Nausea and vomiting of pregnancy

Nausea & Vomiting of Pregnancy
Definition
Nausea and Vomiting of Pregnancy (NVP)
- Symptoms of nausea &/or vomiting when onset is prior to 16 weeks of gestation and there are no other causes – Diagnosis of exclusion.
- Typically starts between the 4th and 7th week, & usually resolved by 20 weeks.
- If the initial onset is after 16 weeks POG, other causes should be investigated.
Hyperemesis Gravidarum (HG)
- Severe form of NVP.
- Generally HG is diagnosed when it is associated with triads of – Weight loss > 5% of pre-pregnancy weight, dehydration, & electrolyte imbalance.
- The latest RCOG guidelines define HG as severe, persistent nausea and vomiting (before 16 weeks POG) that impairs the ability to eat, drink, and perform daily activities. Signs of dehydration are considered contributory to diagnosis. This shift from objective measures, such as weight loss and electrolyte imbalances, to subjective, patient-centered criteria aim to improve the recognition and diagnosis of HG.
Both NVP & HG are thought to be associated with rising level of bhCG hormone.
Previous triads of Hyperemesis Gravidarum (replaced by newer definition as mentioned above)

PostBlock
Assessment
History
- Previous history of NVP/HG
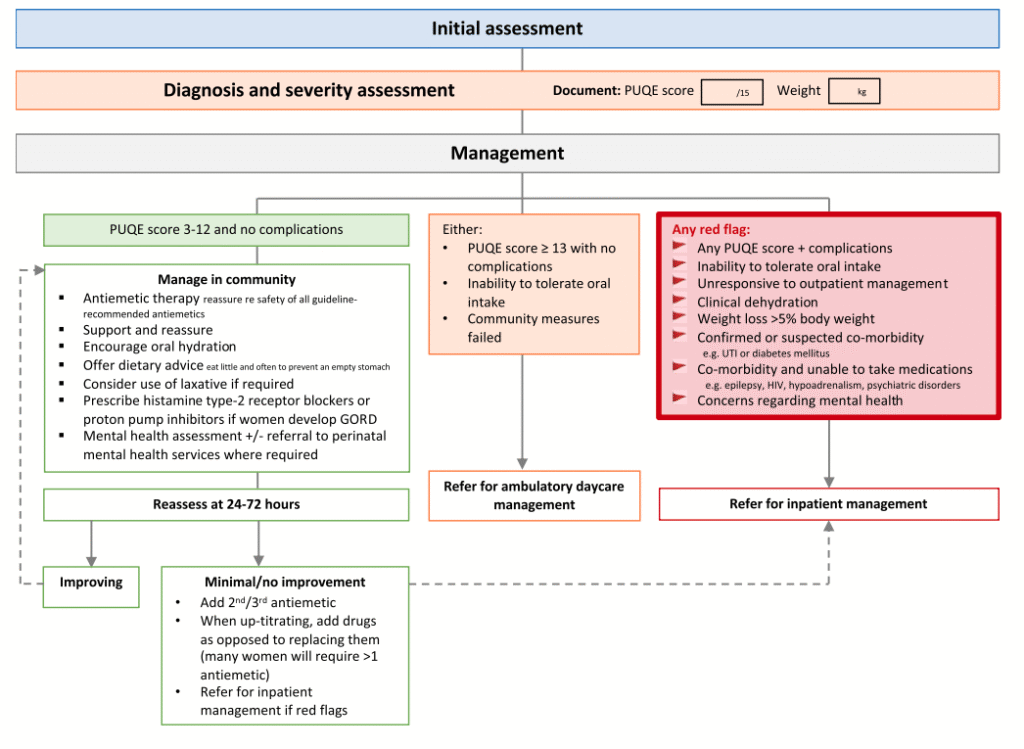
- Quantify severity of symptoms using PUQE score. (Alternatively, RCOG guideline recommends using HELP score to track progress with treatment in women with severe NVP & HG)
- History to exclude other causes:
- Abominal pain
- Urinary symptoms
- Infection
- Hyperthyroid symptoms
- Drug history (prescription &/or recreational)
- Chronic H. pylori infection
- Assessment of mood, mental health & quality of health.
- Ability to perform daily activities
- Co-morbidities
- Ptyalism (excessive production of saliva during pregnancy)
Pregnancy Quantification of Emesis (PUQE) score

Physical examination
- Weight
- Vitals signs – Temperature, BP, PR, RR, SpO2
- Abdominal examination
- Signs of dehydration
- Signs of muscle wasting/weakness
- General systemic examination – including fundoscopy & thyroid
- Assessment for neurological signs indicative of Wernicke’s encephalopathy – confusion, nystagmus or ataxia
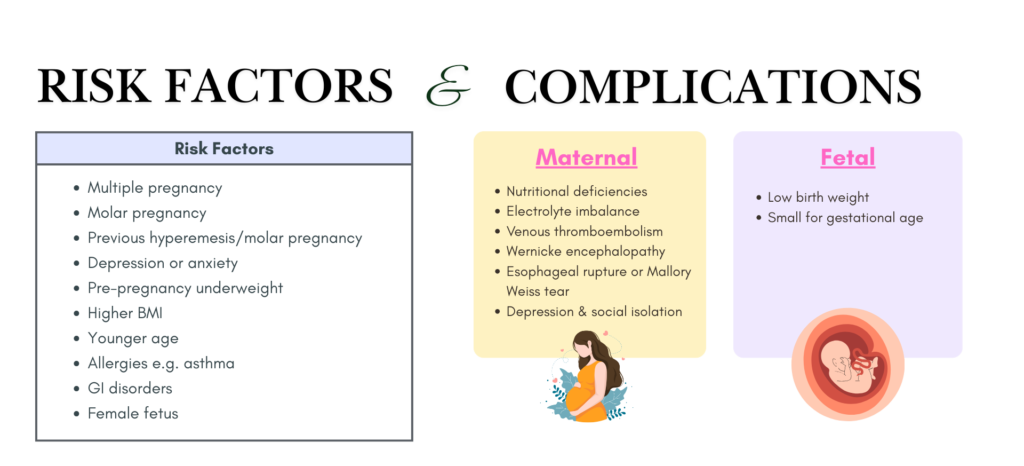
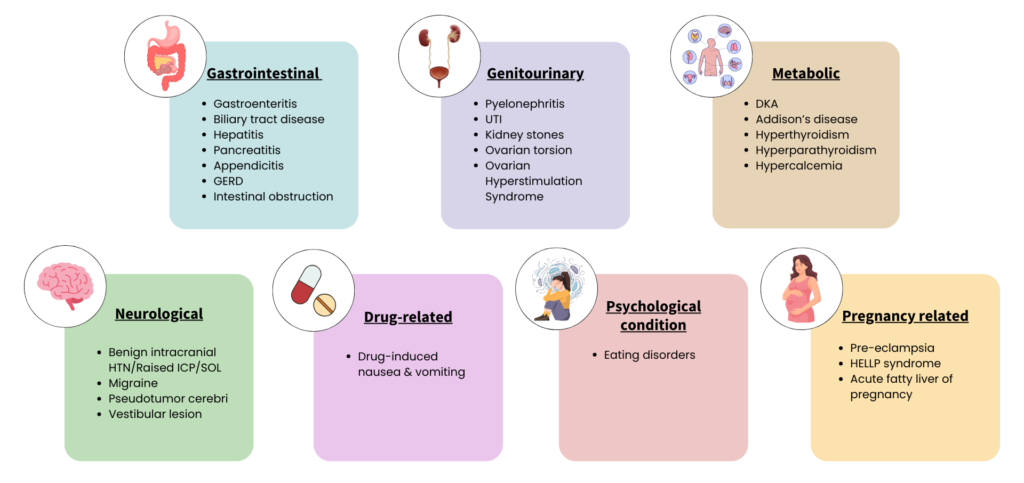
Differential diagnosis
Investigations
Biochemical
- Urinalysis, to look for:
- Leucocytes, Nitrites, Proteins – If positive, consider sending MSU for C&S (TRO UTI)
Ketonuria(The latest RCOG guideline no longer recommend ketonuria as part of assessment as it is not an indicator of dehydration and may be misleading; the severity should be assessed using HELP or PUQE score. However, in my opinion, it may still have a role if you are suspecting DKA)- Glycosuria – Consider diabetes & check blood glucose, especially if ketonuria is also present.
- Full blood count, to check for total white cell count (TWC) and hematocrit (assess for hydration)
- BUSE and creatinine, to assess:
- Hypokalemia
- Hyponatremia
- Raised serum urea/creatinine – suggestive of dehydration/AKI
- Magnesium/phosphate – if electrolytes abnormal
- Calcium, can be either:
– Hypocalcemia due to severe hypomagnesemia causing PTH resistance.
– Hypercalcemia as a potentially treatable cause of vomiting. If left untreated, can progress to severe early onset pre-eclampsia like illness.
- Liver Function Test (in refractory cases or history of previous admissions), TRO hepatitis/gallstones & to monitor malnutrition.
- Abnormal LFTs (often transaminases) may be seen in up to 40% of patients with HG.
- Monitor every 2 weeks if abnormal.
- Thyroid Function Test (only if there are SSx of thyroid dysfunction)
- May show biochemical hyperthyroidism, where:
– Free thyroxine is raised +/- suppressed TSH
– Clinically euthyroid (no symptoms)
– Thyroid antibodies negative
– Usually resolves with HG improvement
– No anti-thyroid medications needed
- May show biochemical hyperthyroidism, where:
- hCG level – as baseline if molar pregnancy is suspected
- Amylase – if pancreatitis is suspected
- Blood glucose – especially in diabetics, TRO DKA.

Imaging
USG:
- To confirm viable intrauterine pregnancy
- To assess for multiple pregnancy/molar pregnancy
Management
Mainly supportive.
Aim:
- To alleviate symptoms of nausea/vomiting
- Rehydration & correction of electrolyte imbalance
- To prevent complications
Admission criteria (to be referred for inpatient management)
- Abnormal urea & electrolytes
- Loss of 5% body weight
- Hematemesis
- Persistent vomiting after day case hydration
- Persistent ketonuria after day case hydration
- Second attendance for day case hydration
- Suspected other cause of vomiting
- Diabetes mellitus
- Severe hyperemesis
- Confirmed or suspected comorbidity (e.g. UTI, unable to tolerate oral medication)
** Day case hydration refer to those that are managed at daycare setting with parenteral fluids, vitamins & antiemetics and are suitable for those who have failed primary care measures and where the PUQE score is < 13.
Non-pharmacological management
- Change of environment/avoidance of triggers
- Dietary
- Eliminate greasy/fried food/coffee/spicy/very sweet food
- Small frequent meals throughout the day
- Supportive psychotherapy
- Acupressure applied by wrist band or finger at pericardium 6 (PC6) located 2.5 finger breadths up from the wrist crease on the inside of the forearm, between the tendons of palmaris longus & flexor carpi radialis.
- Do not routinely recommend ginger either as foodstuffs or OTC tablets as it may be ineffective and potentially harmful, causing adverse effects and worsening of symptoms.
- Consider avoiding iron-containing preparations if these exacerbate symptoms or consider alternative route of administration.
Fluid therapy 💧
Fluid requirement: Maintenance 25 – 30 mL/kg/day + replacement (guided by clinical/lab monitoring).
Normal saline (0.9% NaCl) + potassium chloride (tailored according to potassium deficit; avoid high doses due to risk of hyperkalemia & cardiac arrhythmias)
Adjust/stop fluids: Based on ketonuria/electrolytes; discontinue once normalized & oral intake resumes.
Correct other electrolytes as needed.
🚨Cautions:
- Avoid dextrose containing fluids unless the serum sodium levels are normal & thiamine has been administered. (Dextrose infusion can precipitate Wernicke’s encephalopathy if the woman is thiamine deficient).
- Avoid rapid saline administration due to risk of central pontine myelinolysis.
Pharmacological management 💊
Consists of:
- Antiemetics
- Vitamin supplementation
- Anti-reflux medications
- Thromboprophylaxis
- Enteral/parenteral nutrition
Antiemetics
- Antihistamines – Meclozine/pyridoxine, Promethazine
- Dopamine antagonists – Phenothiazines (Prochlorperazine, Chlorpromazine), Metoclopramide, Domperidone
- Serotonin inhibitors/5-HT3 antagonist (used only if no other alternatives & benefits outweigh risk) – Odansetrone
- Corticosteroids (reserved for refractory cases) – may cause oral cleft in fetus if given < 10 weeks of gestation
Combinations of different drugs can be used if the women do not respond to a single antiemetic.


Metoclopramide
- Used as 2nd line due to risk of extrapyramidal effect – when given by IV, should be given via slow bolus over at least 3 mins to minimize risk.
- Only for short term use, max 5 days.
- Max dose of 30 mg in 24 hours or 0.5/kg body weight in 24 hours, whichever the lowest.
Odansetron
- Studies on its safety is mixed.
- There may be small increased risk of cardiac defect (Data from Swedish Medical & Birth Register)
- Consider only when other antiemetics failed, & preferably used after first trimester.

- Reserved for refractory cases.
- There is concern where 1st trimester exposure can cause oral cleft in fetus if given < 10 weeks of gestation.
- Nevertheless, the latest RCOG guidelines mentioned that there are data showing that first-trimester corticosteroid use does not increase the risk of congenital malformations, including orofacial clefts, cardiac defects, or hypospadias. However, with only around 3,500 exposures studied, it remains less researched compared to other antiemetics.
- Women taking corticosteroids should be screened for diabetes & have their BP monitored.
Vitamin supplementation
- Thiamine (PO 25 – 50 mg TDS, if able to tolerate orally) – for all women with prolonged vomiting especially before dextrose or parenteral nutrition administration.
– If unable to tolerate orally, parenteral thiamine should be given, and high doses (e.g., 100 mg daily) continued for each day IV dextrose is administered to prevent Wernicke’s encephalopathy. - Folic acid (5 mg OD once tolerating orally as empirical supplement in pregnancy)
Anti-reflux medications (if having GERD/esophagitis/gastritis)
- Alginate (PO 10 – 20 mls TDS – max 80 mls/day)
- Ranitidine (IV 50 mg TDS; PO 150 mg BD)
- PPI
Thromboprohylaxis
- VTE risk scoring as per Malaysia VTE CPG guidelines.
- TED stocking
- Anticoagulants if VTE score dictates
Enteral/parenteral nutrition
- May be considered for those who are refractory to all pharmacological (including corticosteroids) & non-pharmacological treatment.
Treatment algorithm
References
- Ministry of Health, Malaysia. 2020. Consensus Statement on Management of Hyperemesis Gravidarum.
- Nelson-Piercy C, Dean C, Shehmar M, Gadsby R, O’Hara M, Hodson K, Nana M; Royal College of Obstetricians and Gynaecologists. The Management of Nausea and Vomiting in Pregnancy and Hyperemesis Gravidarum (Green-top Guideline No. 69). BJOG. 2024 Jun;131(7):e1-e30. doi: 10.1111/1471-0528.17739. Epub 2024 Feb 4. Erratum in: BJOG. 2025 Sep;132(10):1541. doi: 10.1111/1471-0528.18258. PMID: 38311315. From <https://pubmed.ncbi.nlm.nih.gov/38311315/>
- Correction to ‘The Management of Nausea and Vomiting in Pregnancy and Hyperemesis Gravidarum (Green-Top Guideline No. 69)’. BJOG. 2025 Sep;132(10):1541. doi: 10.1111/1471-0528.18258. Epub 2025 Jun 19. Erratum for: BJOG. 2024 Jun;131(7):e1-e30. doi: 10.1111/1471-0528.17739. PMID: 40536112. From <https://pubmed.ncbi.nlm.nih.gov/40536112/
