Asthma Exacerbation

Asthma Exacerbation
Definition
Asthma exacerbation is defined as:
- Progressive or sudden deterioration in baseline clinical status of a patient.
- Characterized by worsening respiratory symptoms e.g. increased SOB, wheezing, coughing & chest tightness.
Common exacerbation triggers
- Viral respiratory infections
- Allergen exposure e.g. grass pollen & other pollens, soybean dust, fungal spores
- Food allergy
- Outdoor air pollution
- Poor adherence with inhaled corticosteroids (ICS)
Assessment
Involves focused history + relevant physical examination + prompt initiation of treatment.
Focused history should include:
- Time of onset
- Triggering factors e.g. respiratory infection, environmental pollutants, stress, etc.
- Symptoms severity
- Risk factors for asthma-related death (as below)
- Allergies
- Current asthma medications, including doses, adherence & response to treatment
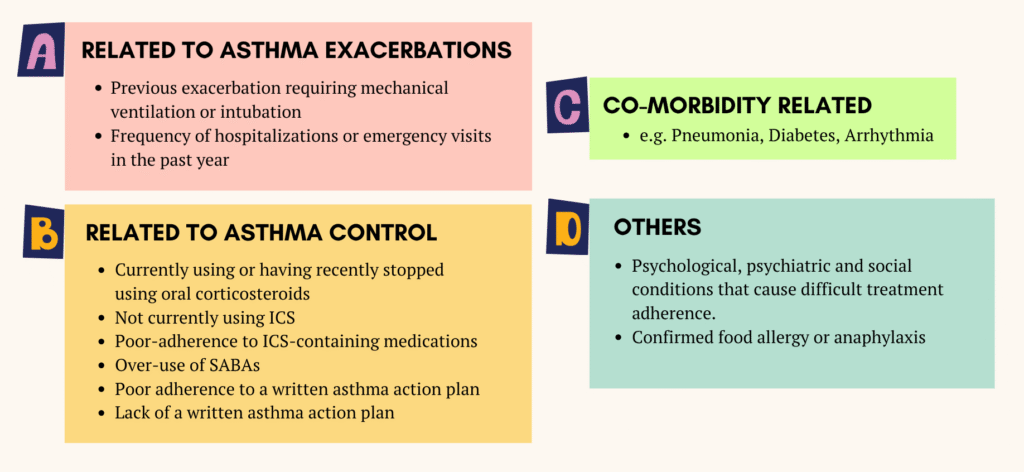
Risk factors for asthma-related death
Physical examination
- Signs of exacerbation severity (as below)
- Vital signs
- Complicating factors e.g. anaphylaxis, pneumonia, pneumothorax
- Signs of differential diagnosis e.g. cardiac failure, inducible laryngeal obstruction, inhaled foreign body or pulmonary embolism.
CXR is not routinely indicated unless there are atypical symptoms, suspected complications or diagnostic uncertainty (e.g. pneumothorax, pneumomediastinum or pneumonia)
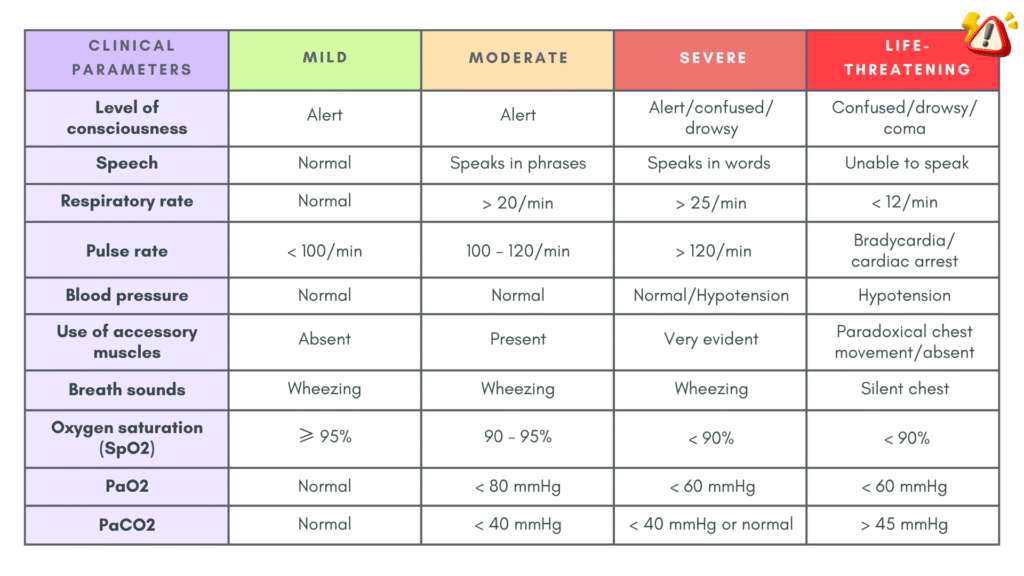
Exacerbation severity
Management of exacerbation at primary care
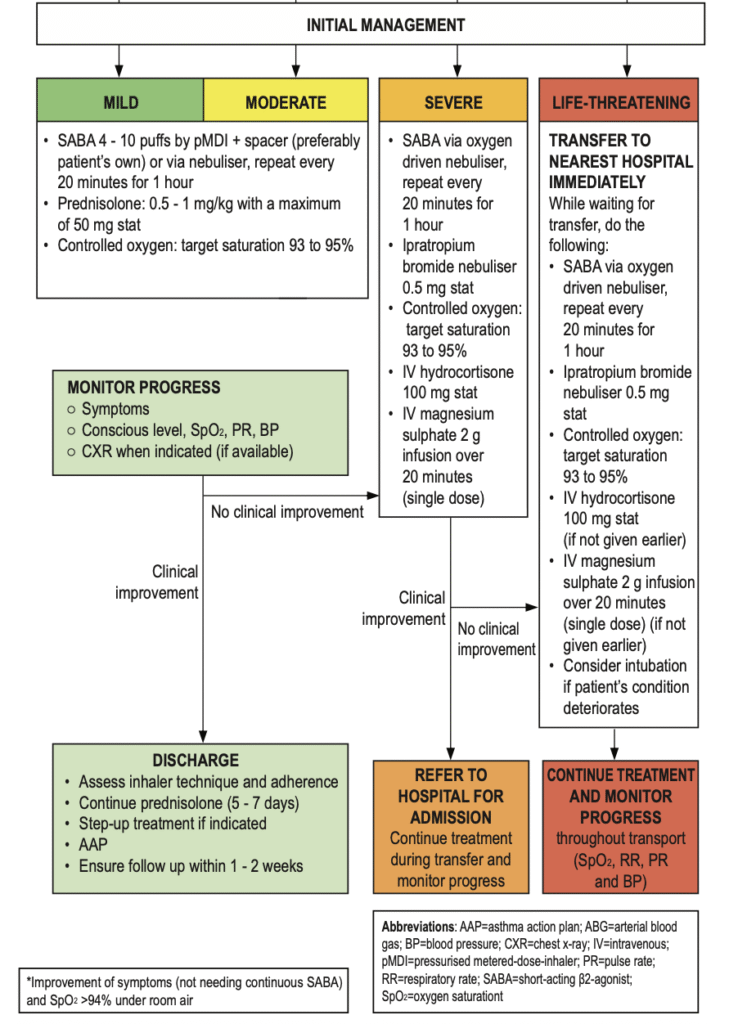
1. Oxygen therapy
- Maintain SpO2 ≥ 94%
2. Inhaled β2-Agonists (First-Line)
- Mild-moderate: pMDI + spacer, 4 – 10 puffs every 20 mins in the 1st hour, then titrate (4 – 10 puffs every 3 – 4 h or 6 – 10 puffs every 1 – 2h)
- Severe/life-threatening: Nebulized β2-agonists, oxygen-driven
- ❌ Avoid oral SABA (systemic side effects)
- Combination with ipratropium bromide is more effective than SABA alone.
2. Systemic corticosteroids
- Start ASAP to reduce inflammation, hasten resolution of exacerbation and prevent relapse.
- Dosage:
– Adults: Prednisolone 0.5–1 mg/kg (max 50 mg) daily for 5–7 days (no taper if <2 weeks).
(Alternatively: IV hydrocortisone 200 mg/day in divided doses – GINA guideline)
– Children 6-11 yrs: Prednisolone 1 – 2 mg/kg/day (max 40 mg) for 3 – 5 days. - Oral, IM or IV route has similar efficacy with the oral route being less invasive & cheaper.
- Continue maintenance inhaled corticosteroids during exacerbation.
3. Magnesium Sulphate
- For severe, refractory asthma: Single IV dose (2g over 20 min)
- No role for repeated dosing (risk of hypermagnesemia) or nebulizer form
4. Aminophylline
- Limited effectiveness –> not recommended routinely
Monitoring
Should include:
- Vital signs – SpO2, respiratory, heart rate & BP
- Mental signs – lethargy, restlessness, etc
- Auscultation – changes in breath sounds, rhonchi or silent chest
- ABG (usually in ED settings) – to monitor hypercapnia or hypoxemia
Criteria for admission
- Progressive deterioration following initial treatment
- Severe or life-threatening asthma
- Other factors to be considered:
– Older age
– Use of > 8 SABA puffs in previous 24 hours
– Past history of severe exacerbations (e.g. intubation, asthma admissions)
– Past history of unscheduled clinic & ED visits requiring use of OCS
– Living alone/socially isolated
– Psychological problems
– Physical disability
Upon discharge
Medications
- Reliever: Use as needed, not regularly
- Controller: Start ICS therapy (Track 1 preferred – if no on MART, start at Step 4) or step up ICS therapy
- Prednisolone: Continue for 5 – 7 days (3 – 5 days for children)
Follow-up
- Review within 2 – 7 days (1 – 2 days for children)
- Assess recovery:
– Is the exacerbation resolving?
– Should prednisolone be continued? - ICS controller:
– Continue higher doses for 2 – 4 weeks.
– Step back to pre-exacerbation dose if well-controlled, unless current exacerbation is due to poor baseline control, in which current higher dose is maintained. - Address modifiable risk factors (inhaler technique, adherence, triggers)
- Provide or update a personalized asthma action plan.
References
- Ministry of Health Malaysia. (2024). Clinical practice guidelines: Management of asthma in adults (2nd ed.). Malaysian Health Technology Assessment Section (MaHTAS).
- Global Initiative for Asthma. (2024). Global strategy for asthma management and prevention.
