Onychomycosis
Onychomycosis
Nail anatomy
Having a basic knowledge of the nail anatomy can help in understanding the various subtypes of fungal nail infections. Thus, a general overview of basic nail anatomy will be discussed first.
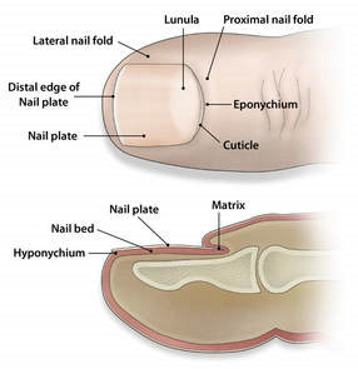
Nail plate: the hard, visible part of the nail, composed of keratinized cells
Nail matrix: located beneath the proximal nail fold, it’s the area where new nail cells are generated.
Nail folds (proximal and lateral): soft tissue structures that surround the nail plate, providing protection & support.
Eponychium: Layer of live cells under the surface of the proximal nail fold that produces the cuticle
Cuticle: A thin layer of dead skin cells that grows from the eponychium and adheres to the nail plate, sealing the nail unit.
Both the Eponychium and Cuticle act as a protective seal that protect the nail bed and matrix from infection.
Hyponychium: The area of skin beneath the free edge of the nail plate, extending from the nail bed, acting as a barrier against germs & debris.
Lunula: The whitish, half-moon shape at the base of the nail plate, representing the visible part of the matrix.
Common organisms involved
1. Dermatophytes (most common) – Tricophyton, Microsporum, Epidermophyton
- When the infection is caused by dermatophytes, then it is also called as Tinea Unguium
2. Non-dermatophyte molds (NDMs) – e.g. Scopulariopsis brevicaulis, Aspergillus spp., Fusarium spp., etc.
3. Yeasts – e.g. Candida spp.
These fungi can produce enzymes with proteolytic, keratinolytic, & lipolytic activities that degrade the keratin in the nails, facilitating fungal invasion of the nail.
Risk factors
- Diabetes
- Immunosuppression
- Advancing age
- Peripheral arterial disease
- Sports activities
- Pre-existing dysmorphic nails due to disease such as psoriasis or trauma
- Tinea pedis
Clinical features
Toenails (big toe commonly affected) are more frequently affected compared to fingernails.
There may also be concurrent cutaneous fungal infection like tinea manuum & tinea pedis.
General nail morphology in onychomychosis
- Thickened nail plate (Onychauxis)
- Discolouration
- Detachment of nail form the nail bed (Onycholysis)
- Subungual hyperkeratosis
- Dermatophytoma – linear, single or multiple white/yellow/orange/brown bands on the nail plate (specific for onychomycosis)

Subtypes
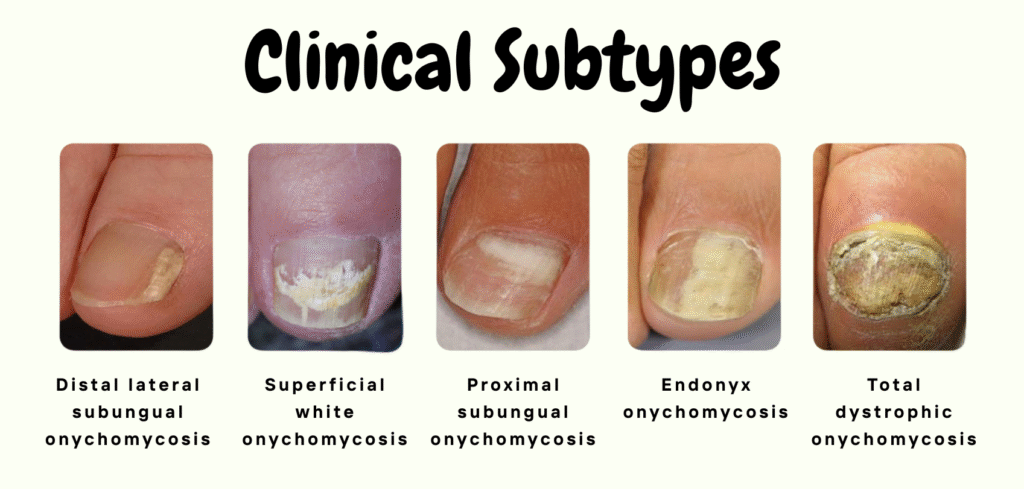
Onychomycosis can be classified based on the pattern and site of infection of the nail complex into :
- Distal lateral subungual onychomycosis (DLSO)
- Superficial white onychomycosis (SWO)
- Proximal subungual onychomycosis (PSO)
- Endonyx onychomycosis
- Total dystophy
|
Subtypes |
Site of Invasion |
Organisms |
Clinical Presentation |
|---|---|---|---|
|
Distal Lateral Subungual Onychomycosis |
Hyponychium → Distal nail bed → Nail plate |
T. rubrum T. mentagrophytes |
Yellowish/whitish/brownish discolouration of the distal corner of the nail Distal subungual hyperkeratosis Onycholysis Onychauxis of the lateral & distal aspect of the nail |
|
Superficial White Onychomycosis |
Upper surface of nail plate |
T. mentagrophytes |
White dots or patches on the surface of the nail plate which can be easily scraped off |
|
Proximal Subungual Onychomycosis |
Undersurface of the proximal nail fold near the cuticle, then extends distally |
T. rubrum Fusarium spp. |
Area of leukonychia in the proximal nail plate & moves distally with nail growth |
|
Endonyx Onychomycosis |
Infection of the nail plate without infection of the nail bed |
T. soudanense T. violaceum |
Milky patches of the nail plate Indentation, lamellar splitting Nail plate firmly attached to the nail bed Subungual hyperkeratosis is ABSENT |
|
Total Dystrophic Onychomycosis |
End stage of all the other subtypes |
– |
Severely dystrophic & crumbled nail plate which is yellowish, diffusely thickened & friable |
Photos from https://bespokehealthandperformance.com.au/types-of-toenail-fungus/
Diagnosis
Onychomycosis can be suspected based on clinical features with suggestive nail morphology as above.
Dermoscopy can help to differentiate onychomycosis from other nail disorders.
Dermoscopy findings may include:
- Jagged proximal edge with spikes in the onycholytic area (most common)
- “Ruined” appearance of the subungual hyperkeratosis
- White to yellow longitudinal streaks/striae
- Leukonychia
- Chromonychia
- Parallel bands of different colors (“aurora borealis”)
- Dermatophytoma
Diagnostic confirmation of onychomycosis prior to initiating treatment is recommended, given the typically prolonged treatment duration and the potential for adverse drug reactions.
Confirmation of onychomycosis can be done via:
- Direct microscopic examination with a Potassium Hydroxide (KOH) wet-mount preparation.
- Histopathologic examination with a Periodic-Acid-Schiff (PAS) stain
- Fungal culture
- Polymerase Chain Reaction (PCR) assays
Depending on the clinical presentations, nail clippings, nail plate/bed scrapings, and subungual scrapings with sterile nail clipper/curetter/blade may be needed for sample collection.
Sample collection based on subtypes:
- For distal & lateral subungual onychomycosis: from the most proximal area of involvement (most active area of infection) after clipping the distal onycholytic nail plate.
- White superficial onychomycosis: superficial aspect of the nail plate is scraped with a no. 15 plate.
- Proximal subungual onychomycosis: upper nail plate of the proximal nail should be debrided or pared & the underlying nail debris collected with a curette.
Prior to sample collection, the nail plate & the surrounding soft tissue should be cleaned with 70% isopropyl or ethyl alcohol to prevent contamination.
Treatment
Aim of treatment: To achieve both clinical (clinically normal nails) & mycological (negative microscopy & culture) cure.
Current treatment options:
- Oral antifungal agents (e.g. terbinafine, itraconazole) – mainstay
- Topical antifungal agents
- Combination (oral + topical antifungals) – improve cure rate
Oral antifungal agents
First line in most cases, especially when > 50% of the nail is affected, multiple nails are affected, the nail matrix is involved, or when dermatophytoma is present.
2 main agents that have shown good results: Terbinafine (most effective), Itraconazole
Terbinafine is generally preferred over itraconazole due to its better cure rates, less potential side effects & drug interactions.
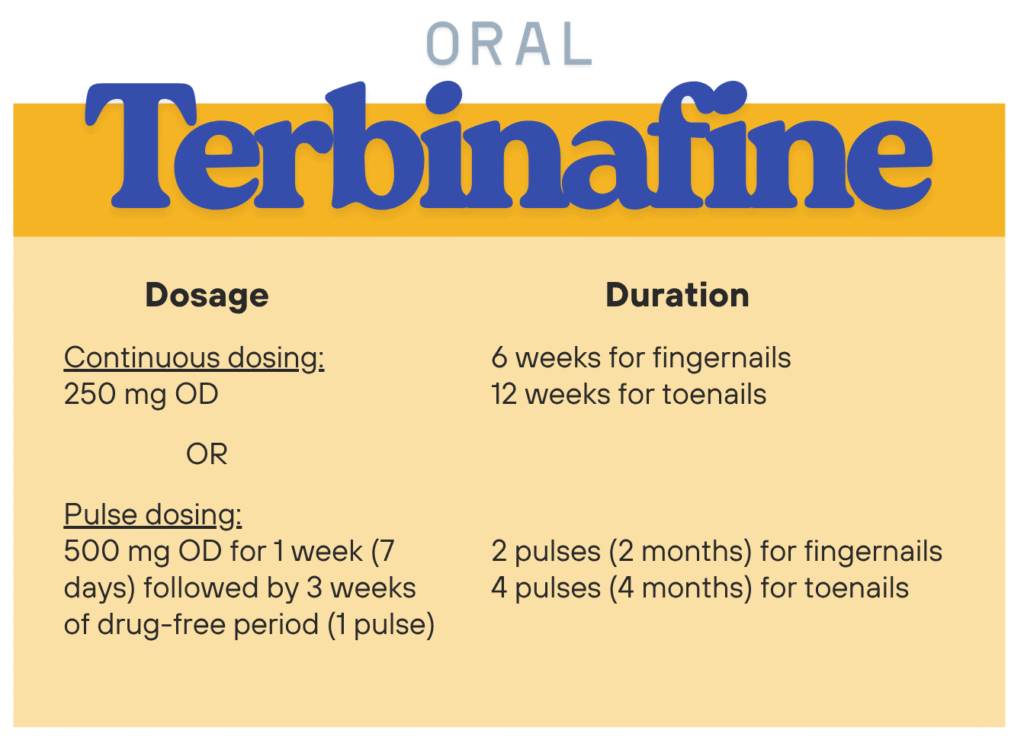
Can be used for dermatophytes, Candida species, and non-dermatophyte molds (less responsive & may required longer treatment duration), especially Aspergillus fumigatus & Scopulariopsis brevicaulise.
Continuous dosing of oral terbinafine has been the usual dosing regimen for onychomycosis.
However, there are some small studies that have shown that when given in pulses, it has similar efficacy as in continuous dosing, and hence may be considered.
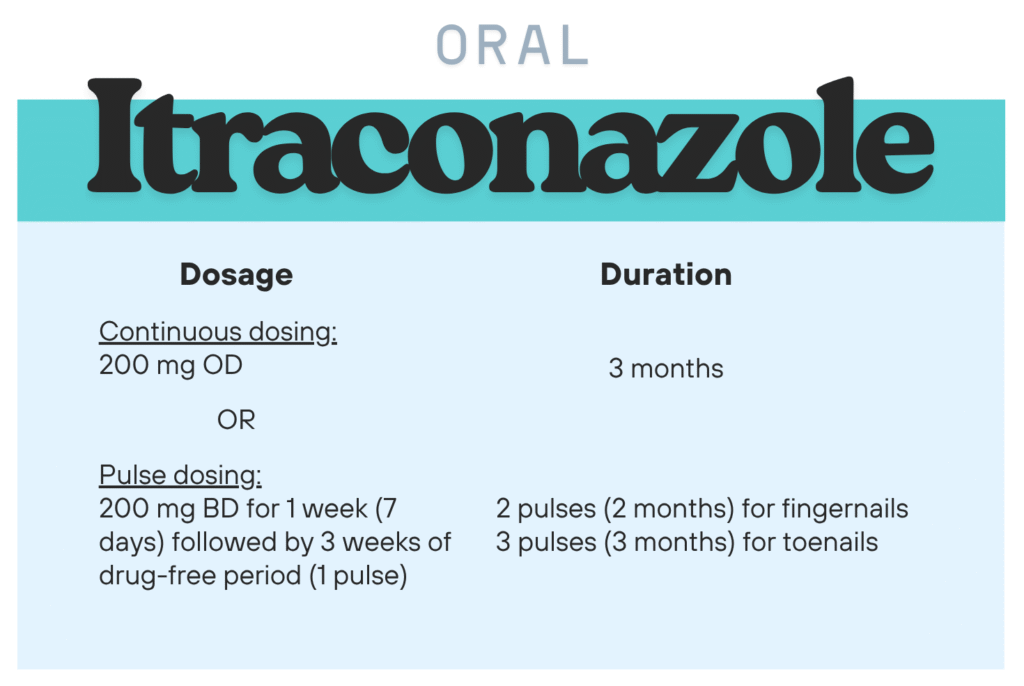
Effective against dermatophytes & yeasts, and may also be used for non-dermatophyte molds.
Has more drug interactions & adverse effects compared to terbinafine.
Itraconazole absorption is dependent on an acidic gastric environment. For optimal absorption, take with food & acidic beverage (e.g. cola or orange juice). Use of proton pump inhibitors (PPIs) and H2-receptor antagonists should be avoided.
Other oral antifungal agents
Fluconazole
- May be used but requires longer treatment duration compared to itraconazole & provides only moderate success.
- Dosage: 150 mg once per week (Fingernails ≥ 3 months; Toenails 6 – 12 months)
Oral Ketoconazole: Not recommended due to risk of severe hepatitis & adverse drug interactions.
Griseofulvin: Should be avoided due to its low cure rate & higher incidence of adverse events.
Topical antifungals
Topical antifungals are often used in combination with nail lacquers to improve nail penetration and enhance fungicidal activity. This approach also prolongs drug contact time on the nail surface and increases local drug concentration through evaporation.
The agent is applied transungually, specifically to the dorsal aspect of the nail.
These treatments are generally well-tolerated, with minimal adverse effects like periungual erythema and a mild burning sensation at the application site.
However, they typically require prolonged treatment durations and may be less effective due to limited penetration through the nail plate.
Indications for topical antifungal agents:
- In combination with oral therapy as an adjunctive to increase cure rate.
- When oral antifungal agents are contraindicated or cannot be tolerated.
- May consider as monotherapy when < 50% of the nail is affected without matrix involvement & only a few (< 3 nails) are infected.
- As long-term prophylactic agent.
Commonly available topical agents: Cilopirox 8%, Amorolfine 5%, Efinaconazole 10%, Tavaborole 5%, Terbinafine 10%
Some of the dosing regimen:
- Ciclopirox 8%: Applied daily on nail for 4 months.
- Amorolfine 5%: Applied once weekly, 6 months (for fingernails) and 12 months (for toenails)
Concurrent nail polish should be avoided due to potential undesirable cosmetic changes.
Children tend to respond better to topical antifungals due to their faster nail growth & thinner nail plate. (The oral antifungal agents like terbinafine and itraconazole are not formally approved for paediatric use in onychomycosis, though off-label use may be considered based on weight-adjusted dosing.)
Miscellaneous
- Nail abrasion, trimming, avulsion, & debridement can be performed, if necessary to enhance topical penetration of antifungal agents & reduce fungal load.
- White superficial onychomycosis can be treated by mechanical removal (e.g. scraping) of the involved area followed by topical antifungal therapy (vide supra)
- Keratolytic agents e.g. urea, salicylic acid may enhance the delivery of topical antifungal agents into the nails
Novel therapies
These include:
- Laser & photodynamic therapy
- Novel antifungals e.g. ravuconazole, posaconazole
- Nonthermal plasma, ultrasound-enhanced drug delivery, nanoparticles
- Natural remedies (e.g. propolis, tea tree oil) – needs further validation.
Prognosis
Superficial white onychomycosis has the best prognosis.
Factors that predict poorer prognosis may include:
- Larger area of nail involvement
- Total dystrophic type
- Involvement of the lateral edge of the nail
- Presence of subungual hyperkeratosis
- Dermatophytoma
- Older age
- Immunosuppression
- Poor peripheral circulation
- Non-dermatophyte infection
Prevention and Recurrence of Onychomycosis
Prevention strategies
Wear non-occlusive (breathable) footwear
Keep feet clean and dry
Trim nails short regularly
Treat tinea pedis if present
Screen and treat family members with tinea pedis or onychomycosis
Recurrence
May occur as:
- Relapse – due to inadequate or inappropriate treatment
- Re-infection – new infection after completing treatment
To reduce recurrence risk,
- Maintain proper foot hygiene
- Keep nails short and feet dry
- Consider regular topical antifungal use as post-treatment prophylaxis.
Complications
Some of the complications that can be associated with onychomycosis include:
- Infective complications
– As a reservoir for cutaneous fungal infections e.g. tinea pedis, tinea corporis, tinea cruris.
– Increased risk for bacterial infections e.g. cellulitis & paronychia - Functional impairment: May interfere with mobility & daily activities (e.g. standing, walking, wearing shoes)
- Physical symptoms: Discomfort, pain, paresthesia, nail deformities (e.g. thickening, dystrophy)
- Psychosocial impact: Social embarrassment due to nail appearance
Regarding Non-Dermatophyte Mold (NDM) in Onychomycosis
NDM Significance: Poses a diagnostic dilemma as they are sometimes considered as contaminants.
Diagnosis requires repeat cultures, direct microscopy, and strong clinical correlation to determine its significance.
6 criteria to support the diagnosis of NDM onychomycosis:
- Positive direct microscopy (KOH)
- Absence of a dermatophyte in culture
- Growth of non-dermatophyte mould in culture
- Similar growth of the causative agent in repeat culture
- Positive inoculum count
- Positive histology
Definitive diagnosis: 3 out of 6 required; 2 of which must include microscopy and culture.
Primary Care Tip: Microscopy identification plus consistent culture of the same organism can confirm NDM causation.
💊 Treatment
- Limited Options: No single definitive therapy for NDMs.
- Recommended Agents:
– Terbinafine & Itraconazole: Effective for Scopulariopsis brevicaulis and Aspergillus spp.
– Topical Ciclopirox: May help with Scopulariopsis infections. - Treatment Approach: Consider systemic, topical, and mechanical (nail avulsion) combination therapies.
References
- Leung AKC, Lam JM, Leong KF, Hon KL, Barankin B, Leung AAM, Wong AHC. Onychomycosis: An Updated Review. Recent Pat Inflamm Allergy Drug Discov. 2020;14(1):32-45. doi: 10.2174/1872213X13666191026090713. PMID: 31738146; PMCID: PMC7509699. From <https://pmc.ncbi.nlm.nih.gov/articles/PMC7509699/>
- Leelavathi M, Noorlaily M. Onychomycosis nailed. Malays Fam Physician. 2014 Apr 30;9(1):2-7. PMID: 25606290; PMCID: PMC4265967.
- National Antimicrobial Guidelines (NAG). Ministry of Health Malaysia. 2024.
- Gupta, A. K., Venkataraman, M., Shear, N. H., & Piguet, V. (2020). Onychomycosis in children – review on treatment and management strategies. Journal of Dermatological Treatment, 33(3), 1213–1224. https://doi.org/10.1080/09546634.2020.1810607
