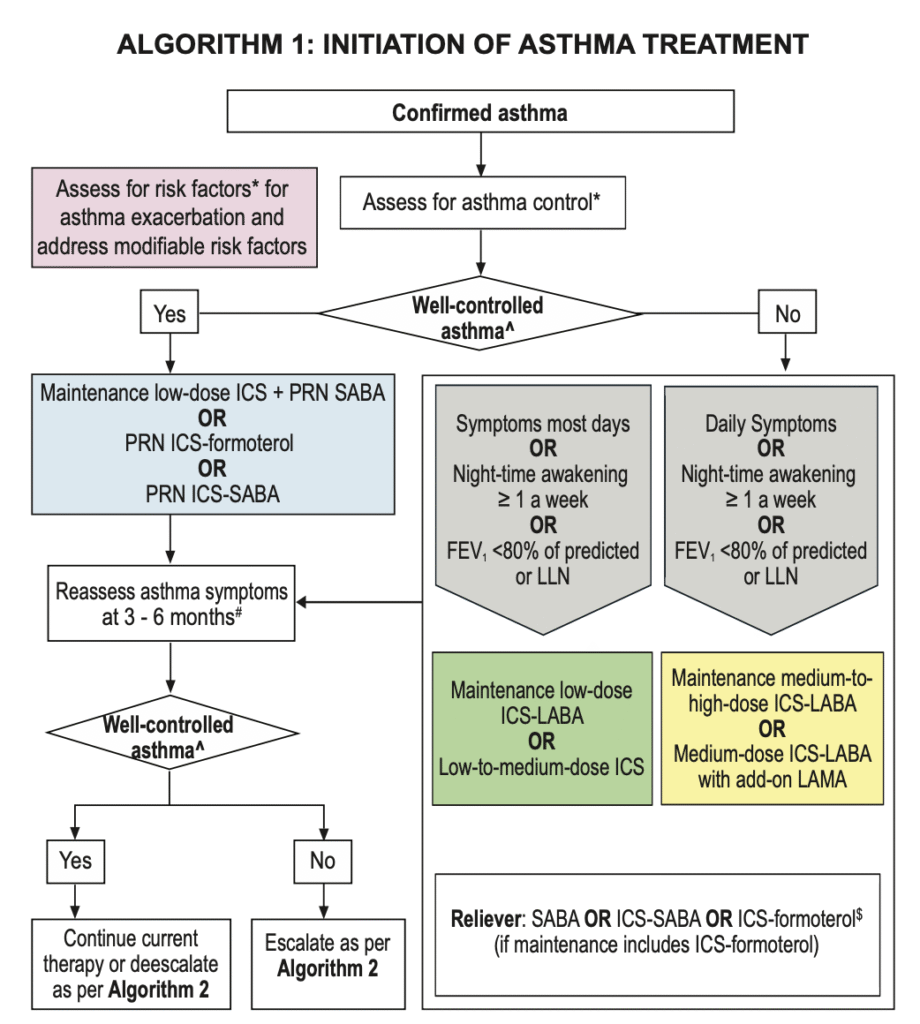
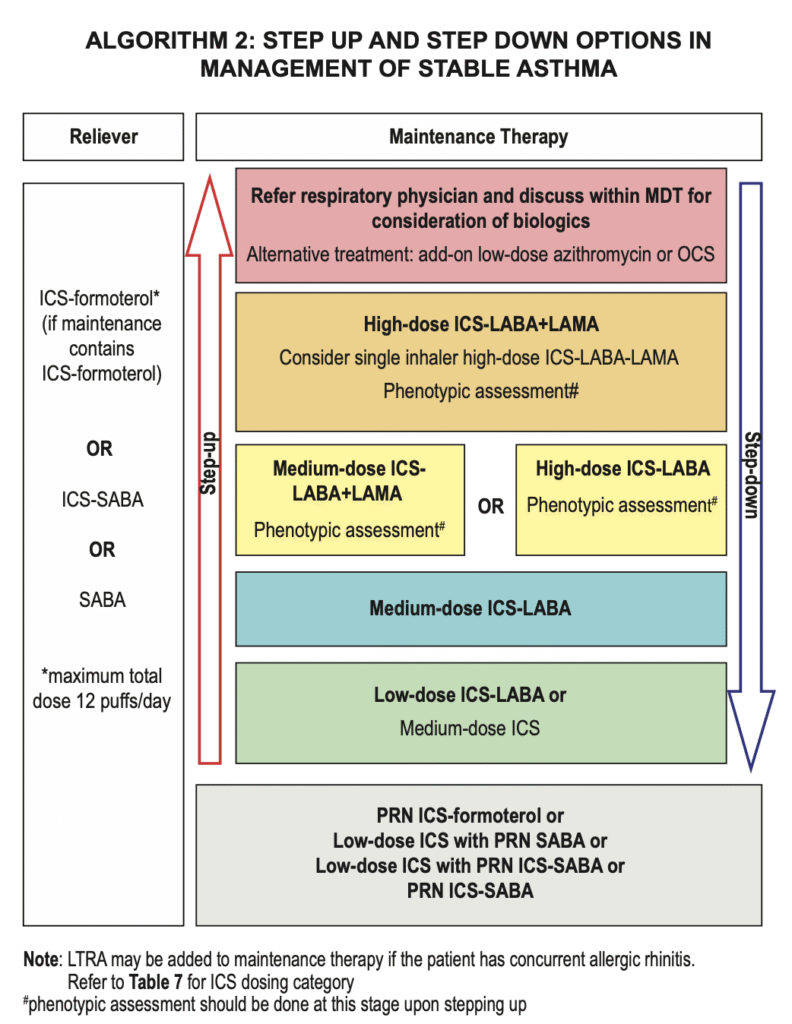
Malaysia CPG guideline
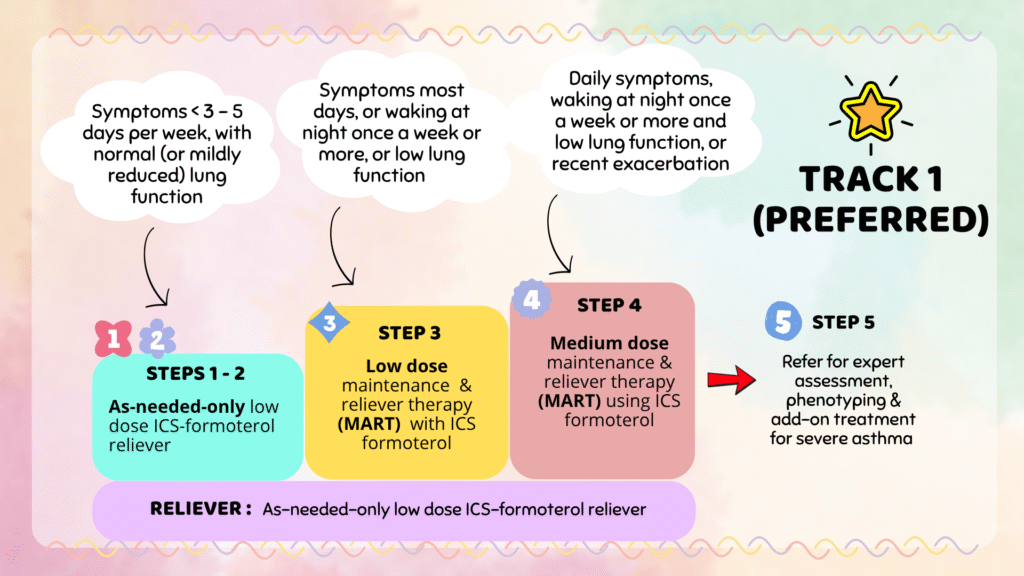
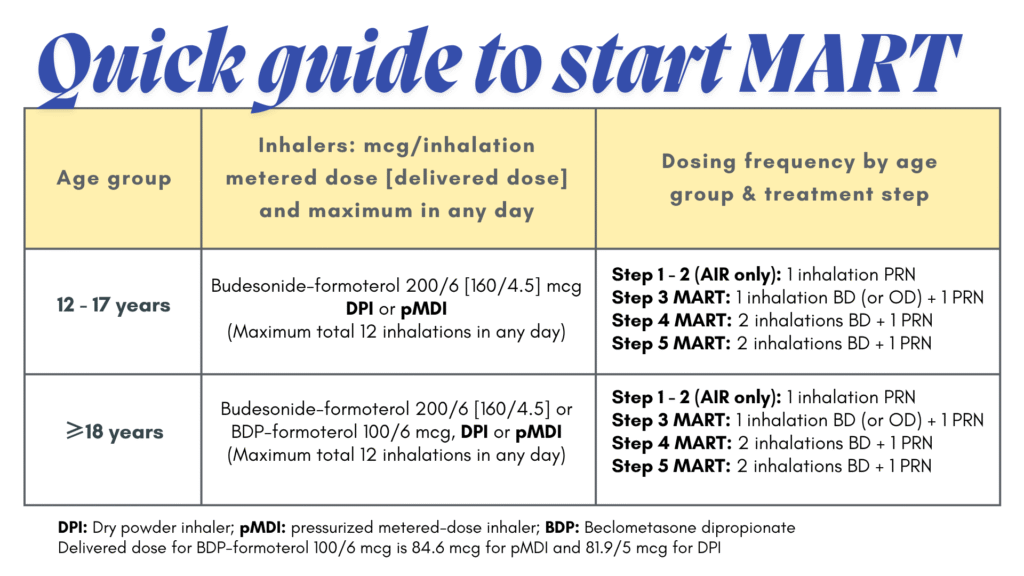
GINA guideline
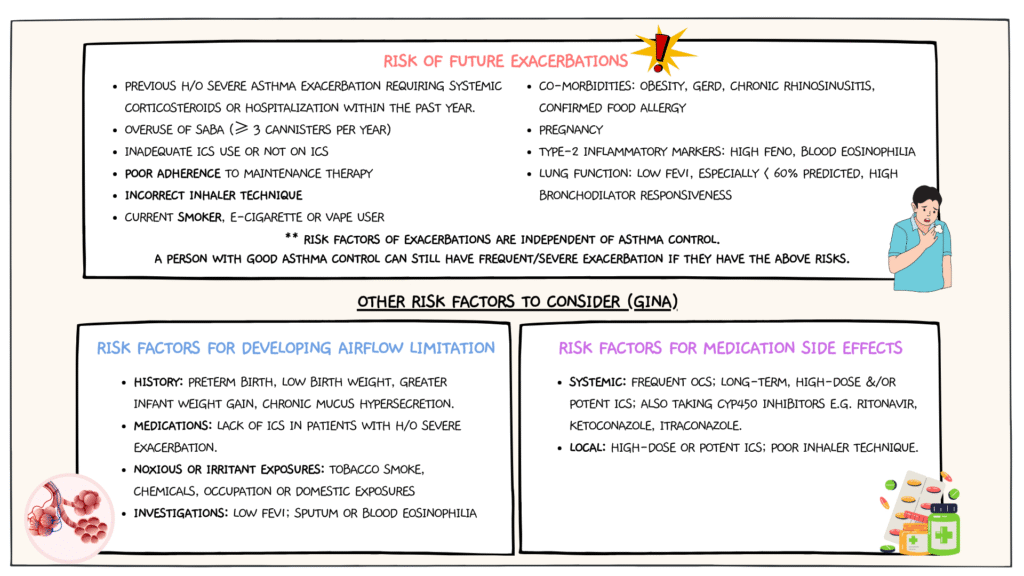
Assessment of asthma on follow up
Should include:
- Symptom control using GINA questionnaire or ACT score
- Risk of future exacerbation (covered in more detail below)
- Adherence to current therapy (insufficient use of ICS & over-reliance of SABA)
- Inhaler techniques
- Lung function – FEV1
- FeNO (if available)
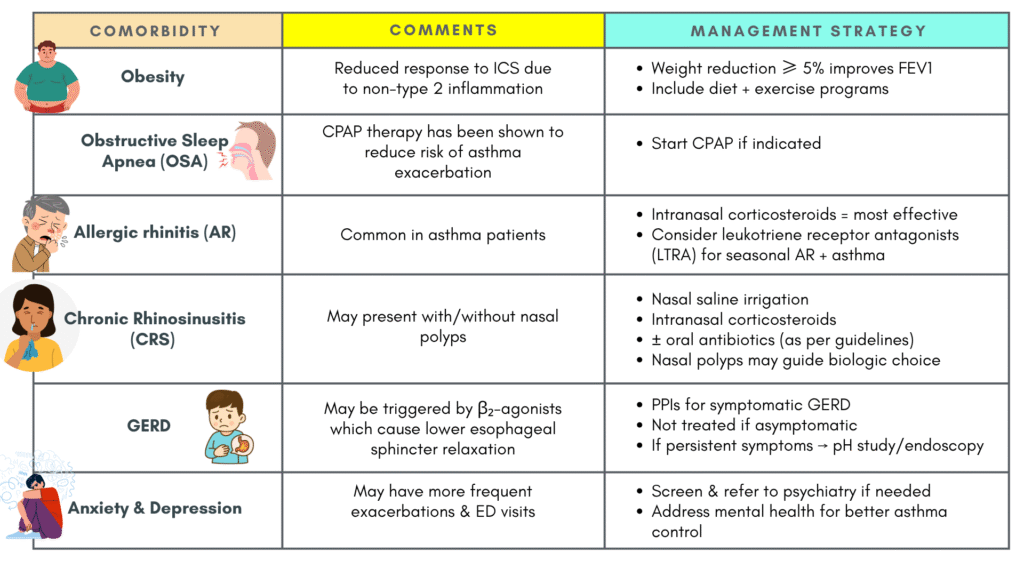
- Other medical conditions that can contribute to symptoms, poor QoL & sometimes poor asthma control, e.g. allergic rhinitis, GERD, rhinosinusitis, obesity, OSA, depression & anxiety
Factors contributing to poor adherence
Poor adherence to prescribed treatment is often one of the causes of poor asthma control.
Always explore & try to address the factors contributing to poor adherence, which may include:
A) Medication/regimen factors
- Difficulties using inhaler device (e.g. arthritis)
- Burdensome regimen (several times per day)
- Multiple different inhalers
B) Unintentional poor adherence
- Misunderstanding about instructions
- Forgetfulness
- Absence of a daily routine
- Cost
C) Intentional poor adherence
- Perception that treatment is not necessary
- Denial or anger about asthma or its treatment
- Inappropriate expectations
- Concerns about side-effect (real or perceived)
- Dissatisfaction with healthcare providers
- Stigmatization
- Cultural or religious issue
- Cost
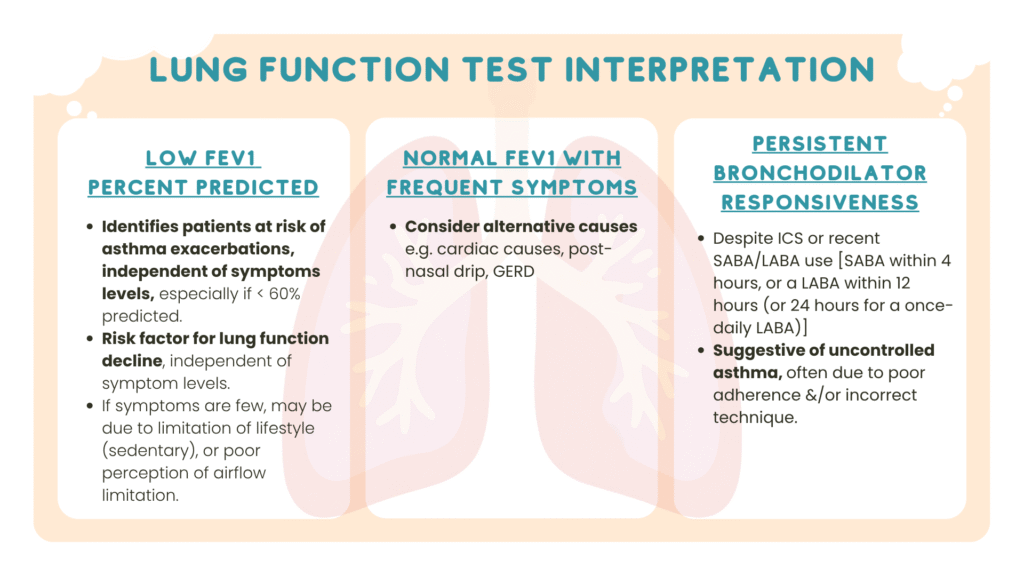
Interpreting lung function test in assessing control
Asthma remission
Can be either on or off treatment.
2 types: Clinical remission & Complete (or Pathophysiological) remission
|
Clinical remission |
Complete (Pathophysiological) Remission |
|---|---|
|
No asthma Sx or attacks for a specific period |
No Sx + Normal lung function, airway responsiveness & inflammation markers |
|
More common at all ages |
Less common |
|
May still have airway hyperresponsiveness/inflammation |
True “disease quiet” |
Clinical remission of asthma in adult life is more common with childhood-onset asthma than adult-onset asthma. However, persistence of airway hyperresponsiveness &/or airway inflammation is found in most adults with clinical remission of asthma.
Severe asthma
It is first important to understand the definition of different terminologies: Uncontrolled asthma, Difficult-to-treat asthma, Severe asthma
Uncontrolled asthma
Defined as poor symptoms control as per GINA questionnaire.
+ Frequent exacerbations:
- ≥ 2 per year requiring OCS &/or
- Serious exacerbation (≥ 1 per year) requiring hospitalization
- Consider also frequent nebulizer use in the local settings.
Difficult-to-treat asthma
Defined as:
- Uncontrolled asthma despite medium- or high-dose ICS with a 2nd maintenance (usually LABA) or maintenance OCS.
- Requires high-dose treatment to maintain good symptoms control & reduce exacerbation risk.
May be due to modifiable factors like:
- Incorrect inhaler technique
- Poor adherence
- Smoking
- Co-morbidities – rhinitis, obesity, GERD, OSA, depression/anxiety
May also be due to incorrect diagnosis/asthma mimickers e.g. vocal cord dysfunction or COPD.
Treatment:
- Optimize treatment – inhaler technique, adherence, change to ICS-formoterol (MART) if available.
- Consider non-pharmacological interventions – e.g. smoking cessation, exercise, weight loss, vaccination
- Treat co-morbidities (more detail below)
- Consider non-biological add-on – LABA, LAMA, LTRA, if not used before
- Consider trial of high dose ICS-LABA if not used
Review response after 3 – 6 months, if still uncontrolled or symptoms become uncontrolled when treatment is stepped down, treat as severe asthma
Managing co-morbidities
Severe asthma
Subset of difficult-to-treat asthma.
Should be referred to specialist for further assessment & management.
Characterized either by:
- Uncontrolled asthma despite adherence to max optimized high-dose ICS-LABA & management of contributory factors OR
- Worsening asthma control when high dose treatment (medium- or high-dose ICS with 2nd controller or maintenance OCS) is reduced.
Inhaler technique & other modifiable factors should be addressed before considering the diagnosis of severe asthma.
Should be evaluated by respiratory physicians for further investigation for alternative diagnosis, phenotypes & be considered for biologic therapy.
Possible DDx:
- Dyspnea: COPD, obesity, cardiac disease
- Cough: inducible laryngeal obstruction (also called vocal cord dysfunction [VCD]), upper airway cough syndrome (i.e. post-nasal drip), GERD, bronchiectasis, ACEi
- Wheeze: obesity, COPD, tracheobronchomalacia, VCD
Treatment options:
A. Biologics – should be considered as add-on treatment
- Phenotype assessment should be done first.
- Examples of biologics: anti-IgE (omalizumab), anti-IL5/5R (mepolizumab, reslizumab, benralizumab), anti-ILF4Ra (dupilumab) and anti-Thymic Stromal Lymphopoietin (tezepelumab)
B. Systemic corticosteroids
- Long-term OCS should be reserved for severe asthma when no alternative treatments are available.
- Should be tapered off or to the lowest effective dose with side effects closely monitored.
C. Macrolide – Azithromycin
- May be considered as an add-on treatment in those who have uncontrolled symptoms despite on high-dose ICS.
- No additional benefit if the patient is already on OCS.
- Recommended dosing:
– 500 mg per dose 3 times per week or 250 mg daily.
– Up to 1 year duration. - Prior to initiating therapy, it is essential to investigate for potential non-tuberculous mycobacterial infection.
- In cases with long QTc medications or risk factors for hearing loss, an ECG &/or audiogram should be considered.
