Anaphylaxis
Anaphylaxis
In general, anaphylaxis is the most severe end of the spectrum of allergic reactions where there is a severe life-threatening generalized/systemic hypersensitivity reaction.
Pathogenesis
1. IgE-mediated (the classic & most frequent mechanism)
- An allergen (often a protein) interacts with the allergen-specific IgE/high-affinity receptor on mast cells & basophils –> release of preformed mediators
2. Non-IgE-mediated (May be immunologic or non-immunologic)
- Immunologic: Via activation of complement system (anaphylatoxins, C3a, & C5a), activation of contact & coagulation system, or IgG mediated
- Non-immunologic: have been described for some drugs e.g. opioids.
- Activation of mast cells via receptors like Mas-related G-protein coupled receptor member X2 (MRGPRX2) by certain drugs e.g. neuromuscular blocking agents & fluoroquinolones.
Pathophysiology of anaphylactic shock
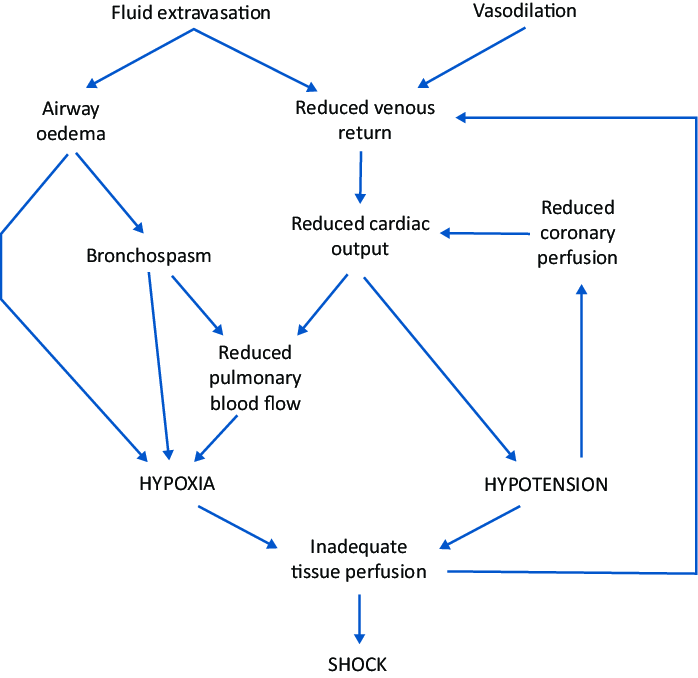
Whyte, Andrew & Soar, Jasmeet & Dodd, Amy & Hughes, Anna & Sargant, Nicholas & Turner, Paul. (2022). Emergency treatment of anaphylaxis: concise clinical guidance. Clinical Medicine. 22. 332-339. 10.7861/clinmed.2022-0073.
Common anaphylaxis elicitors
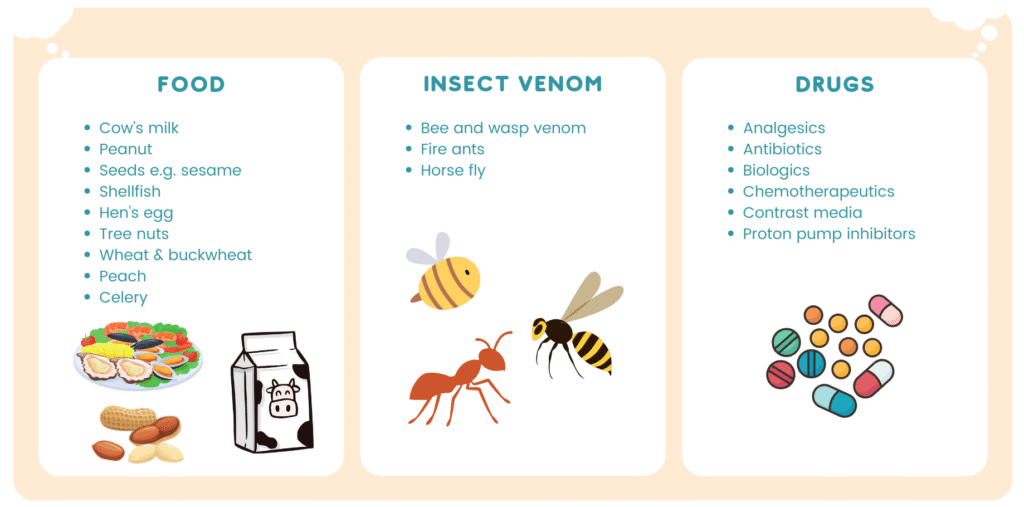
Note: The elicitors may vary in frequency depending on age, geographical region & lifestyle
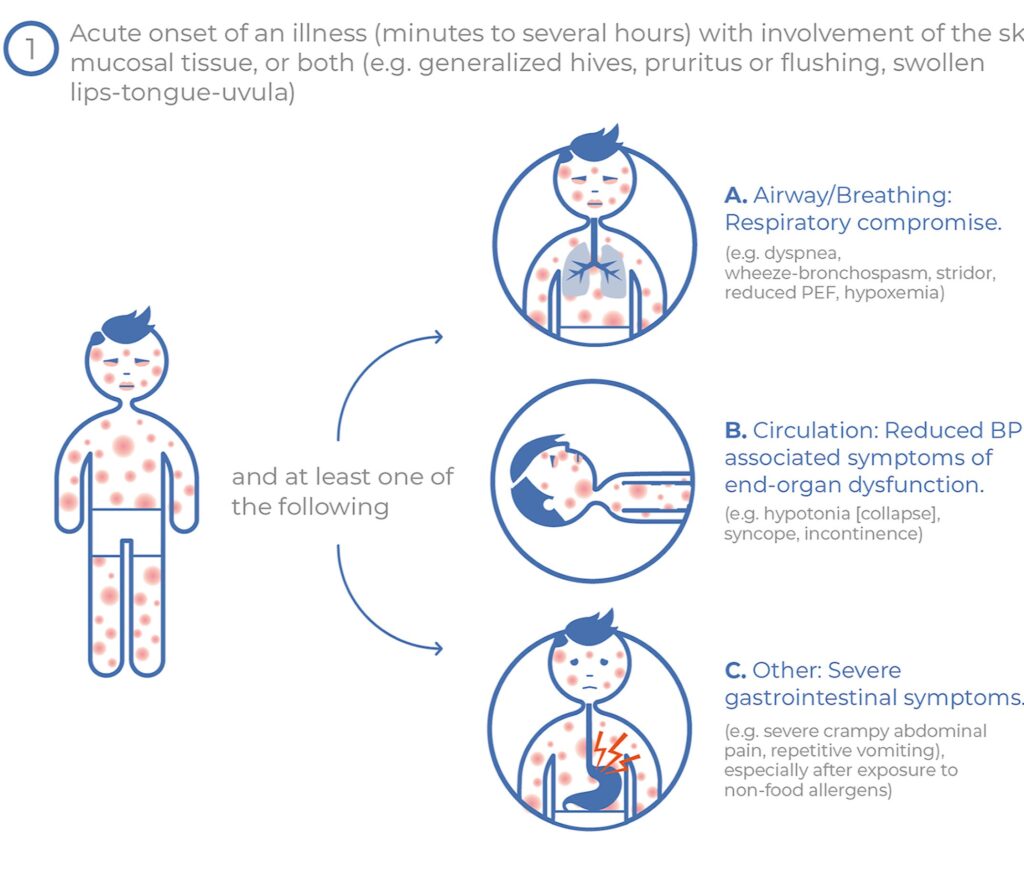
Criteria to help identify anaphylaxis
There are different definitions of anaphylaxis that may vary according to literatures. We are familiar that anaphylaxis is likely when it involves more than one organ system.
However, anaphylaxis can present initially with isolated respiratory or cardiovascular symptoms (though not constituting as anaphylaxis under the NIDAID criteria) and should be managed accordingly.
In view of this, the World Allergy Organization has proposed the following criteria to aid in diagnosis of anaphylaxis.
Anaphylaxis is highly likely when any one of the following 2 criteria are fulfilled
Criteria 1
Acute onset of an illness (minutes to hours) with simultaneous involvement of the skin, mucosal tissues, or both (e.g. generalized hives, pruritus or flushing, swollen lips-tongue-uvula)
AND AT LEAST ONE OF THE FOLLOWING
a. Respiratory symptoms e.g. dyspnea, wheeze-bronchospasm, stridor, reduced PEF, hypoxemia)
b. Reduced BP or associated symptoms of end-organ dysfunction e.g. hypotonia/collapse, syncope, incontinence
c. Severe GI symptoms (e.g. severe abdominal cramp, persistent vomiting), especially after exposure to non-food allergen
Criteria 2
Acute onset of hypotension, or bronchospasm or laryngeal involvement after exposure to a known or highly probable allergen for that patient (minutes to several hours), even in the absence of typical skin involvement.
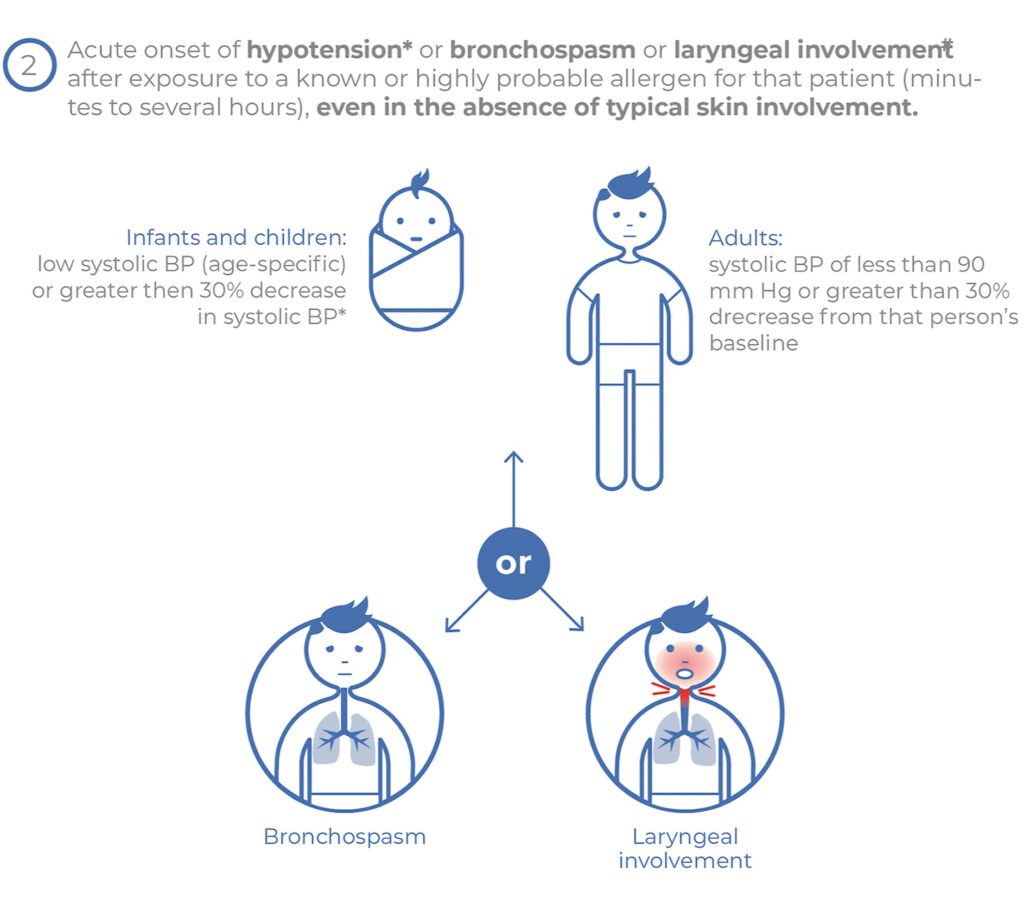
Further elaboration on criteria 2 regarding hypotension, bronchospasm & laryngeal involvement
Definition of hypotension
- Decrease in SBP > 30% from the patient’s baseline OR
- In infants & children < 10 years: SBP less than (70 mmHg + [2 x age in years])
- In adults & children > 10 years: SBP less than 90 mmHg
Bronchospasm
- In this setting, should first exclude lower respiratory symptoms triggered by common inhalant allergens or food allergens perceived to cause “inhalational” reactions in the absence of ingestion.
Laryngeal involvement
- Symptoms: stridor, vocal changes, odynophagia
It is important to keep in mind that these criteria serves to aid in diagnosis and are not a definition per se.
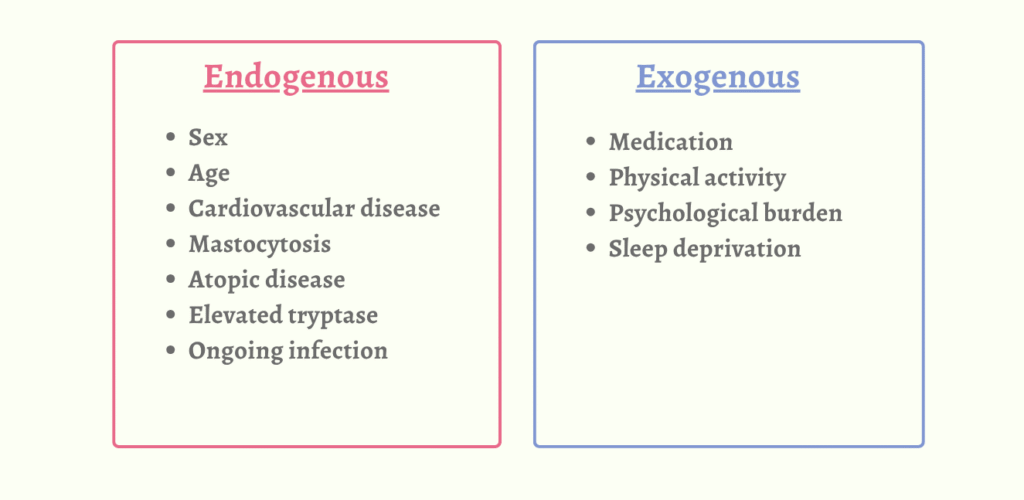
Cofactors
These are endogenous &/or exogenous factors that may aggravate the severity of anaphylaxis.
Common differential diagnosis
- Acute asthma
- Syncope
- Anxiety/panic attack
- Acute generalized urticaria
- Foreign body aspiration
- Cardiovascular e.g. MI, pulmonary embolus
- Neurological e.g. seizure, CVA
Note that these are some of the common diagnostic dilemmas and does not represent the full list of differential diagnosis.
Acute management of anaphylaxis🚨
1. Remove exposure to trigger.
2. Assessment of ABC – Airway, Breathing, Circulation
3. Call for help (ambulance) if not already in hospital setting
4. IM Adrenaline 0.01 mg/kg of a 1:1,000 (1 mg/ml) solution over the mid-anterolateral aspect of the thigh. [MAINSTAY]
- Max 0.5 mg (adult) or 0.3 mg (child) – Dosage will again be discussed below
- Can repeat every 5 – 15 minutes, if needed
5. Place patient in supine position as fatality can occur rapidly if patient stands, walks or sits suddenly.
- Rationale of supine position – To improve venous return to the heart.
- Consider sitting with legs outstretched if there is respiratory distress (to optimize respiratory effort) or vomiting episodes. Lay the patient flat if there is reduced consciousness or hypotensive.
- If unconscious or pregnant, place in recovery position (on left side if pregnant, to reduce risk of IVC compression)
- Hold young children flat, not upright
- Do not allow them to stand or walk, even if they appear to have recovered. Only allow them to stand or walk once hemodynamically stable, which is usually a minimum of 1 hour after 1 dose of adrenaline and 4 hours if more than 1 dose of adrenaline.
6. Establish IV access with large-bore cannula and consider starting bolus of NS (20 mL/kg) in patients with cardiovascular instability.
7. Perform CPR if indicated
8. Frequent/continuous vitals monitoring (BP, HR, respiratory status, & oxygenation)
9. Others
- High flow oxygen (preferably 100% using non-rebreather facemask) in patients with respiratory distress/reduced conscious level/those requiring repeated dose of adrenaline.
- Neb SABA (e.g. salbutamol/albuterol) if there are symptoms of bronchoconstriction.
– Salbutamol 8 – 12 puffs of 100 ug (spacer) or 5 mg (nebuliser) - Consider neb adrenaline (5 mL e.g. 5 ampoules of 1:1000) if there is upper airway obstruction.
- Corticosteroids (benefit unproven)
– Oral prednisolone 1 mg/kg (max 50 mg) or
– IV hydrocortisone 5 mg/kg (max of 200 mg)
Pharmacological agents for anaphylaxis management
Adrenaline (Epinephrine) – Mainstay
|
Age group |
Dose |
Equivalent (in mL) |
|---|---|---|
|
Infants < 10 kg |
0.01 mg/kg |
0.01 mL/kg of 1 mg/mL (1 : 1000) |
|
Children aged 1 – 5 years |
0.15 mg |
0.15 mL of 1 mg/mL (1 : 1000) |
|
Children aged 6 – 12 years |
0.3 mg |
0.3 mL of 1 mg/mL (1 : 1000) |
|
Teenagers and adults |
0.5 mg |
0.5 mL of 1 mg/mL (1 : 1000) |
Adrenaline 1 : 1,000 ampoules contain 1 mg adrenaline per 1 mL
Quick dosing guide:
- Recommended dose per administration is 0.01 mg/kg of body weight to a max of 0.5 mg in adults & child > 30 kg and 0.3 mg in child ≤ 30 kg.
- Dosing can be repeated every 5 – 15 mins if needed.
Route:
IM route is preferred & is generally well tolerated.
IV route (should ideally be administered by trained specialist)
- Has risk of causing fatal arrhythmias especially with bolus administration.
- If IV route is used, it should be diluted and the correct dose should be administered.
- Give as infusion via dedicated line, infusion pump (rather than bolus) and anti-reflux valves wherever possible
- Patient should be monitored closely.
- IV route can be used if patient is in anaphylactic shock, and can be given as 0.1 mg/mL (1:10,000) solution with 0.1 – 0.25 mg (1 – 2.5 mL) given by slow IV injection. Dose may be repeated every 5 – 15 mins if needed or followed by IV infusion at a rate of 0.001 – 0.004 mg/min. However, there may be some variation in dosage & treatment recommendations among countries & individual products [5].
- 1:10,000 dilution can be done by mixing 1 mL of (1:1,000) vial with 9 mL of normal saline.
- Caution: IV boluses are NOT recommended due to risk of cardia ischaemia or arrhythmia UNLESS the patient is in cardiac arrest.
Antihistamines
Considered 2nd line or even 3rd line in some guidelines as they have limited role in treatment of anaphylaxis, but can helped with relieving cutaneous symptoms. They have no role in treating the respiratory or cardiovascular symptoms.
The sedative effect (drowsiness/lethargy) of 1st gen antihistamine may mimic some signs of anaphylaxis, thus are not recommended.
2nd gen antihistamines are preferred (due to less sedation effect) but currently only 1st gen antihistamines are available for parenteral administration (e.g. IM/IV chlorpheniramine)
- Caution: Rapid IV administration of 1st gen antihistamine can cause/worsen hypotension
Glucocorticoids
Commonly used.
Can be given as IV hydrocortisone 200 mg bolus
However, their routine use is becoming controversial as there have been evidence showing no benefit in the acute management of anaphylaxis.
Glucagon
May be used if patient does not response to adrenaline or when adrenaline is relatively contraindicated e.g. in pt with IHD, severe HTN, pregnancy.
May be helpful especially for patients taking beta-blockers.
Dose: 1 – 5 mg IV over 5 mins, followed by 5 – 15 ug/min infusion titrated to clinical response.
Short Acting Beta-2 agonists
E.g. Salbutamol, Albuterol
Given by inhalation or nebulization
Disposition
All patients with anaphylaxis should be referred to hospital for further assessment and monitoring 🚑.
One of the concern after the resolution of the initial reaction, is the occurrence of biphasic reaction, which refers to the recurrence of symptoms meeting the anaphylaxis diagnostic criteria, after the resolution of initial symptoms, & without re-exposure to the trigger.
- This may occur 1 – 72 hours after the initial reaction, with some studies mentioning a mean time of >8 hours [3] whereas it is mentioned in the WAO guidelines as 6 – 12 hours.
- Nevertheless, mortality is rare.
WAO guidelines advised for patient to be observed for at least 4 hours after the last dose of adrenaline.
Relapse, protracted &/or biphasic reactions may occur & overnight observation is strongly recommended if they:
- Had a severe/protracted anaphylaxis, requiring repeated dose of adrenaline or IV fluid resuscitation OR
- Have a h/o severe/protracted anaphylaxis OR
- Have other concomitant illness (e.g. severe asthma, h/o arrhythmia, systemic mastocytosis) OR
- Live alone or have difficulty in accessing medical care OR
- Present for medical care late in the evening.
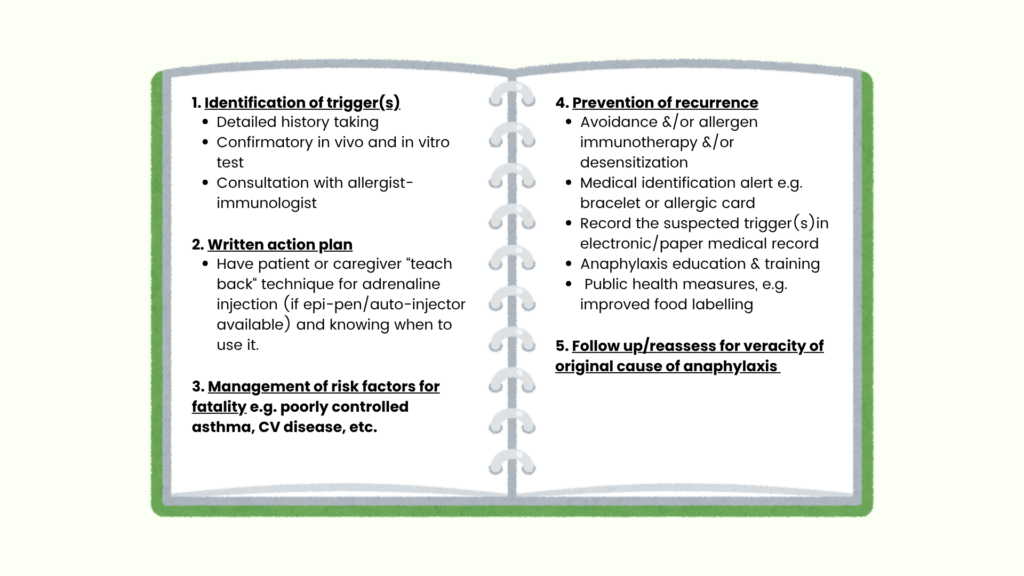
Long-term management/Discharge plan
References
- Cardona V, Ansotegui IJ, Ebisawa M, El-Gamal Y, Fernandez Rivas M, Fineman S, Geller M, Gonzalez-Estrada A, Greenberger PA, Sanchez Borges M, Senna G, Sheikh A, Tanno LK, Thong BY, Turner PJ, Worm M. World allergy organization anaphylaxis guidance 2020. World Allergy Organ J. 2020 Oct 30;13(10):100472. doi: 10.1016/j.waojou.2020.100472. PMID: 33204386; PMCID: PMC7607509.
- Australasian Society of Clinical Immunology and Allergy . ASCIA Guidelines: Acute management of anaphylaxis. ASCIA, 2024. https://www.allergy.org.au/hp/papers/acute-management-of-anaphylaxis-guidelines
- Pourmand A, Robinson C, Syed W, Mazer-Amirshahi M. Biphasic anaphylaxis: A review of the literature and implications for emergency management. Am J Emerg Med. 2018 Aug;36(8):1480-1485. doi: 10.1016/j.ajem.2018.05.009. Epub 2018 May 9. PMID: 29759531.
- Whyte, Andrew & Soar, Jasmeet & Dodd, Amy & Hughes, Anna & Sargant, Nicholas & Turner, Paul. (2022). Emergency treatment of anaphylaxis: concise clinical guidance. Clinical Medicine. 22. 332-339. 10.7861/clinmed.2022-0073.
- Epinephrine. In MIMS online. Retrieved 27 June 2025, from https://www.mims.com/malaysia/drug/info/epinephrine?mtype=generic
