Definition
- Menopause: No period for 12 months (1 year) without any preceding pathological or physiological cause [The average age of menopause in Malaysia is 50.7 years]
- Perimenopause: The time immediately before menopause till 1 year after the last menstrual period.

During this phase, erratic peaks in serum estradiol & progesterone can bring about a wide variation in cycles and flow.
– Cycles may be initially shorter followed by longer intervals.
– The flow may vary from prolonged spotting to heavy periods with clots.
– As ovulation can be unpredictable, contraception is still required till one year after the LMP.
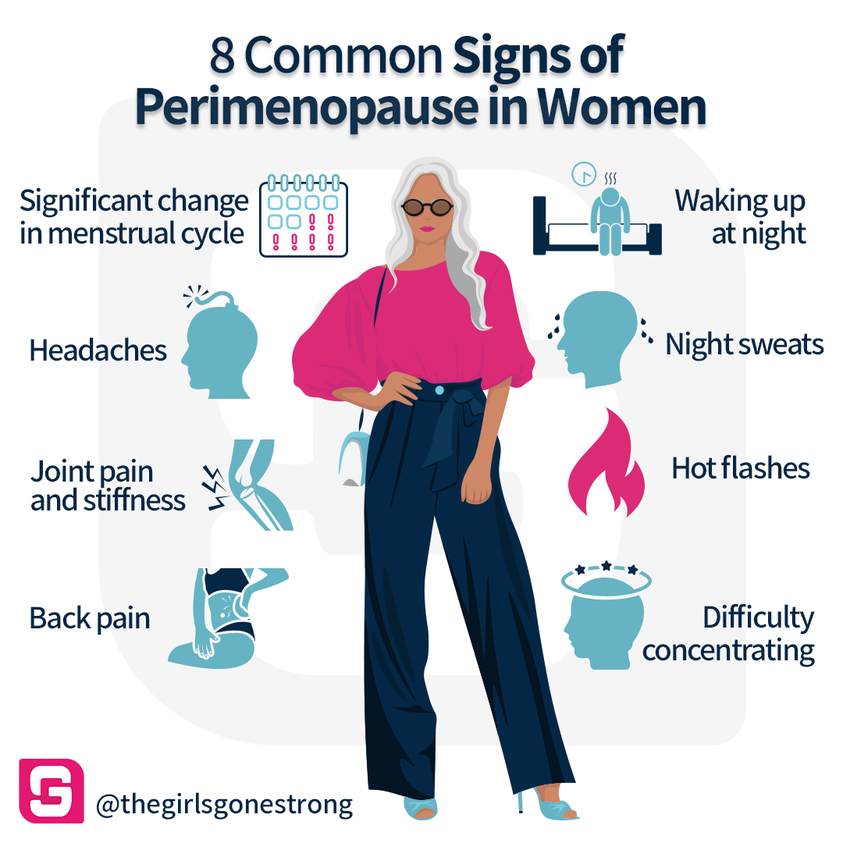
- Diagnosis of perimenopause is purely clinical.
- Blood investigations for anemia, thyroid dysfunction & coagulation disorders (if necessary) are advised.
- AUB during the perimenopause should always be investigated, based on the FIGO classification system of PALM-COEIN
- Sexually active women p/w AUB should have a VE, pap smear & TVS TRO pathology in the cervix, uterus & ovaries.
- Pregnancy should also be ruled out.
Clinical assessment and investigations
Detailed history
- Personal history, including menopausal Sx; Menopausal Questionnaire
- Obstetric, gynaecological history
- Menstrual & sexual history
- Previous medical (e.g. h/o blood clotting problems), surgical history
- Allergic history
- Family history – hormone related cancers, CVS disease, clotting problems, osteoporosis.
- Social history: smoking, vaping, alcohol
- Lifestyle: stress, diet, exercise
General examination
- BP
- BMI
- Breast examination
- Abdominal examination, TRO pelvic masses
- VE (if applicable): TRO infections, cervical lesions, pelvic masses & to assess pelvic floor
Recommended investigations
- FBC, RP, LFT
- FBS, FSL
- Pap smear (if applicable)
- Breast screening using USG &/or mammography
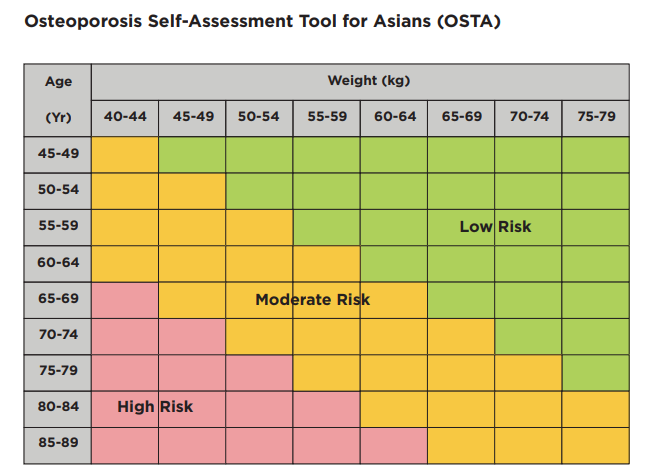
- Bone mineral density (if needed)
- OSTA can also be used to identify those at risk for osteoporosis.
- VE & pap smears are carried out only in women who are/have been sexually active.
- FSH should not be routinely considered when diagnosing menopause in women > 45 y/o
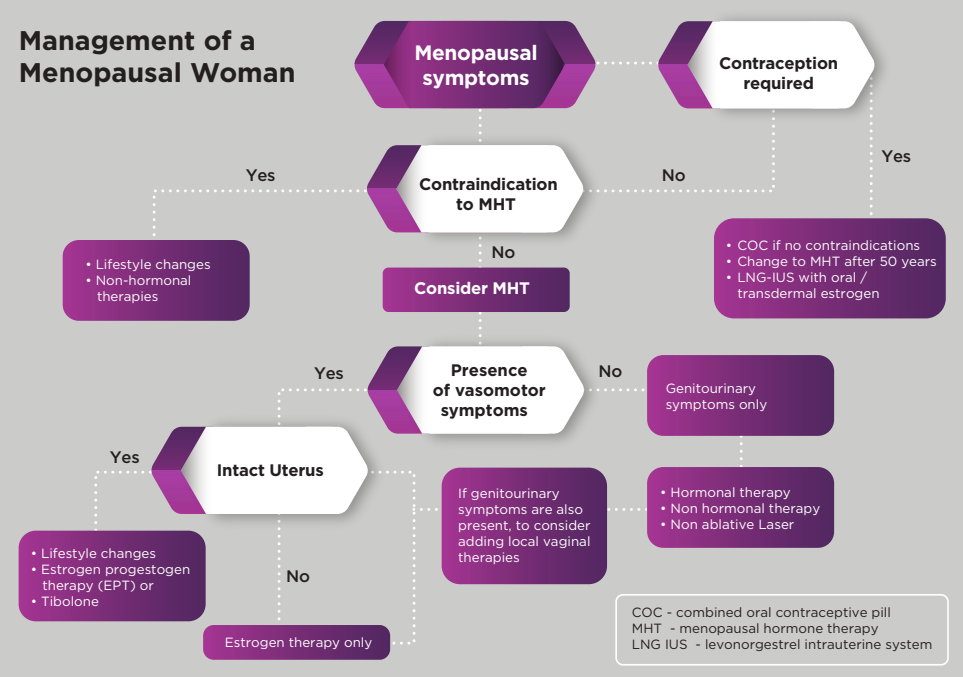
Management
Lifestyle changes
- Maintaining healthy weight
- Stop smoking or vaping
- Cutting down spicy food and excessive food
- Minimizing PUFA, trans fats, salt, & sugar.
- Minimizing alcohol
- BP control
- Regular exercise 5 days a week; 30 mins each time
- Sleeping soundly for 6 – 9 hours every night
- Stress reduction
- Support group programs (esp. spousal support)

Menopausal Hormonal Therapy (MHT)
Indications for MHT
i. Vasomotor symptoms
ii. Prevention of bone loss
iii. Hypoestrogenism due to e.g. hypogonadism, POI, or premature surgical menopause
iv. Genitourinary syndrome of menopause
Contraindications of MHT
- Breast/endometrial CA (any hormone related cancer)
- Blood clots in the lungs, eyes, or deep veins
- Heart attack, stroke or TIA
- Liver disease or liver problems
- Inadequately controlled arterial HTN
- Undiagnosed uterine or vaginal bleeding
- Porphyria
- Pregnancy
Relative contraindications: Endometriosis, Fibroids (Annual pelvic USG is advised)
Types of MHT
a) Hysterectomised women need only estrogen therapy
b) Non-hysterectomised women need both estrogen and progestogen. Progestogen is added for endometrial protection. Can be given as:
i. Cyclical therapy – for perimenopause, will have regular period
ii. Continuous combined therapy – for menopausal women, no bleed therapy
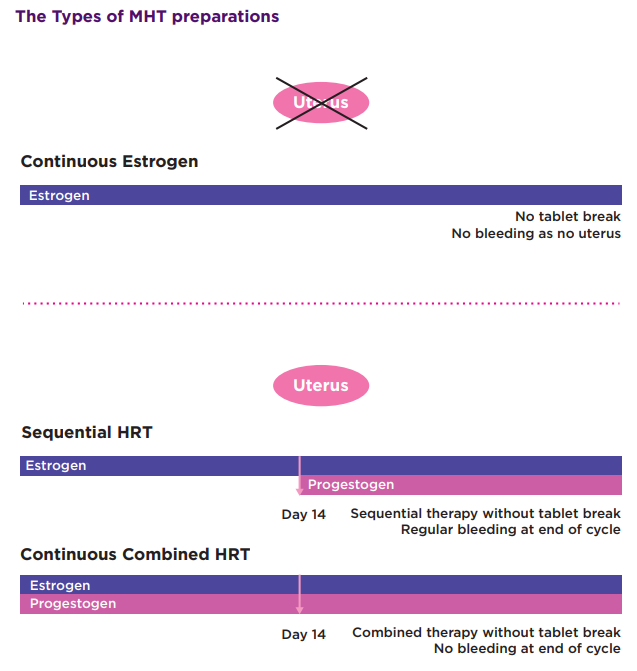
For continuous combined therapy:
– Initial spotting or staining (break through bleeding) is common up to 6 months, after which there should not be any bleeding.
– Missing a pill/non-compliant may also cause irregular bleeding.
– Unschedule bleeding beyond 6 months should always be investigated.
Some key concept 🗝️
Benefits of MHT outweigh risks when given to healthy symptomatic women < 60 years or within 10 years of menopause & thus should be considered in these group of patients. (Women who initiate MHT 10 years after menopause have a higher absolute risk of CHD, stroke, venous thromboembolism & dementia.)
Women with perimenopausal Sx are advised either:
a) low dose COCP – acts as contraceptive, better cycle control & treats perimenopausal Sx.
b) MHT – better cycle control & treats perimenopausal Sx. Inadequate as contraceptive.
(Women above 50 years who are yet to reach menopause should be counselled about the 1% risk of pregnancy & additional contraceptive measures are to be taken)
c) LNG-IUS +- estrogen (orally or transdermal)
Low dose vaginal ET may be considered for relief of Sx of genitourinary syndrome of menopause. Additional progestogen therapy is not needed,
– Not indicated for treatment of hot flushes, prevention of osteoporosis, heart disease, or other major health conditions.
Any unscheduled vaginal bleeding should always be investigated.
Possible side effects of MHT
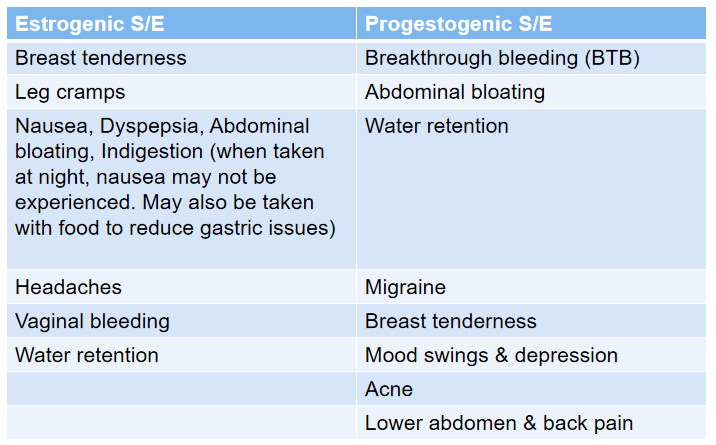
S/E are usually transient & resolves with time.
Women are encouraged to persist for at least 3 months to allow the initial S/E to settle.
Major S/E of concern
– CVS: Stroke, CAD, Venous thromboembolism, PE
– Malignancies: Breast cancer, Endometrial cancer (estrogen alone in patient with intact uterus)
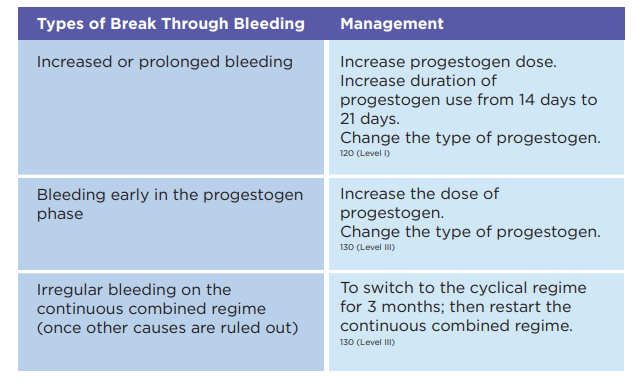
Management of Breakthrough Bleeding (BTB)
Follow up after starting MHT
Initial review after 3 months to check on S/E & effectiveness of treatment.
Upon a satisfactory review, annual consultation is advised.
During the f/up, things to review:
1. BP, PR & BMI
2. Any S/E, e.g. breast tenderness, nausea, headaches & bleeding
3. Presence of any new gynecological or non-gynecological problems
4. Regular breast evaluation. Mammogram &/or breast USG are carried out 1 – 2 yearly depending on screening test & risk of breast CA.
5. Cervical screening (if applicable) at 1 – 3 yearly intervals
6. Review & discussion on benefit-risk ratio
7. Relevant blood IX, i.e. lipids & glucose.
Reason for earlier follow up
- Unscheduled vaginal bleeding
- Persistent S/E to MHT
- Persistent menopausal Sx
- Recent blood-clotting disorder
- Recent Sx of CVS disease
- Recent hormone-dependent breast CA or another hormone-dependent CA
- Any recent new gynecological or non-gynecological problem that is of concern to the individual
Factors to be considered if pt remains symptomatic whilst on MHT:
1. GI disturbances leading to poor absorption.
2. Drug interactions leading to reduced bioavailability e.g. carbamazepine, phenytoin
3. Other medical problems mimicing menopause e.g. hypothyroidism, DM
4. Inadequate estrogen dose
5. Pt’s expectations that all menopausal Sx will be resolved.
Duration of use for MHT
- Presently no mandatory limitation to duration of MHT use.
- Factors to be taken into consideration of continuous use of MHT include:
– Pt’s personal preferences.
– Yearly review with benefit-risk assessment.
– Whether the primary use of MHT is for prevention or for QOL purposes. - When long term MHT(> 10 yrs) is considered, a low dose hormonal regime is advised.
- Continued use of MHT (> 10 years) is recommended in those with persistent VMS, to improve symptoms related to GSM, to increase bone density & to reduce fracture at all sites.
Reasons for stopping MHT 🛑
- New contraindications
- Risks > benefits
- Side effects
- Persistence of symptoms
- Pt’s preference
Possible of symptoms recurrence upon stopping MHT.
MHT should be ceased gradually over a period of 3 – 6 months rather than abruptly, to avoid rebound of Sx.
Alternative pharmacological therapy
Alternative treatment may be required for those who are contraindicated of MHT but having specific Sx of VMS & GSM
Alternative pharmacological therapy
– Clonidine (anti-hypertensive)
– SNRIs (venlafaxine 100 mg/day)
– SSRIs – paroxetine, fluoxetine, citalopram & escitalopram
– Antiepileptics – gabapentin 300 mg TDS, pregabalin 75 mg BD.
Supplements
- 1200 mgs of calcium (dietary + supplements) is recommended daily for its +ve effect on BMD & fracture risk reduction.
- Adequate Vit. D supplementation (600 IU in women below 70 years & 800 IU after 70 years) reduces the risk of fracture & falls.
(Aim to achieve Vit. D levels of > 50 ng/mL)
Algorithm summary