Scabies

Scabies
General features
Causative agent (mite) : Sarcoptes scabiei var. hominis
Transmission: Skin-to-skin contact, including sexual activity. May also sometimes be transmitted via fomites, e.g. beddings (less common)
Incubation period:
– Without previous exposure: 2 – 6 weeks
– With previous infestation: develop symptoms within 1 – 5 days of re-exposure
Life cycle of Sarcoptes scabiei
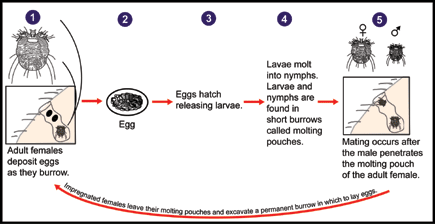
The male mite fertilises the female mite & dies shortly after mating.
The female mite then burrows into the stratum corneum where they lay 2 – 3 eggs per day. They continue to burrow at a rate of 0.5 – 5 mm per day for its 4 – 8 weeks of lifespan.
The eggs hatch into larvae which then mature into adult mites in about 3 weeks and the cycles continue.
The itching and rash are due to allergic reaction (TH1-mediated hypersensitivity) towards the various mite-related antigens.
Clinical features
1. Main symptom is itch – generalized, intense and worse at night.
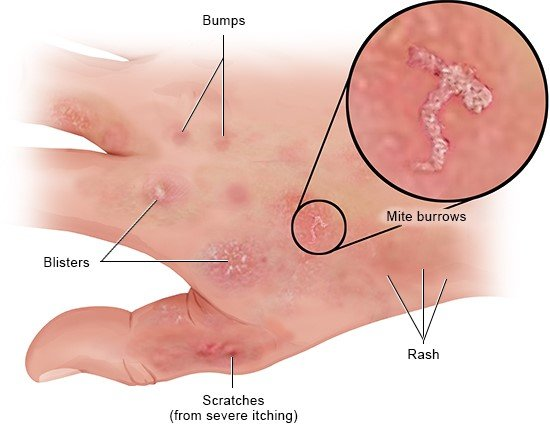
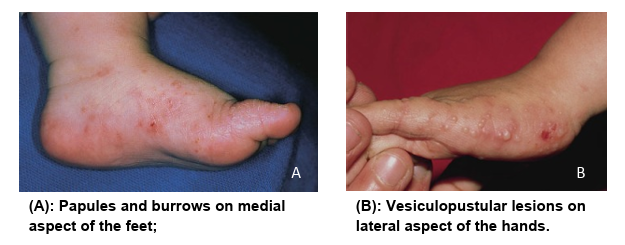
2. Erythematous papulovesicular lesions
- Common site: anterior axillary folds, nipple area, periumbilical skin, elbows, volar surface of the wrists, interdigital web spaces, belt line, thighs, buttocks, penis, scrotum, ankles
- In adults, often the face, neck and head are spared, whereas in infants, children, elderly and immunocompromised, these sites are common and may include the scalp, palms & soles.
- There may be associated excoriations, scratch marks or dermatitis.
3. Burrows – seen as a serpiginous tract that measure around 1 cm in length
- Common site: finger webs, wrists, feet, axillae, umbilicus, male genitalia & breast areolas in women.
- In infants & children: palms and soles, sides of the feet, head (especially post auricular fold)
4. Nodules
- Vary in size
- May be seen in the scrotum and penis in men and around the areolae in women.
- Other sites include axillae, gluteal folds, upper thighs.
Variants
A. Crusted (Norwegian) scabies
Uncommon.
Due to altered immune response leading to uncontrolled proliferation of mites (thousands & millions of mites compared to 10 – 15 in classical scabies.
Highly contagious
Risk factors: immunocompromised individuals, neurologically impaired individuals. [May also occur in healthy individuals]
Characteristic features: Diffuse hyperkeratosis (more severe on the palms and soles, under the fingernails, on the ears, trunks & extremities) with variable degree of underlying erythroderma. Itching may be minimal or absent.
Usually seen in elderly males.
May be due to secondary infection with Staph. aureus or due to autoantibody response.
Bullae may be tense of flaccid.

Federico, Massimo & Mellick, Larry. (2010). Norwegian Scabies: A Challenging Dermatologic Condition. The Open Emergency Medicine Journal. 310. 25-26. 10.2174/1876542401003010025.

Cardoso, Alberto & Cardoso, Alberto & Talhari, Carolina & Santos, Monica. (2019). Update on parasitic dermatoses. Anais Brasileiros de Dermatologia. 95. 10.1016/j.abd.2019.12.001.

B. Nodular scabies
May be due to local hypersensitivity reaction to dead mites or secondary to persistent infection.
Common sites: male genitalia & breast (may be widespread in infants).
Other sites may include: axillae, buttocks
May persist for months despite successful treatment

C. Scabies incognito
Atypical clinical picture secondary to inappropriate use of steroids.
Diagnosis
Generally depends on patient’s history and physical examination (characteristic sites, burrows, nodules, etc).
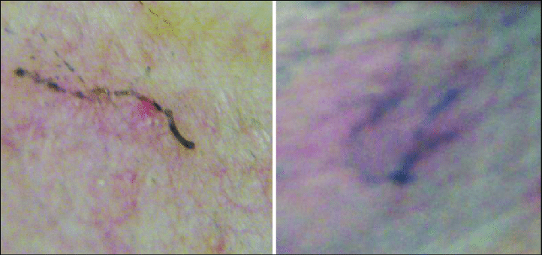
Definitive diagnosis is by demonstration of the mite, eggs, or scybala (fecal pellets of mites) via dermatoscopy &/or digital photography.
Skin scrapings using blade/needle/adhesive tape from suspicious lesion may allow visualization of mites eggs/feces under microscope.
Burrow ink test (using ink from fountain/surgical marking pen):
- Rubbing ink on suspected burrow and removing the excess ink using alcohol swab.
- The ink may be visualized tracking into the burrow (classical zigzag line) indicating the presence of burrow
The 2020 International Alliance for the Control of Scabies Consensus Criteria for the Diagnosis of Scabies
This criteria is used only for classical scabies in otherwise healthy individuals and is not applicable in atypical/variant scabies, immunocompromised individuals, elderly, cognitive impaired or bedridden individuals.
A. Confirmed scabies
At least one of :
- A1: Mites, eggs or faeces on light microscopy of skin samples
- A2: Mites, eggs or faeces visualized on an individual using a high‐powered imaging device
- A3: Mite visualized on an individual using dermoscopy
B. Clinical scabies
At least one of :
- B1: Scabies burrows
- B2: Typical lesions affecting male genitalia
- B3: Typical lesions in a typical distribution and two history features
C. Suspected scabies
At least one of :
- C1: Typical lesions in a typical distribution and one history feature
- C2: Atypical lesions or atypical distribution and two history features
History features
- H1: Itch
- H2: Positive contact history
Diagnosis can be made at any of the three levels (A, B or C). A diagnosis of clinical or suspected scabies should only be made if other differential diagnosis are less likely.
References: Engelman D, Yoshizumi J, Hay RJ, Osti M, et al. The 2020 International Alliance for the Control of Scabies Consensus Criteria for the Diagnosis of Scabies. Br J Dermatol. 2020 Nov;183(5):808-820. doi: 10.1111/bjd.18943. Epub 2020 Mar 29. PMID: 32034956; PMCID: PMC7687112.
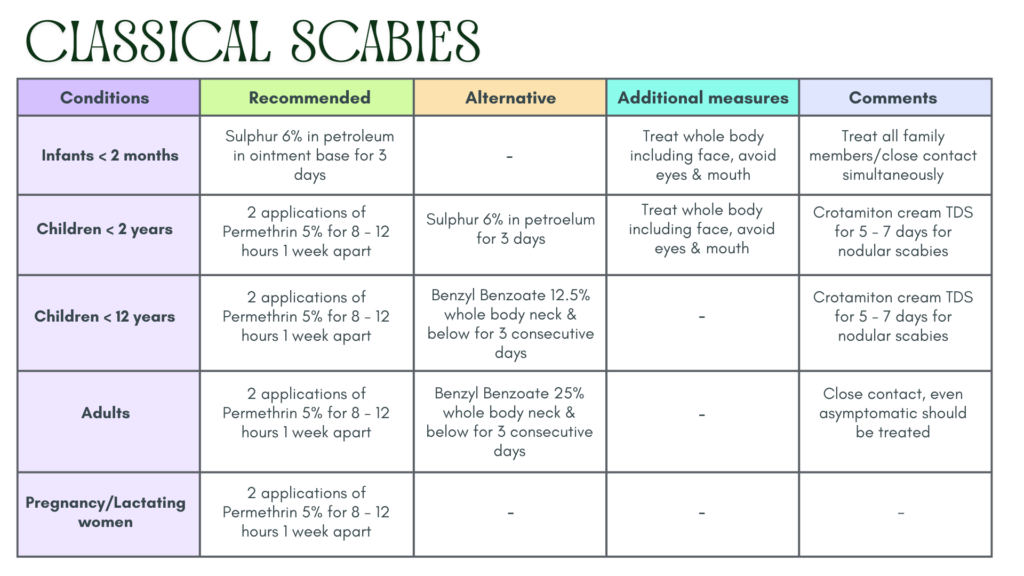
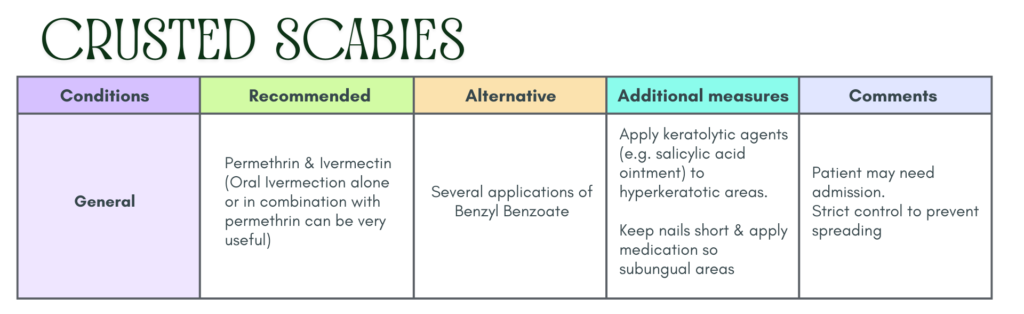
Treatment
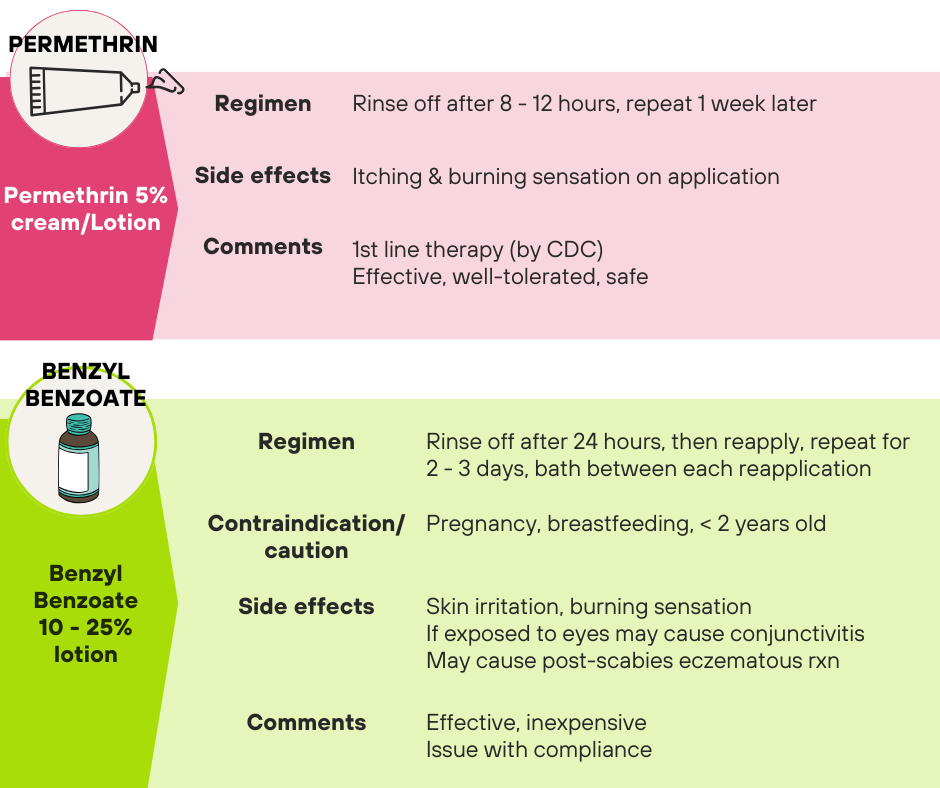
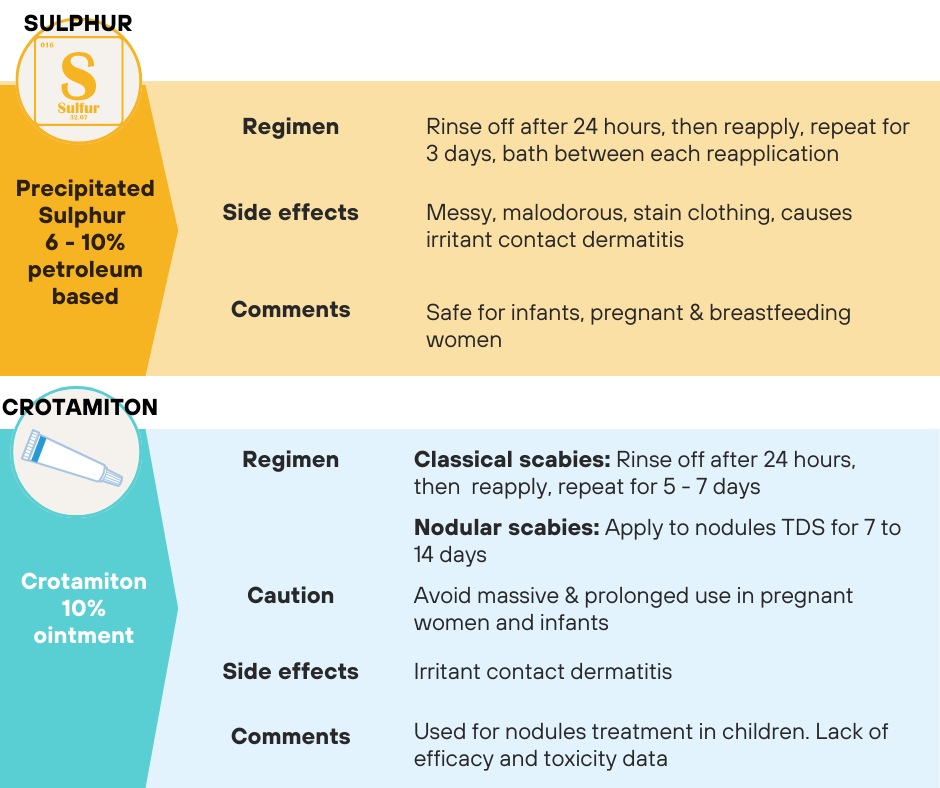
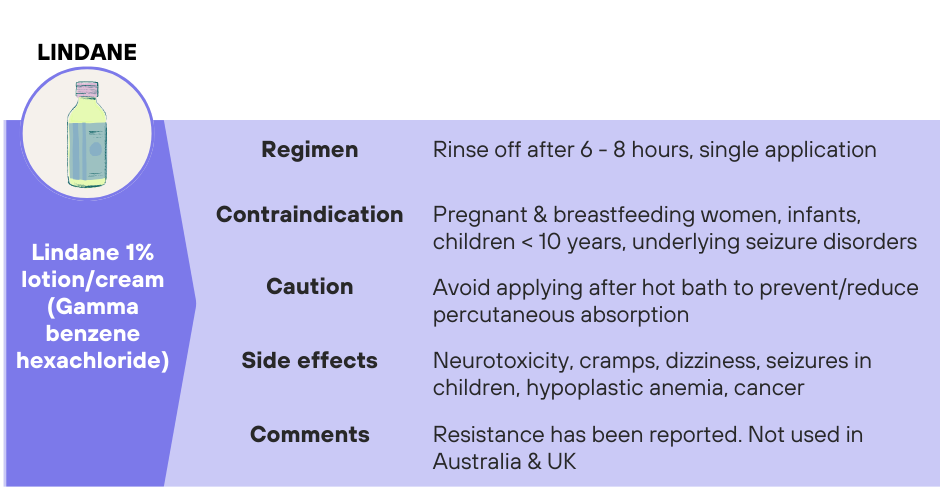
Topical treatment
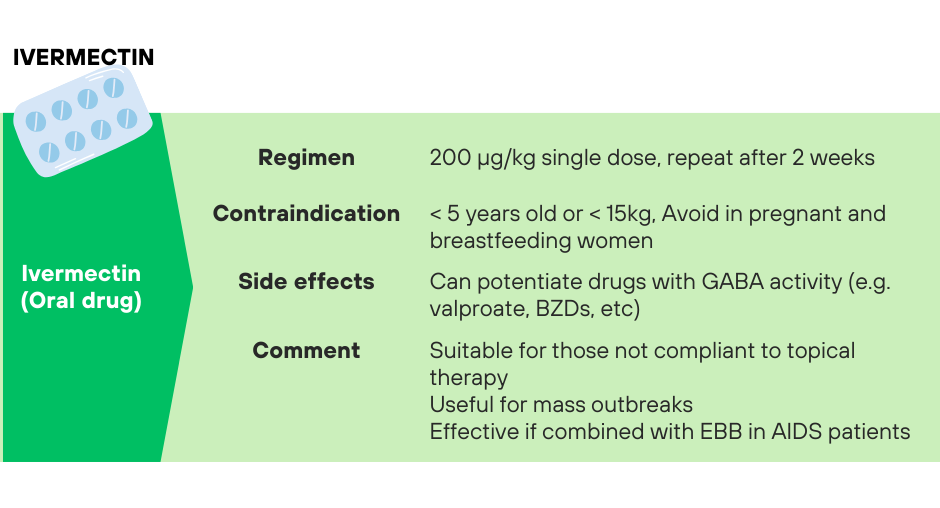
Oral treatment – Ivermectin
Treatment according to specific considerations
Further treatment to consider
Secondary bacterial infection
Systemic antibiotics that cover Gram +ve organisms for at least 7 days. Topical antibiotics are not required for those already started on systemic antibiotics.
Antiseptic wash/soaks e.g. KMnO4 (1:10,000) in impetiginized scabies.
Nodular scabies
May apply on individual nodules:
- Topical anti-inflammatory agents, e.g. topical corticosteroids (mid potent to potent) for 2 weeks.
- Crotamiton cream BD for 7 – 14 days.
Persistent itching
Itching can persists 1 – 2 weeks after successful treatment.
If persistent itching is present, consider: cutaneous irritation, allergic contact dermatitis due to medications, post-scabetic eczema or possible treatment failure.
Treatment options:
- Antihistamines
- Corticosteroids – topical or short course of oral steroids (0.5 mg/kg depending on severity)
- Emollients – for dry & eczematous skin
Treatment of contact
Definition of contact: Prolonged skin-to-skin contact (> 10 mins on any one occasion) over the previous 2 months.
Members of the affected household and all close contact should be treated at the same time, even when asymptomatic.
Regimen (same as the treated patient):
- For most, one treatment is sufficient.
- For symptomatic contacts, two treatments are required (permethrin 5%)
Treatment of fomites 👕👖
These include underwear, clothing, towels, bed linen, slippers, etc used by the affected person in the 72 hours prior to treatment.
Treatment options:
- Laundered using a hot wash cycle (> 50 °C ) or hot tumble dried to kill the mites 🔥
- Alternatively, place in a plastic bag & leave them for 72 hours before airing and reusing
Vacuum/iron/steam clean mattresses thoroughly.
Amenities like toilets and chairs should not be shared (until 24 hours after the first treatment)
Follow up
Repeat visits at 2 weeks and 4 weeks after initial treatment are recommended. Lesions usually heal by one month.
If symptoms re-appear, patient can be retreated when necessary.
Treatment failure
Signs of treatment failure:
- Appearance of new vesicles/papules/burrow at any stage after completing a course of scabicide.
- Persistent itch ≥ 6 weeks after first course of treatment of scabicide
Possible cause:
- Improper & inadequate application of scabicide.
- Allergic contact dermatitis to scabicides should be excluded.
- Reinfestation due to failure of simultaneous treatment of family members/contact.
Treatment options:
- Re-treat with alternative topical scabicides.
- Re-educate and re-counsel patient & family members.
Indications for referral
- Diagnosis uncertainty
- Failure of optimized treatment of patient and contacts
- Patients with complications like severe infection
References
- Ministry of Health Malaysia. (2015). Guideline for management of scabies in adults and children(MOH/P/PAK/286.14(GU)). Medical Development Division.
- Engelman D, Yoshizumi J, Hay RJ, Osti M, et al. The 2020 International Alliance for the Control of Scabies Consensus Criteria for the Diagnosis of Scabies. Br J Dermatol. 2020 November; 183(5):808 – 820. doi: 10.1111/bjd.18943. Epub 2020 Mar 29. PMID: 32034956; PMCID: PMC 7687112
