Preeclampsia

Preeclampsia
Definition
Preeclampsia refers to new-onset hypertension after 20 weeks of gestation that is associated with:
- Proteinuria OR
- Significant end-organ dysfunction in the absence of proteinuria
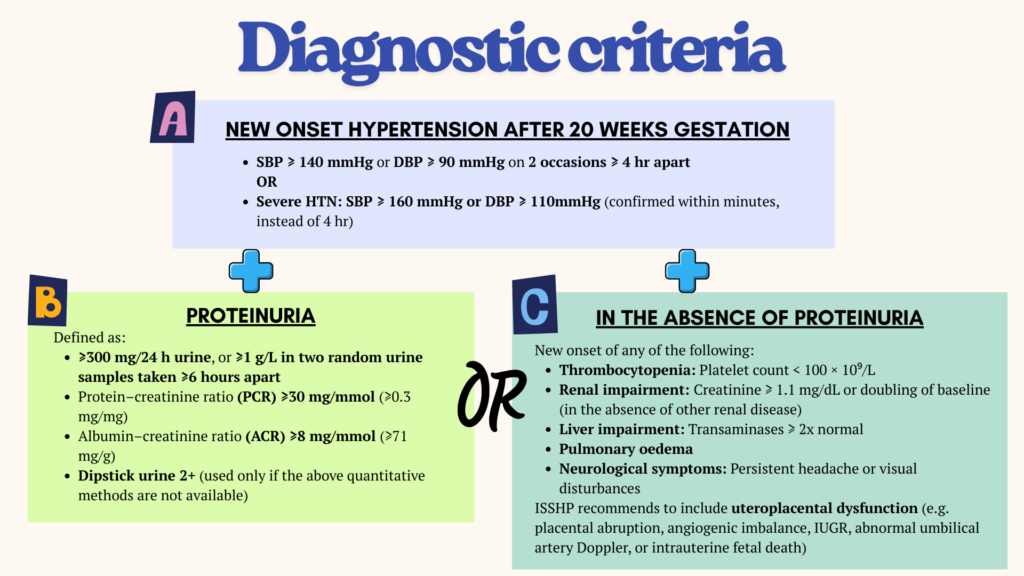
Regarding urine dipstick
Has low diagnostic accuracy – neither sensitive nor specific at the 1+ level.
Confirmatory quantitative proteinuria testing (urinary PrCr, ACR or 24 hr urine collection) should be done when pre-eclampsia is suspected, e.g.
- ≥ 1+ dipstick proteinuria in women with HTN & rising BP
- In women with normal BP, but SSx suggestive of preeclampsia.
In the event that confirmatory test is not available, then dipstick proteinuria of ≥ 2+ provides a reasonable assessment of true proteinuria.
In a patient with diagnosed preeclampsia, a heavy proteinuria of 4+ on dipstick may predict adverse perinatal outcome. However this predictive value is only limited to settings without advanced fetal surveillance capacity.
Pathophysiology
Preeclampsia is a complex disorder driven primarily by placental and maternal endothelial dysfunction, which is represented in a two-stage model.
Stage 1: Abnormal placentation
- Inadequate trophoblast invasion of spiral arteries, influenced by maternal susceptibility & risk factors
- Failure to remodel vessels into low-resistance, high-flow channels
- Results in placental hypo perfusion, hypoxia & ischemia.
Stage 2: Maternal systemic response
- Ischemic placenta releases anti-angiogenic factors (e.g. ↑ sFlt-1, ↓ VEGF/PlGF) and ↑ reactive oxygen species.
- Causes widespread endothelial dysfunction
- Leads to hypertension, proteinuria & multi-organ involvement.
Nevertheless, there may be multiple subtypes with different pathophysiological pathways, rather than a single one size fits all mechanism.
Risk factors
Risk factors for preeclampsia should be promptly assessed during antenatal follow up, so that appropriate prophylaxis can be started.
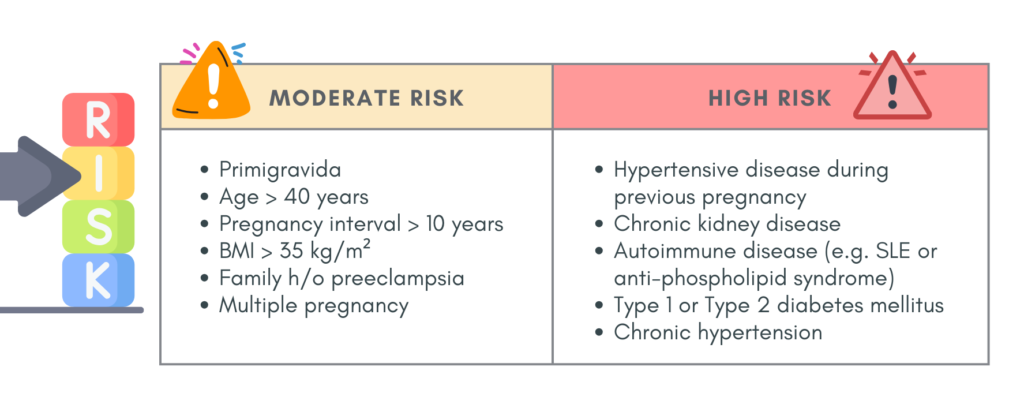
Prophylaxis for preeclampsia
1. Aspirin
- Start low-dose aspirin in women with ≥ 1 high risk or ≥ 2 moderate risk factors.
- Initiate at 12 – 16 weeks gestation & continue until delivery.
- Dose: 100 – 150 mg OD at bedtime. (75 – 150 mg RCOG; 75 mg Malaysia Training Manual)
– The ISSHP guideline do not recommend dose of < 100 mg, due to platelet insensitivity (seen in ~40% of women), especially as pregnancy advances & with higher BMI.
2. Calcium
- 500 – 1000 mg daily, started before 20 weeks of gestation.
- Reduces preeclampsia risk, particularly in women with low dietary calcium intake (< 900 mg/day)
- Should be given in addition to aspirin, when indicated.
Clinical assessment – History & Physical Examination
Aim is to identify high risk pregnant women and any SSx preeclampsia/impending eclampsia.
History
Risk factors assessment:
- Family history of HTN
- h/o pregnancy induced HTN
- Primigravida
- Associated conditions:
– Multiple pregnancy
– Diabetes mellitus
– Renal disease
– SLE/anti-phospholipid syndrome
– Obesity (> 80 kg; BMI > 27)
– Maternal age
– Pre-existing chronic hypertension
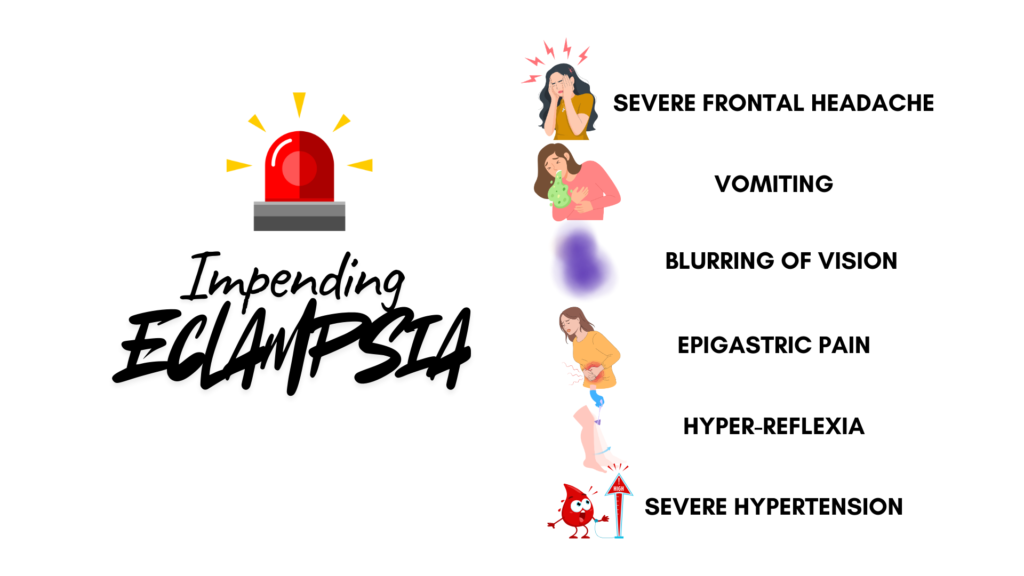
Watch out for any indications for hospital referral (NICE):
- Sustained SBP ≥ 160 mmHg
- Maternal biochemical or hematological investigations (rise in creatinine/risk in ALT/fall in platelet count)
- Signs of impending eclampsia
- Signs of impending pulmonary edema
- Other signs of severe pre-eclampsia
- Suspected fetal compromise
- Any other concerning clinical signs.
Physical examination
- BP measurement
- Excessive weight gain (> 1 kg per week)
- Edema in the face & abdomen &/or non-dependent oedema
- Obesity (BMI > 27 or Wt 80 kg)
- Abdominal examination – polyhydramnios, multiple pregnancy
- Proteinuria
Prediction of preeclampsia
This can be done by measuring the angiogenic markers – sFlt-1/PlGF (soluble fms-like tyrosine kinase-1/platelet growth factor) from ≥ 20 weeks gestation.
- Angiogenic imbalance is defined by:
– Low PlGF (< 5th centile for gestational age), or
– High sFlt-1/PlFG ratio (e.g. > 38, Roche assay) - The sFLt/PlGF ratio has a high negative predictive value for preeclampsia within 1 week & is useful in:
– Identifying patients needing admission & close monitoring.
– Guiding decisions on antenatal corticosteroids when preterm delivery is anticipated.
An alternative approach is using the “Triple test” approach (The Fetal Medicine Foundation model – recommended in the ISSHP guidelines), which consists of:
- Identifying clinical risk factors & blood pressure
- Serum PlGF
- Uterine artery doppler ultrasound
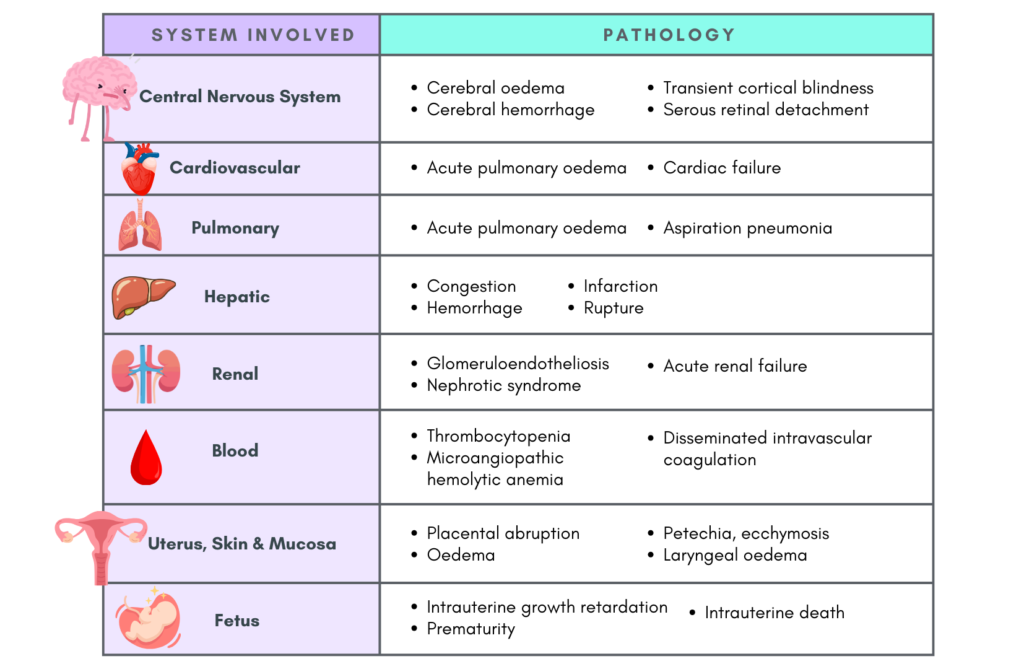
Complications of preeclampsia
Maternal & Fetal monitoring in Preeclampsia
This section may not be that applicable in the primary care settings, however there is no harm with gaining extra knowledge. Nevertheless these are based on guidelines, and local practices may differ.
Maternal monitoring
Risk prediction can be done using fullPIERS (usable at any gestation) or PREP-S (up to 34 weeks) to guide level of care, need for transfer, & intervention thresholds (NICE guideline). However, neither model predicts neonatal outcomes.
fullPiers components include:
- Gestational age
- Chest pain or dyspnea
- Oxygen saturation
- Platelet count
- Serum creatinine
- AST or ALT
Proteinuria is not included as repeat testing is usually unnecessary once proteinuria is confirmed.
When lab results are unavailable, miniPIERS may be used, which consist of:
- Systolic blood pressure
- Dipstick proteinuria
- Parity
- Gestational age
- Symptoms (headache/visual changes, chest pain/dyspnea, abdominal pain ± vaginal bleeding)
Uric acid (gestation-adjusted) may be an additional marker for monitoring as it is associated with increased risk of adverse maternal & fetal outcomes.
Fetal monitoring
a) Structural screening – especially in chronic hypertension
- NT scan: 12 – 14 weeks
- Detailed anomaly scan (by MFM): 22 – 24 weeks (Increased risk of congenital cardiac anomalies)
- Cardiology referral if cardiac anomaly detected.
b) Growth & doppler surveillance
- Ultrasound every 2 weeks for – fetal growth, amniotic fluid volume & umbilical artery doppler.
- At ≤ 33 + 6 weeks with fetal growth restriction, consider ductus venosus doppler. If absent/reversed a-wave –> high stillbirth risk
Biophysical profile is not recommended as it can be falsely reassuring, & an abnormal profile is usually a late finding.
Management at primary care
Women with pre-eclampsia/severe hypertension should be assessed & managed in hospital.
Pre-eclampsia can progress quickly, without warning. The level of BP itself is not reliable to stratify immediate risk in pre-eclampsia.
When BP is ≥ 160/110 mmHg, urgent treatment in a monitored setting is required.
Common anti-hypertensive drugs used are: Labetalol, Nifedipine and Hydralazine.
- Among these, only nifedipine can be given orally, whereas both labetalol & hydralazine are administered parenterally in cases of acute hypertensive crisis.
- Dose of nifedipine:
– Oral 5 – 10 mg stat (repeat in 30 mins if needed)
– After the initial emergency dose, 10 – 20 mg can be given every 3 – 6 hours until BP stabilizes.
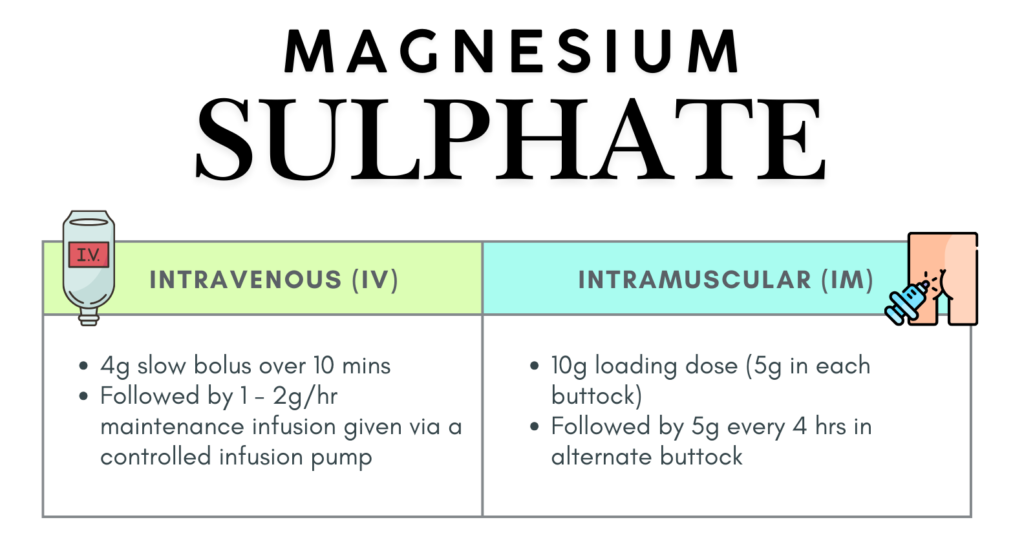
Another critical medication is Magnesium Sulphate, which is used for the treatment of eclampsia and prevention of eclampsia in patient with severe pre-eclampsia
Preeclampsia/Severe hypertension management at primary care
- Refer to hospital and arrange transport immediately.
- Inform the receiving hospital (labour room) prior to referral.
- Set up an IV drip with normal saline for emergency drug administration if the need arises.
- Give IM MgSO4 10g bolus (5g each buttock) to prevent eclampsia.
- Give oral nifedipine (10 mg stat) or IM hydralazine 6.25 mg (Prepared by mixing 1 ampule [20 mg] hydralazine + 9 ml distilled water = 2 mg/ml, then give 3.1 mL [6.2 mg])
- Monitor & record the maternal BP, pulse rate & fetal heart rate every 15 mins.
- Patient should be accompanied during transfer.
Eclampsia management at primary care
- Call for help.
- Put patient in lateral position, maintain airway and given oxygen through nasal prong/ventimask.
- Give IM MgSO4
- Start parenteral antihypertensive therapy (e.g. hydralazine or labetalol) if available or nifedipine.
- Set up an IV drip with normal saline for emergency drug administration for further resuscitation.
- Suck out secretions
- Insert Foley’s catheter to record & monitor urine output.
- Monitor & recored maternal BP, PR, RR & fetal heart rate every 15 minutes using Labour Progress Chart.
- Arrange for transport, inform the labour room personnel of the hospital and accompany the patient to the hospital.
- Prepare IV MgSO4 2g (or 5g for IM) in a drying in case patient have a recurrent seizure during transfer.
References
- Magee, L. A., Brown, M. A., Hall, D. R., Gupte, S., Hennessy, A., Karumanchi, S. A., Kenny, L. C., McCarthy, F., Myers, J., Poon, L. C., Rana, S., Saito, S., Staff, A. C., Tsigas, E., & von Dadelszen, P. (2022). The 2021 International Society for the Study of Hypertension in Pregnancy classification, diagnosis & management recommendations for international practice. Pregnancy hypertension, 27, 148–169. https://doi.org/10.1016/j.preghy.2021.09.008
- Hypertension in pregnancy: diagnosis and management. London: National Institute for Health and Care Excellence (NICE); 2019 Jun 25. (NICE Guideline, No. 133.)
- Ministry of Health Malaysia. (2018). Training manual hypertensive disorder in pregnancy (3rd ed.). Family Health Development Division, Ministry of Health Malaysia. Retrieved January 20, 2026
