Rhinosinusitis
Definition
Inflammation of the nose & the paranasal sinus (PNS) characterised by 2 or more Sx, one of which should be either nasal blockage/obstruction/congestion or nasal discharge (anterior/posterior nasal drip):
+- facial pain/pressure
+- reduction or loss of smell.
AND at least one of the following;
Endoscopic signs of:
– Nasal polyps, &/or
– Mucopurulent discharge primarily from middle meatus &/or
– Oedema/mucosal obstruction primarily in middle meatus.
CT changes:
– Mucosal changes within the ostiomeatal complex &/or sinuses.
Past medical h/o CRS (medically diagnosed)
– In primary care, obtaining a past medical h/o CRS is sufficient to make a diagnosis.
Predisposing/risk factors
- Smoking (active & passive)
- Family history of chronic rhinosinusitis, asthma
- GERD
- Infection
- Allergies
Classification
Duration⌚
a) Acute rhinosinusitis(ARS):
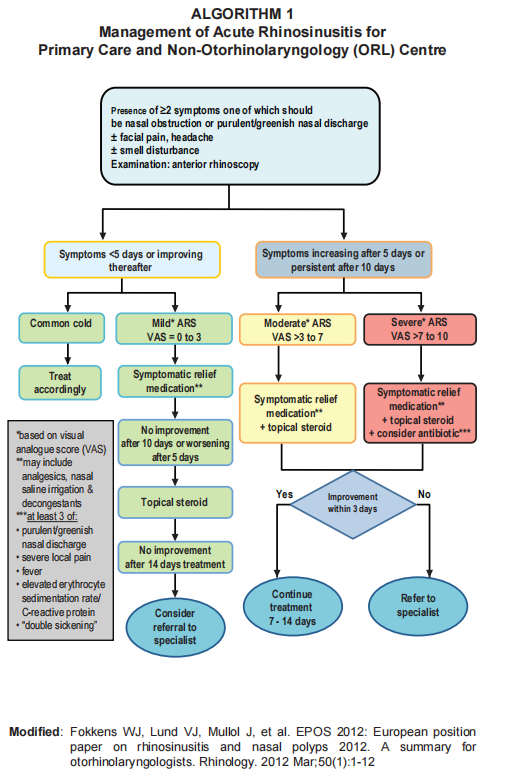
– Defined as worsening symptoms after 5 days or symptoms persist after 10 days and < 12 weeks.
– If the duration of symptoms is < 5 days, it is diagnosed as acute viral rhinosinusitis (common cold)
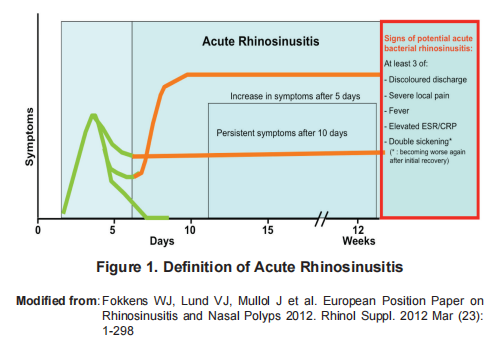
Majority of ARS are viral in origin.
Acute bacterial rhinosinusitis is suggested when there are at least 3 SSx of:
- Discoloured discharge (with unilateral predominance) & purulent secretion in the nasal cavity.
- Severe local pain (with unilateral predominance)
- Fever (> 38 degrees)
- Elevated ESR/CRP
- Deterioration of SSx after recovering (‘Double Sickening’): Pt often report having a cold that was getting better but then they started feeling worse again.
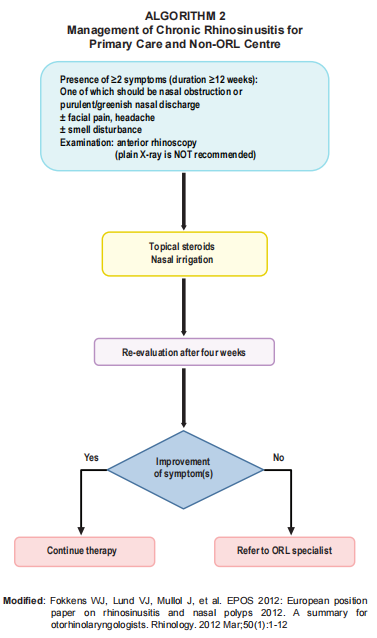
b) Chronic rhinosinusitis(CRS): Symptoms > 12 weeks.
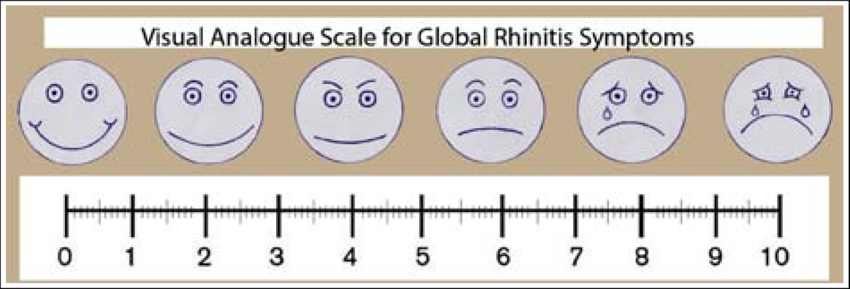
Severity
Severity of RS can be divided into the following based on total severity visual analogue scale (VAS) score
- Mild = 0 – 3
- Moderate = >3 – 7
- Severe = > 7 – 10
Clinical presentation
- Nasal obstruction
- Rhinorrhea
- Headache
- Decreased sense of smell
- Postnasal drip
- Facial pressure or pain
- Fever
- Sore throat
- Cough
Assessment
Anterior rhinoscopy should be performed as part of clinical assessment of suspected acute rhinosinusitis in primary care setting (albeit a rather limited role).
– May reveal: mucosal oedema, nasal inflammation, purulent nasal discharge, polyps & anatomical abnormalities.
Nasal endoscopy should be performed to diagnosed rhinosinusitis at otorhinolaringology center (not required in diagnosing ARS in primary care)
Imaging ☢️
Plain radiograph has no role.
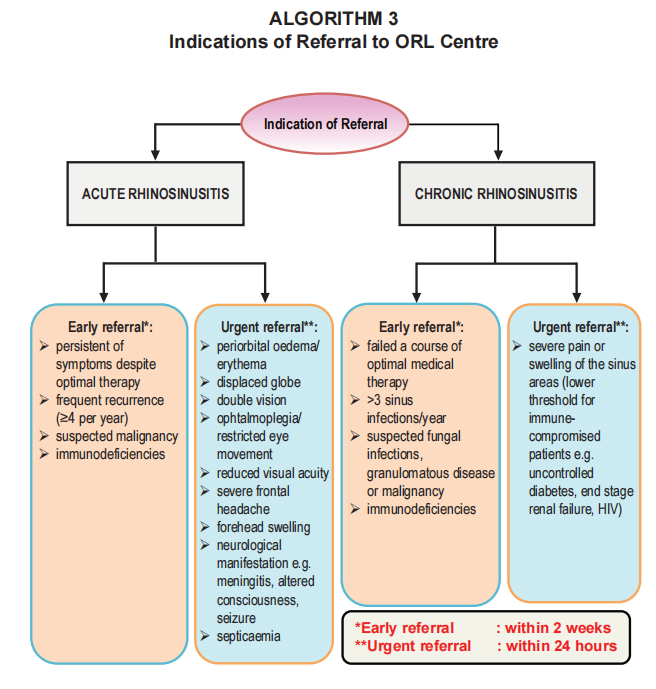
CT scan is the gold standard for evaluation of paranasal sinus (PNS) and is indicated when:
– Failed medical therapy
– Planned for surgery
– Atypical or severe disease or complications are suspected: unilateral Sx, blood-stained discharge, displacement of the eye & severe pain.
MRI may be useful in cases of diagnostic uncertainty or when intracranial complications are suspected.
Laboratory tests
Culture and sensitivity (C&S) may be considered in patient who do not respond to Abx treatment after 72 hours in ARS .
Nasal swab should not be performed, rather endoscopically-directed middle meatal culture should be used to obtain specimen for C&S.
Common pathogen involved in RS:
- 2 main causative agents in acute bacterial RS:
– Strep. Pneumoniae
– H. influenzae - Moraxella catarrhalis: more common in children.
- In CRS:
– Staph. aureus
– Enterobacteriaceae spp
– Pseudomonas spp - Anaerobic organisms are predominant in acute sinusitis with dental origin.
Differential diagnosis

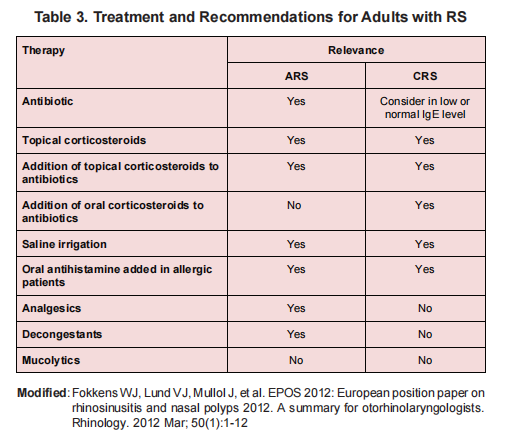
Pharmacological management
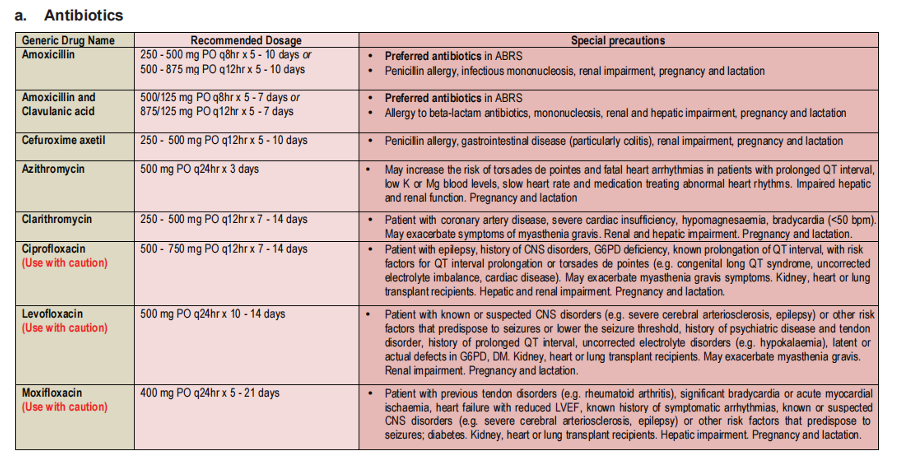
a) Antibiotics – only in acute bacterial RS
The preferred Abx:
– Amoxicillin 500 mg TDS x 5 – 7 days OR
– Augmentin 625 mg TDS x 5 – 7 days.
Abx should not be used routinely in chronic rhinosinusitis.
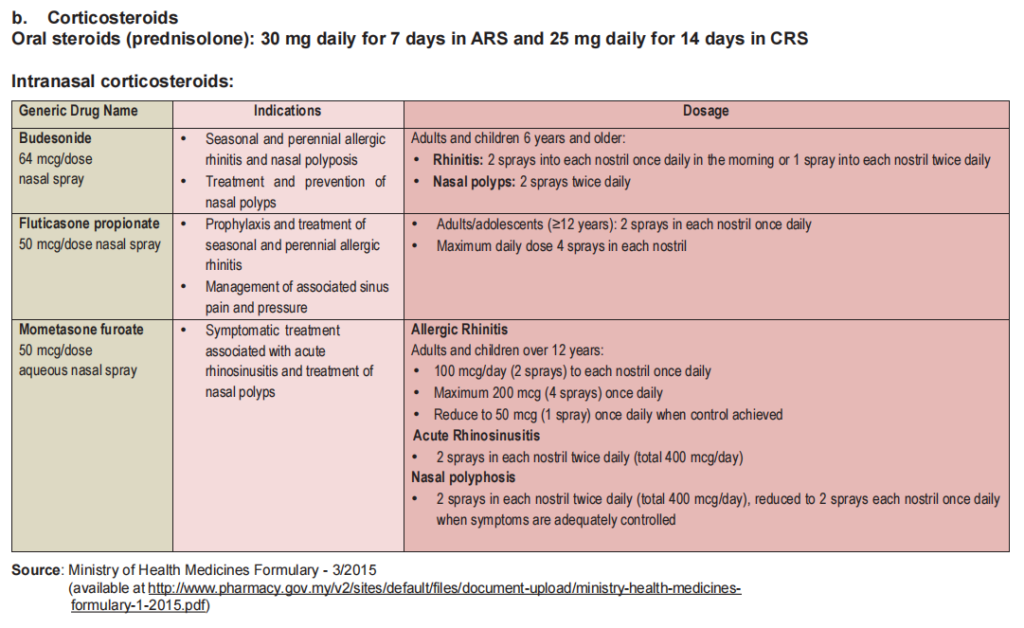
b) Corticosteroids
Intranasal corticosteroids:
– Should be considered for 14 – 21 days in ARS
– Should be given for 16 – 52 weeks in CRS
Short term oral corticosteroids should ONLY be given in CRS in ORL center.
In local practice, oral corticosteroids are not given in ARS due to the possibility of exacerbation of bacterial infection.
c) Nasal saline irrigation
– Should be used as an adjunct therapy.
– Facilitates mechanical removal of mucus, infective agents & inflammatory mediators.
– Also decreases crusting in the nasal cavity & increases mucociliary clearance.
In local practice, oral corticosteroids are not given in ARS due to the possibility of exacerbation of bacterial infection.
d) Antihistamines
– Should be prescribed if there are associated symptoms suggestive of allergic rhinitis (e.g. sneezing, nasal itchiness, nasal obstruction & rhinorrhoea).
e) Other medications
Analgesics: PCM or NSAIDs
Decongestants:
– Topical decongestants should not be prescribed for > 2 weeks due to rebound phenomenon.
– Oral decongestants should be cautiously prescribed in those with medical conditions e.g. DM, CV disease, glaucoma & BPH.
Treatment recommendations
Surgical management
Indications for surgery in ARS:
– Presence of orbital or intracranial abscess on CT scan OR
– No clinical improvement after 24 – 48 hours of IV antibiotics.
Functional endoscopic sinus surgery (FESS) should be offered in patient with CRS who fail optimal medical treatment.
Algorithm