Young hypertension

Young Hypertension
Generally refers to those ≥ 18 years and < 40 years of age (though there may be some variation in regarding the age according to different guidelines)
The ACC/AHA guidelines have lowered the diagnostic threshold of hypertension since their 2017 guidelines where BP above 130/80 are categorized as stage 1 and above 140/90 as stage 2.
Nevertheless, our Malaysia CPG guidelines still maintain the conventional diagnostic threshold where stage 1 is only diagnosed if BP ≥ 140/90. This is similar to that of the ESC (2018) & NICE (2019) guidelines
|
Blood pressure |
120-129/80 |
SBP 130-139 or DBP, 80-89 |
SBP ≥ 140 or DBP ≥ 90 |
BP ≥ 160-179/100-109 |
SBP ≥ 180 or DBP ≥ 110 |
|---|---|---|---|---|---|
|
Classification | |||||
|
ACC/AHA (2017) |
Elevated |
Stage 1 |
Stage 2 |
Stage 2 |
Stage 2 |
|
ESC (2018) |
High normal |
Grade 1 |
Grade 2 |
Grade 3 | |
|
NICE NG136 (2019) |
Stage 1 |
Stage 2 |
Severe | ||
|
Malaysia CPG (2018) |
At risk |
Stage 1 |
Stage 2 |
Stage 3 (Severe) |
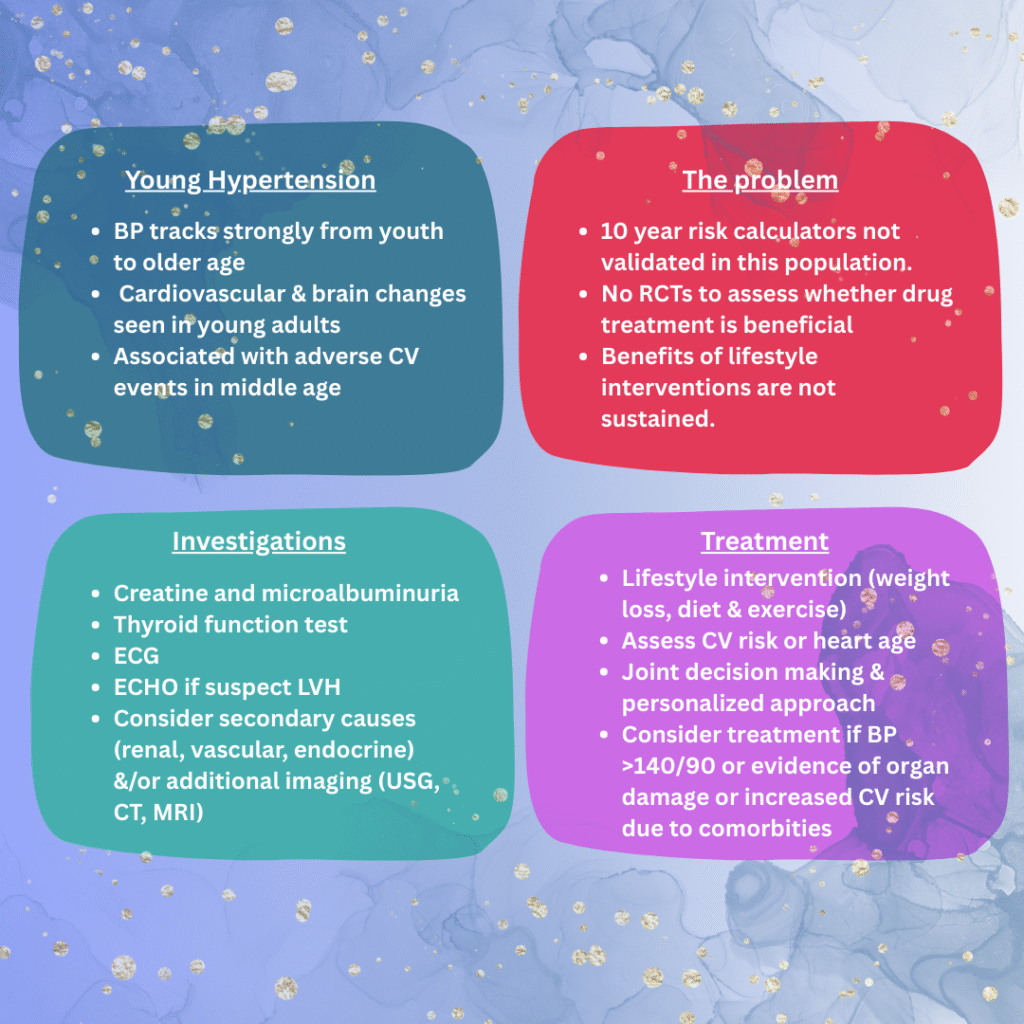
Why is it important to address the issues of young hypertension?
It increases the risk of CV events in middle age and earlier onset of MI, stroke, TIA and heart failure.
Those with elevated BP when they are young are likely to have elevated BP later on.
The short term implications may be associated with disruption of the cardiovascular and brain health where they may have higher rate of left ventricular hypertrophy and/or alteration of brain volume and white matter hyperintensity volume.
Investigation
The main purpose for investigation is 1) To investigate for any secondary cause (if clinical history and physical examination are suggestive. 2) To assess for any complications of hypertension. 3) To assess for any other CV risk factors (e.g. DM, dyslipidemia)
Secondary causes of hypertension may include :
- Parenchymal renal disease
- Renovascular disease (may be secondary to fibromuscular dysplasia or atherosclerosis)
- Sleep apnoea
- Endocrine disorders – Primary aldosteronism, Cushing syndrome, Phaeochromocytoma, Acromegaly, Thyroid disease, Parathyroid disease
- Drug-induced or related (e.g. OCP, Steroids, NSAIDs, Erythropoietin)
- Coarctation of aorta
- Takayasu arteritis
Investigations should be according to the suspicion of underlying secondary cause e.g. USG to assess for renal parenchymal disease, CTA renal TRO renovascular disease, etc.
These predictors may serve as a guide to suspect secondary causes & may warrant referral to secondary/tertiary care for further assessment.
- Age < 30 year old with no risk factors
- Resistant hypertension
- Sudden deterioration in BP control
- Evidence of end-organ damage
Investigations to assess for complications of hypertension & other CV risk factors are similar to that of the usual guideline, including but not limited to :
- ECG – to identify LVH changes (The European guideline recommend echocardiography to assess for LVH as ECG has limited sensitivity. Alternatively, cardiac MRI may also be considered.)
- Renal profile
- Microalbuminuria – to assess for subclinical renal damage
- Lipid profile
- Blood glucose
Risk-based approach
When managing hypertension, stratifying patient according to their 10 year cardiovascular risk is important to guide initiation of treatment. This can be achieved by various tools, including Atherosclerotic Cardiovascular Disease (ASCVD) risk calculator from AHA/ACC, Systemic Coronary Risk Evaluation system (SCORE2) from ESC guidelines and QRISK3 score utilized by UK guidelines.
The issue when employing this approach is that these tools are validated mainly for age group 40 and above, with the exception of QRISK3 score in which it can be used for 25 years and above.
Our Malaysia CPG guideline recommends Framingham risk scoring or Risk stratification table that take into account patient’s BP, target organ damage (LVH, retinopathy, proteinuria) and/or complications (heart failure, renal failure), and other CV risk factors.
The issue when adapting risk-based approach in young hypertensive is that the 10-year CV risk is often low, irrespective of other risk factors, despite their substantially increased lifetime risk of CV events.
Treatment
|
Blood pressure |
120-129/80 |
SBP 130-139 or DBP, 80-89 |
SBP ≥ 140 or DBP ≥ 90 |
BP ≥ 160-179/100-109 |
SBP ≥ 180 or DBP ≥ 110 |
|---|---|---|---|---|---|
|
Treatment threshold | |||||
|
ACC/AHA (2017) |
Lifestyle |
Treat if CVD or 10 yr ASCVD risk > 10% |
Treat |
Treat |
Treat |
|
ESC (2018) |
Lifestyle advice but treat if high risk |
Low-moderate risk: Treat if lifestyle fails High risk: Treat |
Treat |
Treat | |
|
NICE NG136 (2019) |
OD/CVD, DM, or 10 yr CV risk > 10% |
Treat |
Treat |
Lifestyle interventions are recommended to address the risk factors, although the benefits appear to be short-term.
Starting antihypertensive
- ACC/AHA and ESC guidelines – thiazide diuretics, CCB, ACEi, ARB and beta blockers are equally effective in older & younger individuals < 65 years of age. They do not advocate any specific starting agent among the different class group.
- NICE guideline – ACEi or ARB are recommended for those < 55 years of age except those of black African or African-Caribbean family origin in whom CCBs are recommended.
There is a section in our Malaysia CPG guideline on managing hypertension in children & adolescent, but there are no specific guidelines in regards to young hypertension.
Another important point to consider while treating young hypertension is in relation to treating women of childbearing age. ACEi and ARBs should be avoided in pregnancy due to risk of adverse fetal outcomes. If pregnancy is unplanned, ACEi and ARBs should be withdrawn promptly and other antihypertensives (e.g. labetalol, nifedipine or methyldopa) should be initiated.
Young hypertension in a nutshell