Obesity (Adult)
Obesity
Diagnosis
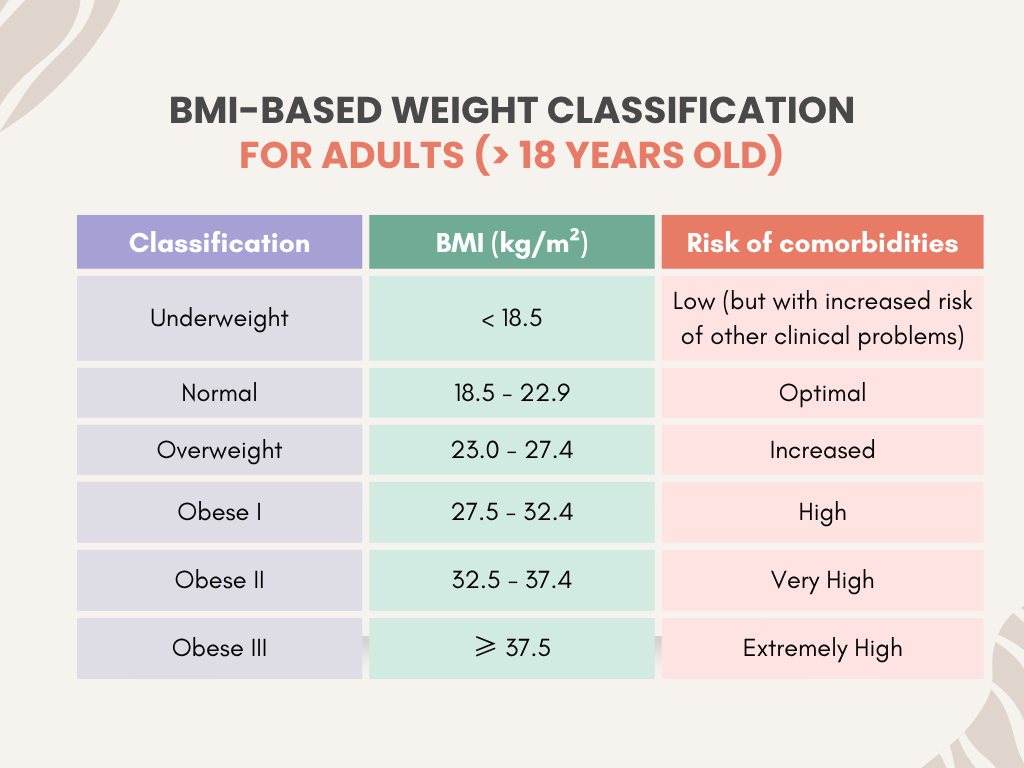
The Body Mass Index (BMI) has been widely accepted as a means of measurement of obesity as recommended by WHO.
BMI = Weight (kg)/Height² (m²)
A lower BMI cut-off points for overweight and obesity are employed for the Asian population in comparison to the Caucasians. This is due to the fact that Asians generally have higher body fat percentages compared to Caucasians at similar BMI cut-off points, which can be interpreted as having higher CV risks at similar BMI cut-off points.
Limitations of BMI
- Does not distinguish weight between muscle & fat. The elderly may have a misclassification of healthy BMI where in truth they have a higher body fat composition due to age-related loss of lean body mass (sarcopenia)
- It also does not distinguish body fat distribution where abdominal or visceral fat is an known determinant and independent risk factors for cardiovascular disease.
In view of this limitation, waist circumference (WC) measurement has been recommended in combination with BMI in assessing overweight & obesity.
Waist circumference (WC) measurement
- Measured in the horizontal plane, midway between the lowest ribs & the iliac crest.
- Correlates well with abdominal fat content irrespective of BMI
- Most useful in individuals who are in the normal & overweight BMI-based categories.
- It is unnecessary to measure WC in those with BMI > 35 kg/m2 as it loses its predictive value.
The WHO recommends WC of ≥ 102 cm in men and ≥ 88 cm in women.
Asian countries may use cut off points of 90 cm in men & 80 cm in women (Studies have showed high prevalence of T2DM and CVD at these cut off values)
Obesity-related medical conditions
Obesity has been a rising concern due to its increased prevalence and subsequent related medical conditions which include, but not limited to:
- Hypertension
- T2DM and prediabetes
- Metabolic syndrome
- Dyslipidemia
- Obstructive sleep apnea (OSA)
- Osteoarthritis/Degenerative joints/Back pain
- Metabolic associated-dysfunction fatty liver disease (MAFLD)
- GERD
- Cancer
Management of Obesity
Principal goals:
- Prevent complications by keeping patient metabolically healthy
- Prevent/treat existing comorbidities
- Fight against stigmatization of people with obesity
- Restore individual’s well-being, positive body image & self-esteem
Psychological & Behavioral Intervention
When managing a patient with obesity, we need to take into account not only the physical aspect but also the mental aspect of the individual.
The psychological aspect of obesity:
- May be associated with various mental health issues e.g. weight bias, stigma & discrimination with prejudice & stereotype labelling like being lazy, unmotivated, lacking willpower & discipline.
- Mental health consequences: Body image dissatisfaction, reduced quality of life, low self-esteem, poor overall wellbeing.
- Individuals may also have pre-existing mental health issues.
Interventions
Most are cognitive-based & often used together with lifestyle modification.
Multicomponent approaches:
- Enhancing communication & avoiding stigmatization.
– Communicate with empathy without negative judgement & bias (acknowledged that they may have already been exposed to negative experiences like discrimination).
– Asking permission from the individual first to speak about their weight.
– Avoid the use of inappropriate or hurtful words.
– Avoid blaming by keeping in mind that obesity has a complex multifactorial etiology & that it may not fully be under voluntary control. - Psychoeducation – to achieve behavioral & psychological goals to improve overall health & not just amount of weight loss.
- Motivational interviewing
- Behavioral strategies – to improve adherence to lifestyle intervention programmes.
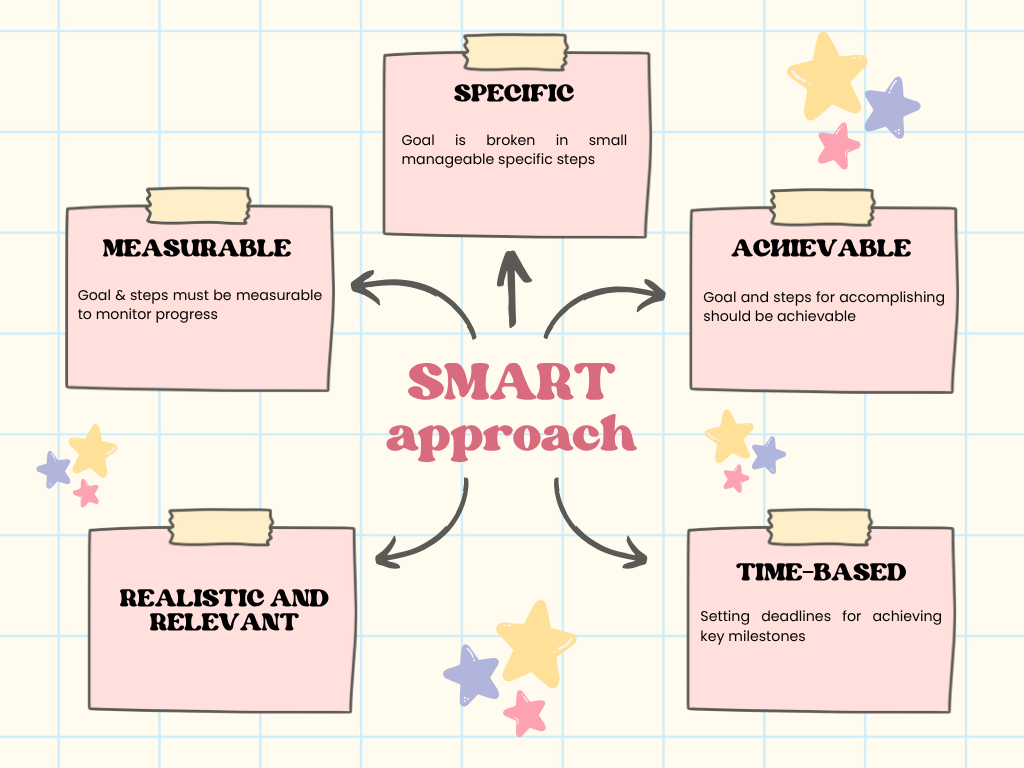
Example: Goal setting & action planning using SMART approach
- Psychological interventions – Cognitive Behavioral Therapy (CBT), Acceptance & Commitment Therapy
Comprehensive lifestyle modifications
Consists dietary & activity habits.
Aim: To achieve weight loss by decrease in consumed calories & increased energy expenditure (negative energy balance)
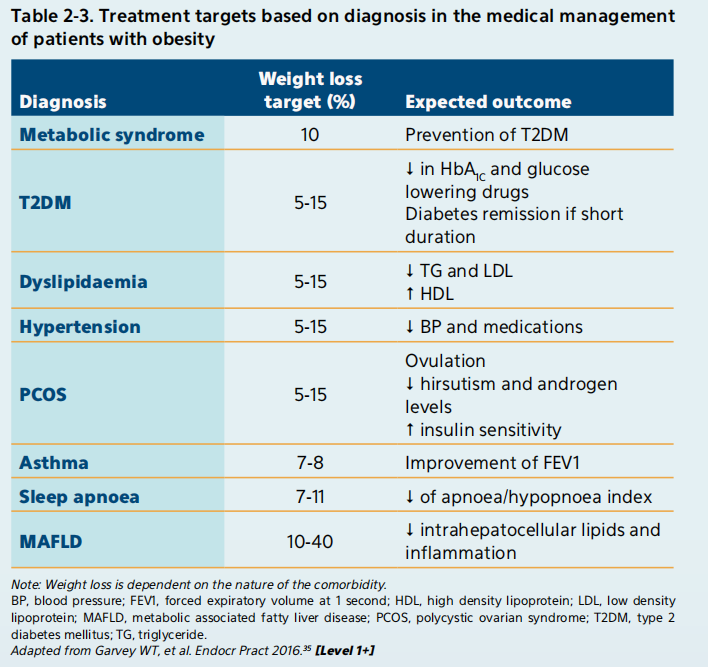
Weight loss goals
- A sustained weight loss of 3 – 5 % is likely to result in clinically meaningful improvement in metabolic outcomes.
- Realistic weight loss goals:
– Up to 1 kg per week
– Up to 10% of baseline body weight
– A total of 3 – 5% of baseline body weight in the presence of CV risk factors (e.g. HTN, hyperglycemia & hyperlipidemia)
Calorie restriction
Diet should be individualized accordingly based on sex, age, physical activity level, comorbidities & patient preference.
Suggested strategies to achieve an initial weight loss of 0.5 – 1 kg/week:
- 1,200 – 1,500 kcal/day for women
- 1,500 – 1,800 kcal/day for men
- Reduce daily energy by 500 – 700 kcal from the usual daily intake.
Very low calorie diet (i.e. < 800 kcal/day) should only be done under medical supervision which involve also a dietitian.
Low fat or low carbohydrate diet have been found to help reduce weight, waist circumference, body fat percentage and improve metabolic profile (e.g. lipid, glucose, BP)
Alternative methods of calorie restrictions include meal replacement or intermittent fasting.
For intermittent fasting, the degree of weight loss depends on the cumulative caloric restriction & not the duration of the fast and may include:
- Time restrictive diets: Restricting the no. of hours of eating per day OR
- Alternate day fasting: Restriction of calorie consumed during fasting and non-fasting days.
Physical activity
Should be integrated with other components of lifestyle modification e.g. calorie restriction.
However, it is essential to ensure that the individuals themselves are capable to perform any physical activity or exercise safely.
- Moderate-intensity physical activity of at least 150 mins/week has demonstrated weight maintenance.
- A longer duration of > 300 mins/week was associated with weight maintenance after weight loss.
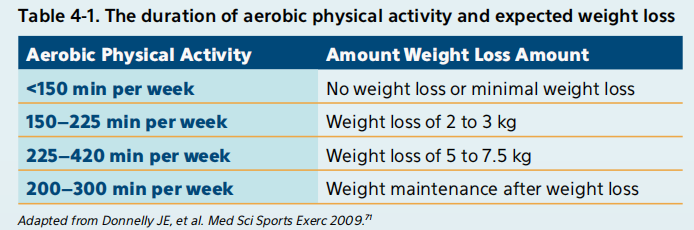
The effects on weight loss is proportional to the intensity of the activity. Higher intensity = better effects on weight loss.
There is evidence showing that higher intensity activity has better effects on weight loss compared to lower intensity activity.
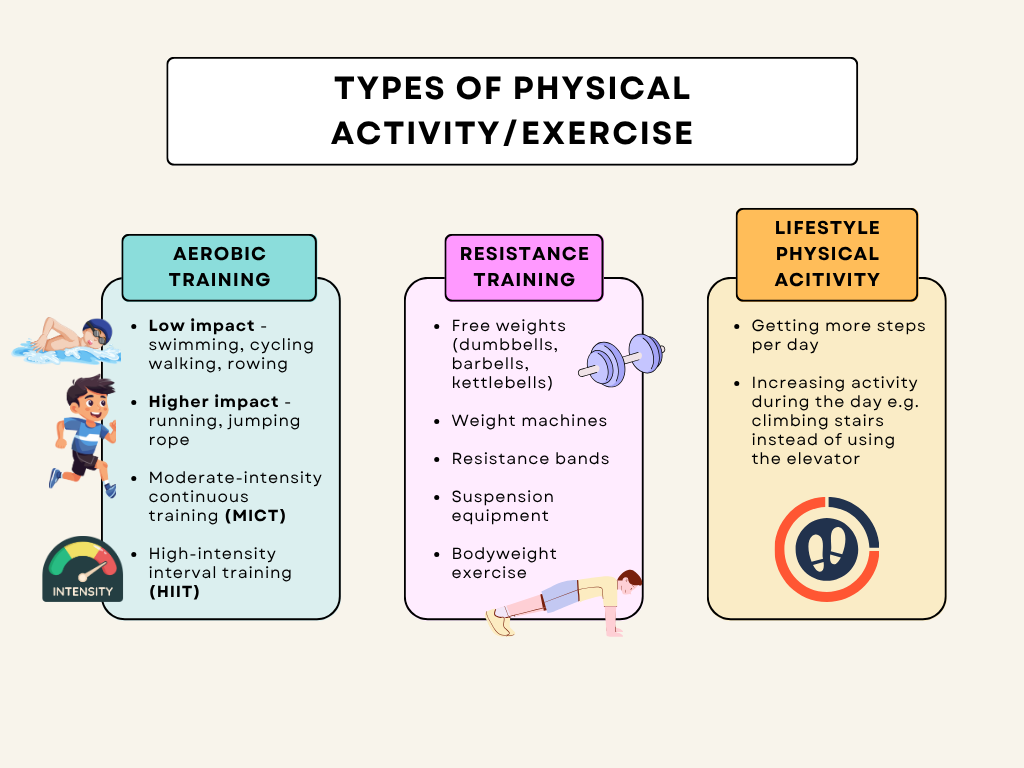
Prescription of physical activity/exercise
For those who have never exercised or physically inactive before, start small and go slow. Consider using the FITT formula (Frequency, Intensity, Time [duration], Type of exercise)
Start with small amounts of physical activity & increase the frequency, intensity & duration over time.
Each level of intensity and duration should be maintained for at least 1 – 2 weeks before increasing it further.
General starting regimen:
- Increasing the no. of walking steps & daily chores
- Gradual progression of aerobic exercise training
- Introduction of strength or resistance exercise
- Encourage flexibility exercises to attain the full range of motion
Caution to avoid problems:
- Progressing too rapidly will result in muscle soreness, fatigue, increased cardiac risk, & decreased motivation.
- To include warm up & cool down for each exercise period.
- Ensure adequate hydration before, during and after exercise.
- Stop when there are abnormal signs during exercise, e.g. chest pain, excessive breathlessness.
For elderly 🧓:
- Start small and go slow by gradually increasing the frequency, intensity & duration over time.
- Introduce strength training at moderate or greater intensity that involve all major muscle groups on 2 or more days a week. (Avoid training the same muscle group for consecutive days)
- Limit sedentary time.
- Emphasize functional balance & strength training at moderate or greater intensity, on 3 or more days a week, to enhance functional capacity & to prevent falls.
Physical activity should be encouraged in all individuals with obesity. Advise for:
- A minimum of 150 mins/week (30 mins/day) progressing to 300 mins/week (60 mins/day) of moderate intensity.
- Or at least 75 – 150 mins/week of vigorous intensity is required for weight loss.
- Both resistance & aerobic exercise should be included.
- Exercise prescription according to FITT formula.
Pharmacotherapy
Should only be used as an adjunct to lifestyle modification and is considered when weight loss goals or weight maintenance cannot be achieved with lifestyle intervention alone.
Pharmacotherapy may:
- Aid compliance with dietary restriction.
- Augment diet-related weight loss
- Achieve weight maintenance after satisfactory weight loss
Indications for pharmacotherapy
- BMI 27.0 – 29.9 kg/m² with associated risk factors (T2DM, Hypertension, Dyslipidemia, Obstructive sleep apnea)
- BMI ≥ 30 kg/m² with or without risk factors
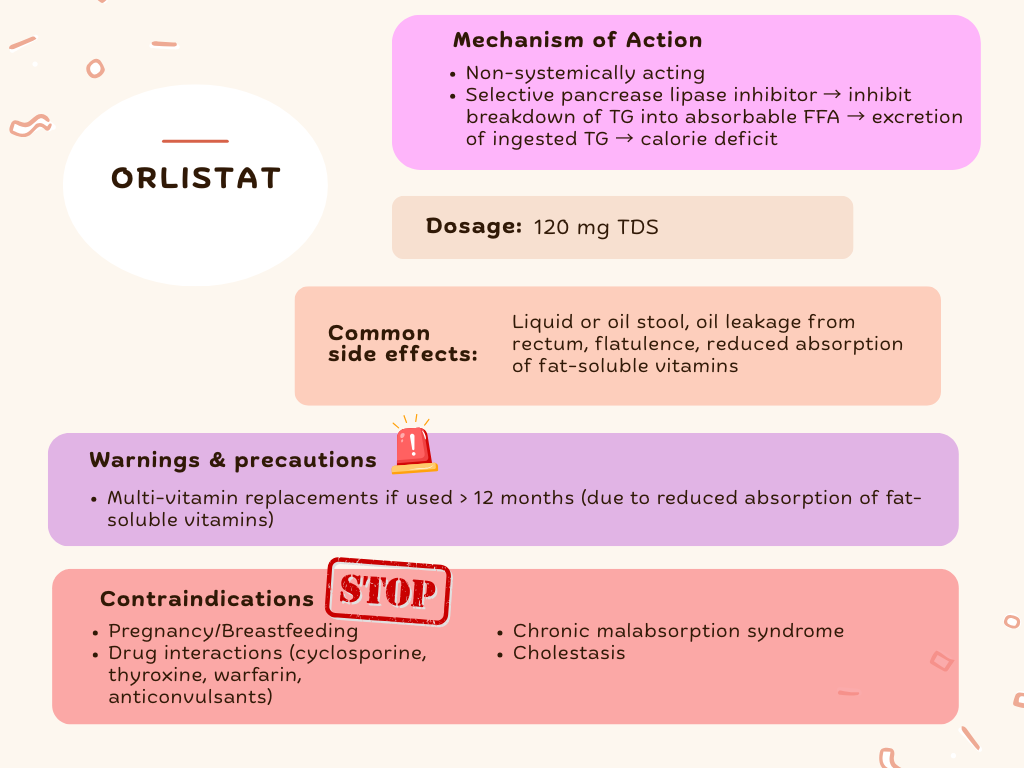
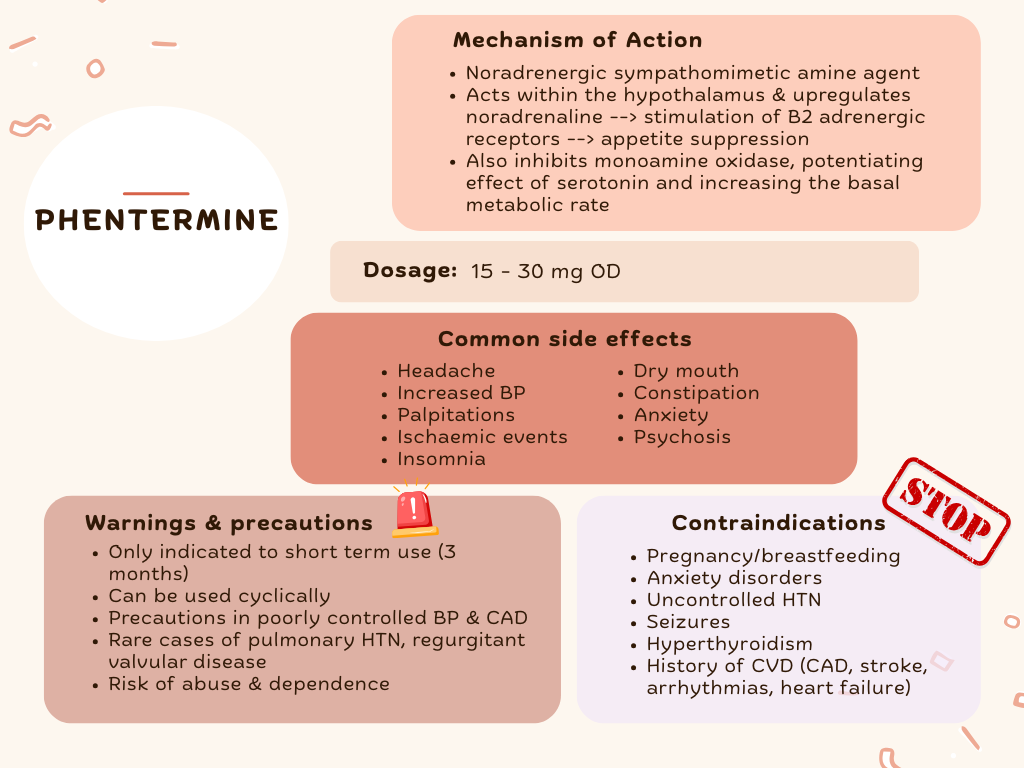
Pharmacotherapy should be considered long-term as obesity is a chronic disease.
- Short courses for ≤ 6 months do not result in sustained weight loss after medication discontinuation.
- However, sympathomimetic amines like phentermine alone should not be used long term especially in individuals with uncontrolled HTN or h/o heart disease as long-term prospective studies on CV outcomes have not been done.
If there is ≤ 5 % weight loss (not responding) after 3 months of an anti-obesity initiation or if there are significant tolerability issues, the drug should be discontinued and alternative medications/approach should be considered.
Once started on pharmacotherapy, TCA to review efficacy & safety:
- Monthly for first 3 months
- At least every 3 months thereafter
Anti-obesity drugs
5 USFDA approved medications:
- Orlistat – oral
- Phentermine (for not more than 3 months) – oral
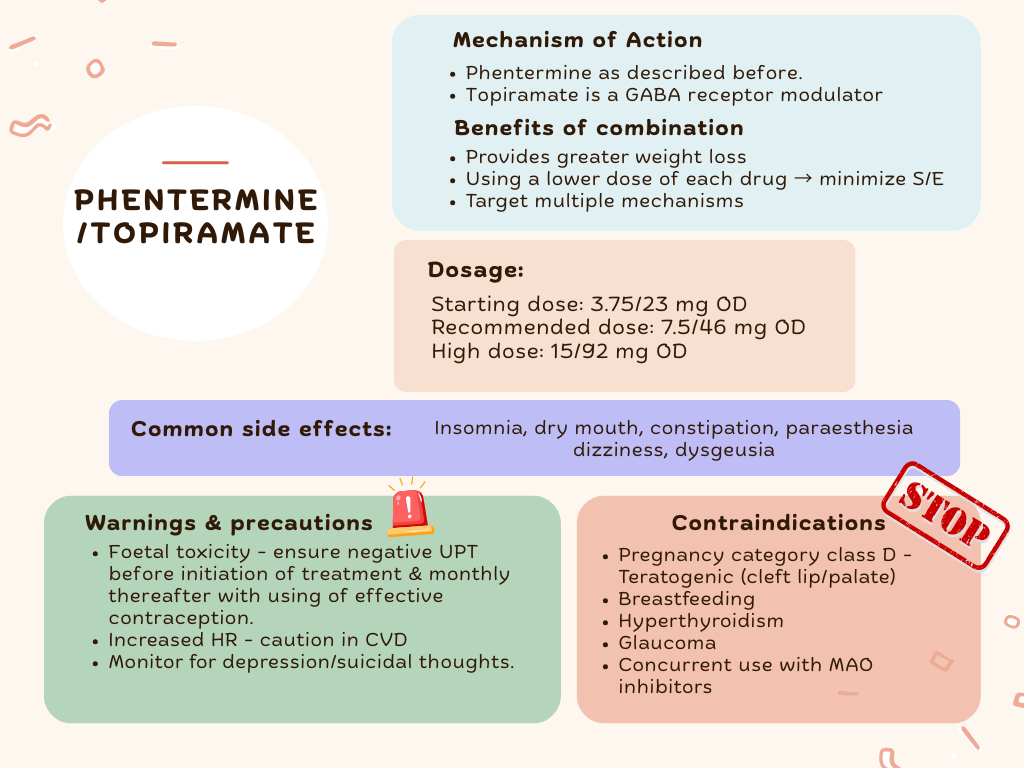
- Phentermine/topiramate combination – oral
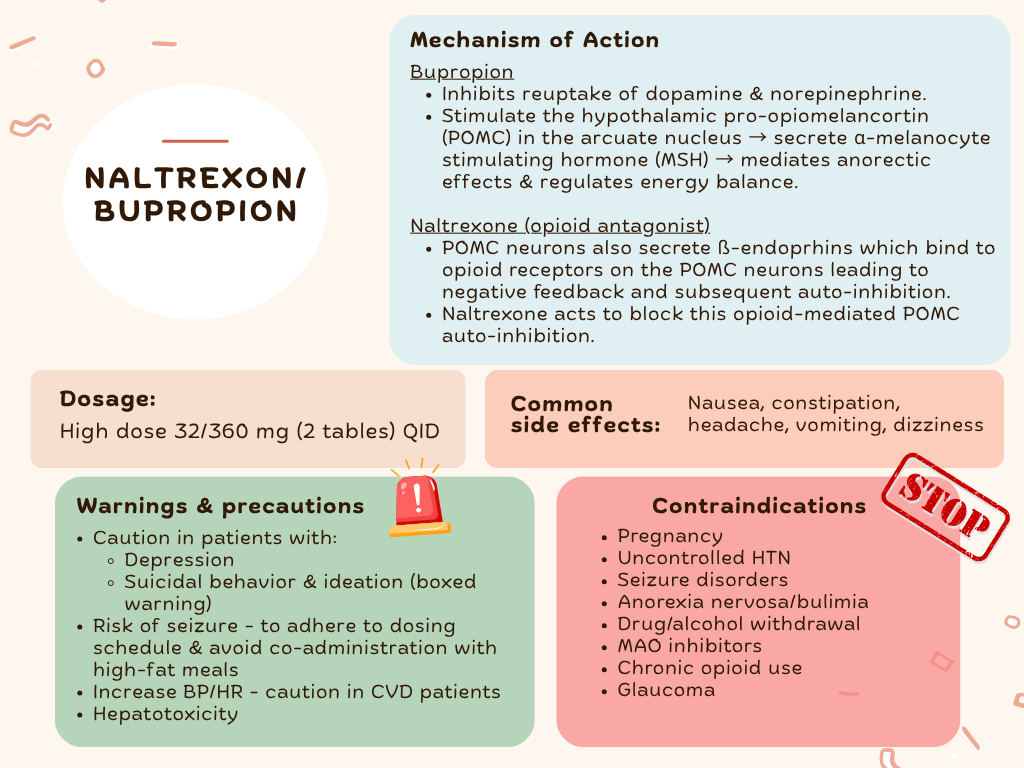
- Naltrexone/bupropion combination – oral
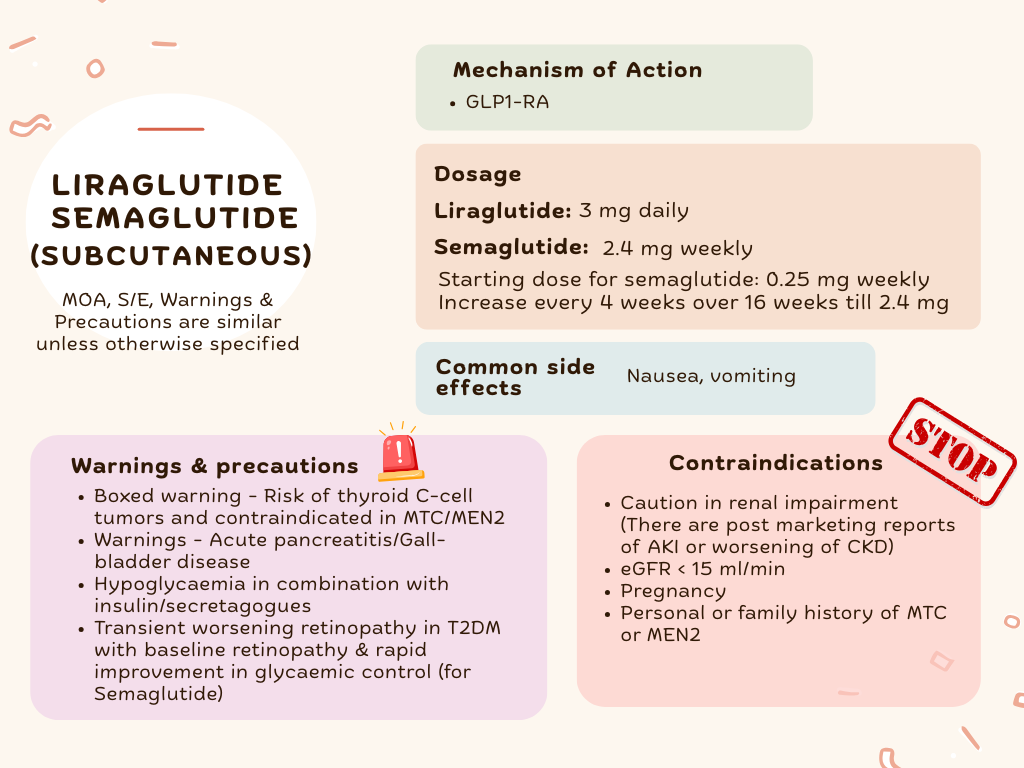
- High dose liraglutide (3 mg daily) – subcutaneous
- High dose semaglutide (2.4 mg weekly) – subcutaneous
In Malaysia, orlistat, phentermine, high dose liraglutide & semaglutide are available.
These medications can be categorized into:
- Acting on GI (to reduce fat absorption) – Orlistat
- Acting on CNS – Phentermine, Phentermine/Topiramate, Naltrexone/Bupropion, SC Liraglutide, SC Semaglutide
Surgical management
Bariatric surgery may be considered in individuals with morbid obesity who fail medical therapy.
Recommended for patients between the ages of 18 – 65 years.
The ultimate benefit of surgery is weight loss & control, & the remission of obesity’s metabolic component.
Surgical procedures include:
- Roux-En-Y gastric bypass (recommended)
- Sleeve gastrectomy
- Abdominal gastric banding
Indications for bariatric surgery
- Morbid obesity without any comorbidities – BMI >= 37.5 kg/m2 who fulfil the selection criteria*
Selection criteria includes:
- Previous non-surgical attempts at weight reduction for at least 6 months
- Demonstrated patient commitment:
– Follow up visits with healthcare team, voluntary participation in support groups & other recommendations made by their healthcare team.
– Compliance with instructions on medical management, procedures or test, including the use of dietary supplements & exercise routines.
– Smoking cessation for a minimum of 4 weeks before surgery.
- Morbid obesity with metabolic syndrome – BMI >= 32.5 kg/m2 with metabolic syndrome or CV risk that failed medical therapy & lifestyle modifications.
- Low BMI (< 32.5 kg/m2) with or without comorbidities – Surgery should not be routinely done. Should only be strictly performed under clinical study protocol with patient’s informed consent & approval from ethics committee.
References
Ministry of Health Malaysia, Malaysian Endocrine and Metabolic Society, Family Medicine Specialists Association of Malaysia, Malaysian Dietitians’ Association, & Malaysian Association for the Study of Obesity. (2023). Clinical practice guidelines: Management of obesity (2nd ed.). Malaysia Health Technology Assessment Section, Medical Development Division, Ministry of Health Malaysia.
