Insomnia

Insomnia
Definition
Persistent difficulty with sleep initiation, duration, consolidation, or quality that occurs despite adequate opportunity and circumstances for sleep, resulting in some form of daytime impairment.
Neurotransmitters involved in sleep
Understanding the different neurotransmitter involved can help us to understand the different pharmacological treatment.
Sleep-inducing (inhibiting wakefulness): Adenosine, Nitric oxide, GABA
Sleep-preventing (triggering wakefulness): Glutamate, Norepinephrine, Dopamine, Serotonin, Acetylcholine, Histamine, Orexin A and B
Acute vs Chronic insomnia
Acute insomnia
- Also known as adjustment insomnia
- Duration: < 3 months
- Usually has a precipitating/identifiable stressors
- Expected to resolve when the stressor resolves
- However, there is risk of progression to chronic insomnia if the individual developed changed thinking & maladaptive behaviors around sleep.
Chronic insomnia
- Occurring on ≥ 3 nights per week over a period of 3 months
- Resulting in significant distress or impact on daytime functioning
- High rate of recurrence
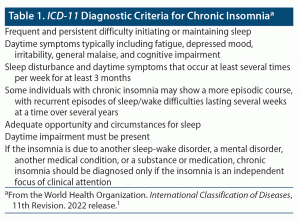
Diagnostic criteria for chronic insomnia
The criteria are similar for both the American Academy of Sleep Medicine (AASM, 2014) and ICD-11, with the AASM going into more details on the sleep disturbance & associated consequences.
American Academy of Sleep Medicine Criteria

ICD-11 Diagnostic criteria
Comorbidities
Common comorbid disorders include depression, anxiety, chronic medical conditions. It is important to keep in mind that insomnia disorder often coexist with & is not merely secondary to the mentioned comorbid disorders.
Insomnia can also present together with comorbid sleep disorders like OSA, restless leg syndrome, and circadian rhythm disorder.
- Excessive daytime sleepiness is uncommon for insomnia and warrants further investigation & exclusion of sleep disordered breathing.
The importance of assessing for comorbidities lies in the bidirectional interactions between insomnia disorder and comorbidities where each can exacerbate the other (e.g. insomnia can worsen the comorbidity and vice versa).
Common comorbidities or contributory factors to chronic insomnia
|
Mental |
Medical |
Neurological |
Substance use/dependence |
|
|
|
|
Approach to assess insomnia
2-question screening tool
- Do you have trouble getting to sleep or staying asleep?
- Do you feel well rested during the day?
(OR Are you satisfied with the quantity & quality of your sleep?)
Further assessment
Ask about:
- The nature of sleep disturbance e.g. delayed sleep onset, trouble staying asleep, early morning awakening
- Sleep routines
- Potential maladaptive habits
- Impaired daytime functioning – fatigue, reduced alertness
- Any comorbidities – medical and psychological/mental disorders
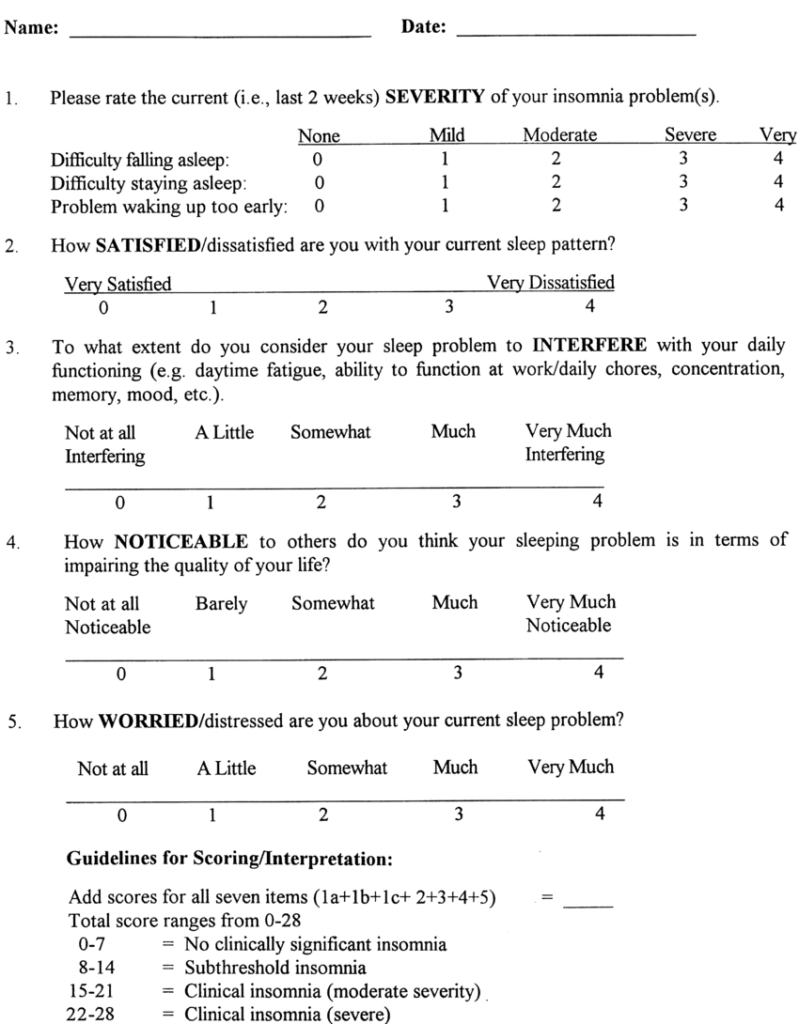
Severity assessment using the Insomnia Severity Index (ISI)
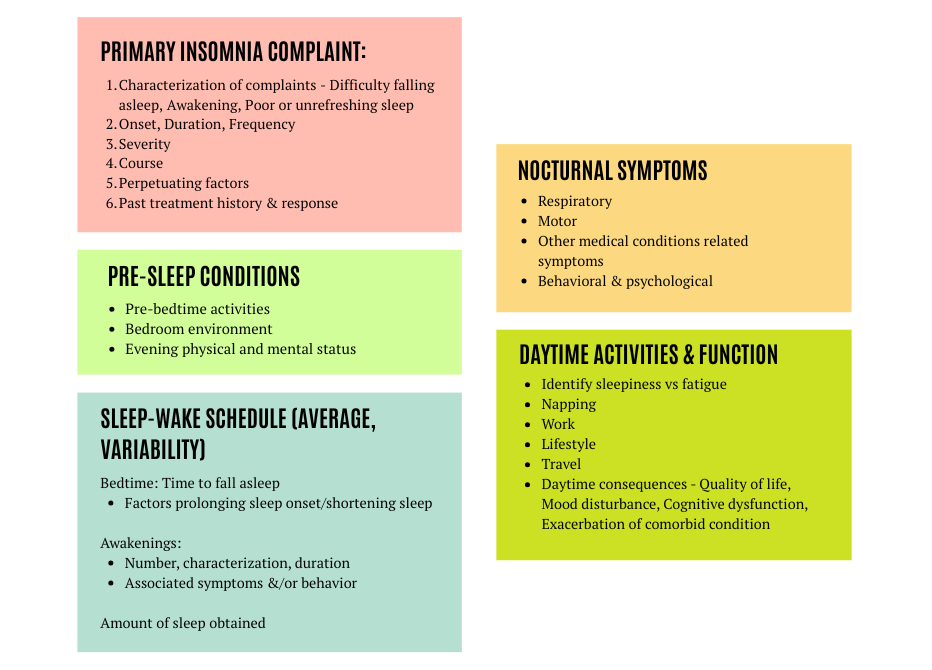
Detailed Sleep History
As outlined in the AASM guideline
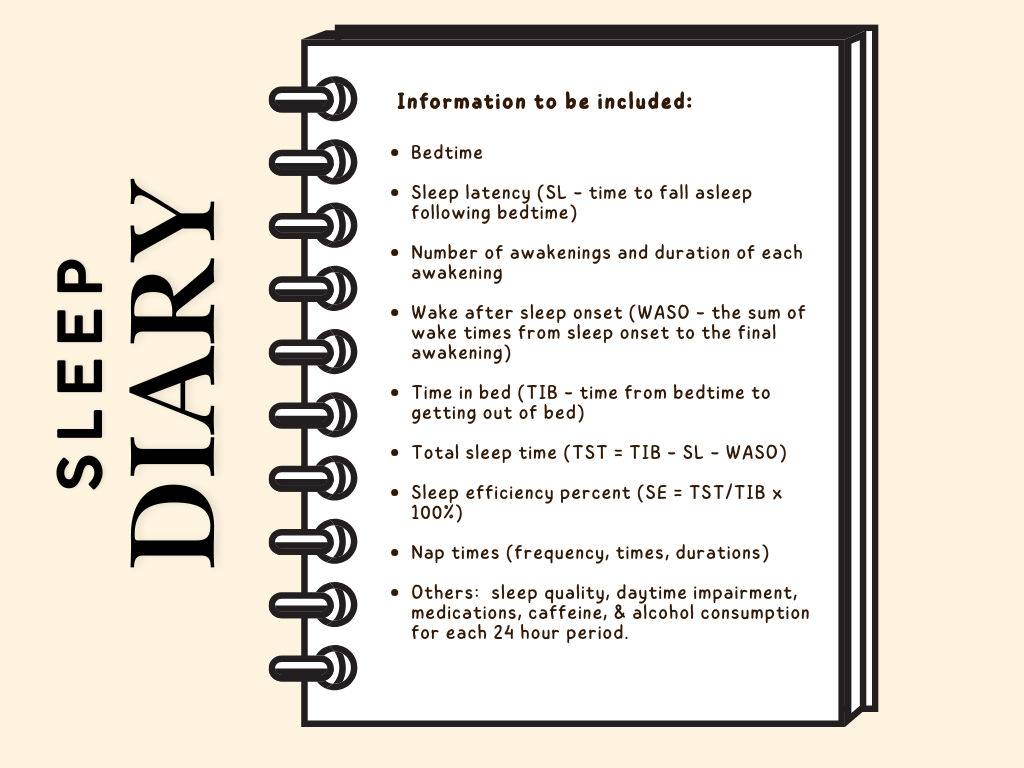
Sleep Diary
Useful to assess patient’s symptoms while engaging patient in their own treatment.
Physical & mental status examination
May provide information regarding comorbid disorders & differential diagnosis.
This include:
- Assessment on risk factors for sleep apnea – obesity, increased neck circumference
- Evaluation for other physical signs of comorbid medical conditions (e.g. pulmonary, cardiac, GI, endocrine, etc).
Mental status examination should focus on mood, anxiety, memory, concentration, & degree of alertness or sleepiness.
Investigations
Lab test, polysomnography & actigraphy are not usually necessary nor recommended for initial assessment.
Additional clinical screening tools, laboratory & sleeping studies may be required TRO other sleep disrupting conditions like mood disorders, restless leg syndrome, obstructive sleep apnea, etc.
Management
Key principles:
- Reducing sleep-related anxiety & maladaptive behaviors around sleep.
- Addressing comorbidities & precipitating factors
Cognitive Behavioral Therapy for Insomnia (CBT-I)
Consists of combination of cognitive strategies & behavioral methods.
First-line therapy (recommended by guidelines)
A typical course of CBT-I lasts for 6 – 8 weeks.
Can be done via individual/group sessions, face-to-face or online & via patient self-education.
Multicomponent therapy (combination of different interventions) is more effective & recommended compared to therapy.
These interventions consist of :
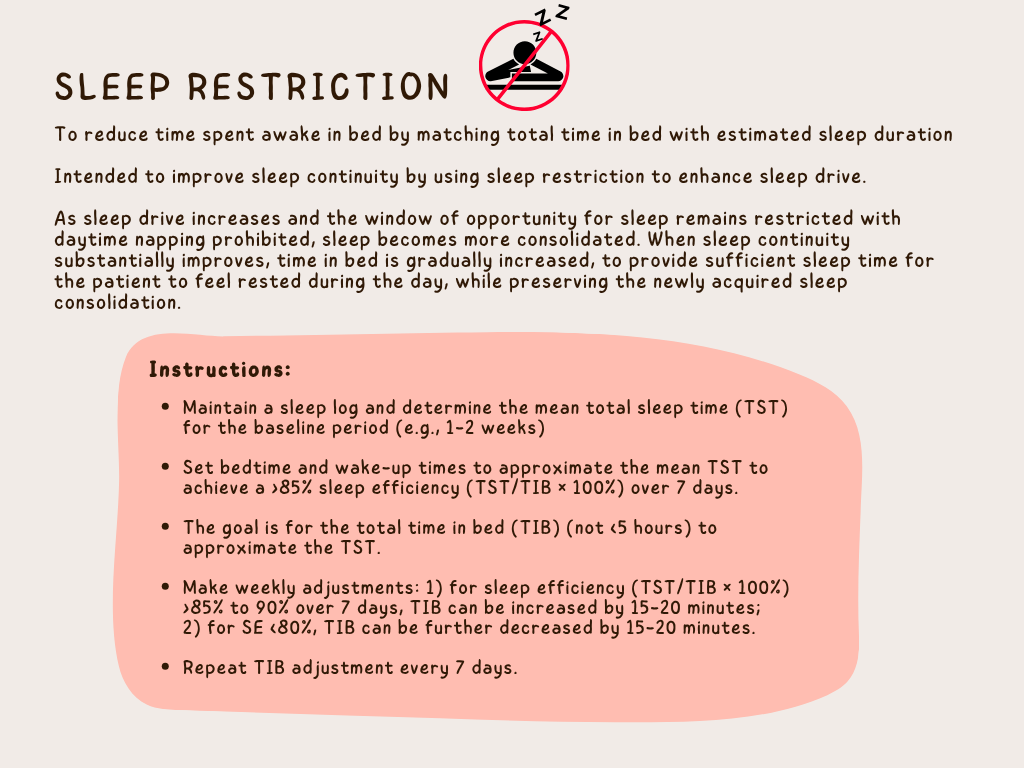
- Sleep hygiene
- Sleep restriction
- Stimulus control
- Relaxation strategies
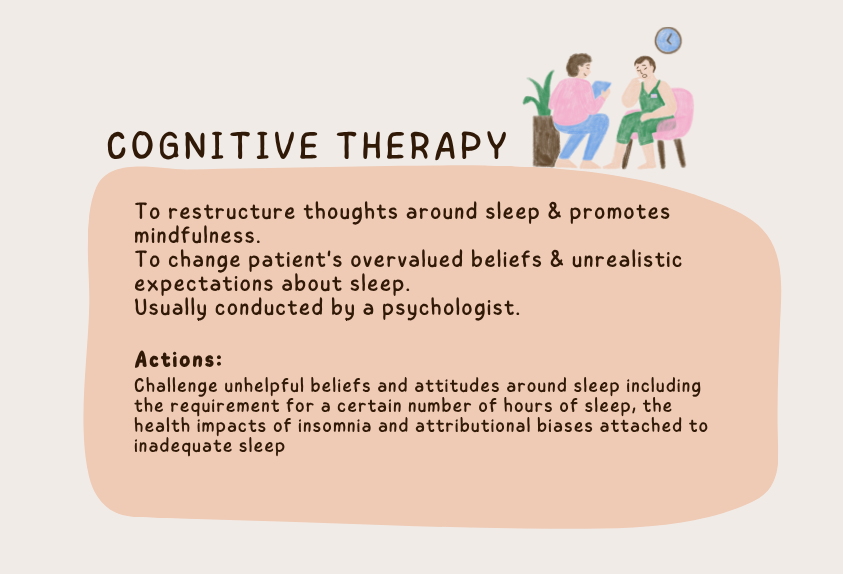
- Cognitive therapy
Pharmacological management for chronic insomnia
1. Dual orexin receptor antagonists (DORAs)
Orexin-A & orexin-B are neuropeptides involved in arousal behavior & inducing wakefulness.
MOA: Acts by blocking 2 orexin receptors OX1R and OX2R. Reduces arousal but preserve patient’s ability to be awaken in response to auditory stimuli.
Can improve sleep latency, sleep maintenance & total sleep time.
Effective in sleep maintenance due to sleep arousal.
DORAs can be safe & effective longer-term option.
Example of DORAs: Suvorexant, Lemborexant, Daridorexant
2. Benzodiazepines (BZDs) and Benzodiazepine receptor agonists
Effective short term treatment for sleep onset & sleep maintenance insomnia.
Empirical data support both nightly & intermittent (2 – 5 times per week) administrations. PRN dosing is not generally recommended due to potential for carry-over sedation the next morning & potential for inducing conditioned arousals in anticipation of a medication dose.
There is risk of dependency, tolerance and abuse but this can be reduced by limiting dose increment & regular monitoring.
Generally recommended for short-term use (up to 4 weeks). Initial treatment of 2 – 4 weeks may be appropriate.
A safe withdrawal strategy (after more than a few days of use) is required as sudden withdrawal can lead to rebound insomnia (typically lasting 1 – 3 days) or physical & psychological withdrawal symptoms. This can be achieved by gradual tapering of the dose & frequency of administration
Examples of :
- BZDs – Alprazolam, Clonazepam, Estazolam, Lorazepam, etc.
- BZD receptor agonists – Eszopiclone, Zalepion, Zolpidem
3. Melatonin (2mg extended-release formulation)
Indicated for treatment of insomnia in adults > 55 years of age. (As listed in MIMS)
May also be useful for circadian rhythm disturbance (sleep onset insomnia) or early wakening.
Meta-analyses have demonstrated small effects on sleep latency, with little effect on WASO or TST (Kindly refer to the sleep diary above for these terminologies)
4. Melatonin agonist – Ramelteon
Primarily used for sleep-onset insomnia
Short acting
Off-label pharmacological treatment (most have limited evidence on efficacy & safety)
These include :
Sedating low-dose antidepressant
Examples : Trazodone, Mirtazapine, Doxepin, Amitriptyline, Trimipramine
Can be considered in patients with comorbid major depression & insomnia.
However, low-dose sedating antidepressants alone do not constitute adequate treatment of major depression with comorbid insomnia but it can be used as an adjunct (sleep-aid) to other full dose antidepressants according to AASM guideline.
If sedating antidepressant is used as monotherapy for patient with comorbid depression & insomnia, the dose should be that recommended for treatment of depression.
Sedating antipsychotic
Examples : Quetiapine or Olanzapine
May be useful in individuals with comorbid bipolar disorders or severe anxiety disorders.
Antihistamines
Limited evidence on safety & efficacy.
Potential for significant side effects due to concurrent anticholinergic properties.
It is important to keep in mind that there is limited evidence regarding their role in insomnia management, and their significant potential adverse effects have to be taken into consideration.
For Acute Insomnia
The main focus is to address the precipitating factors.
Pharmacological treatment is generally used for short duration (up to 4 weeks) if needed.
Matching treatment with patient’s complaint & presentation
Patient should be monitored frequently to assess treatment efficacy & identify any potential adverse effects.
For pregnant or breastfeeding women, CBT-I may be a better option than any insomnia medication.
Indications for referral
- Possible comorbid sleep disorder
- Not responding to brief behavioral disorder
- Persistent & distressing symptoms
- When insomnia is related to other comorbidities like depression or anxiety (consider referral to psychiatrist)
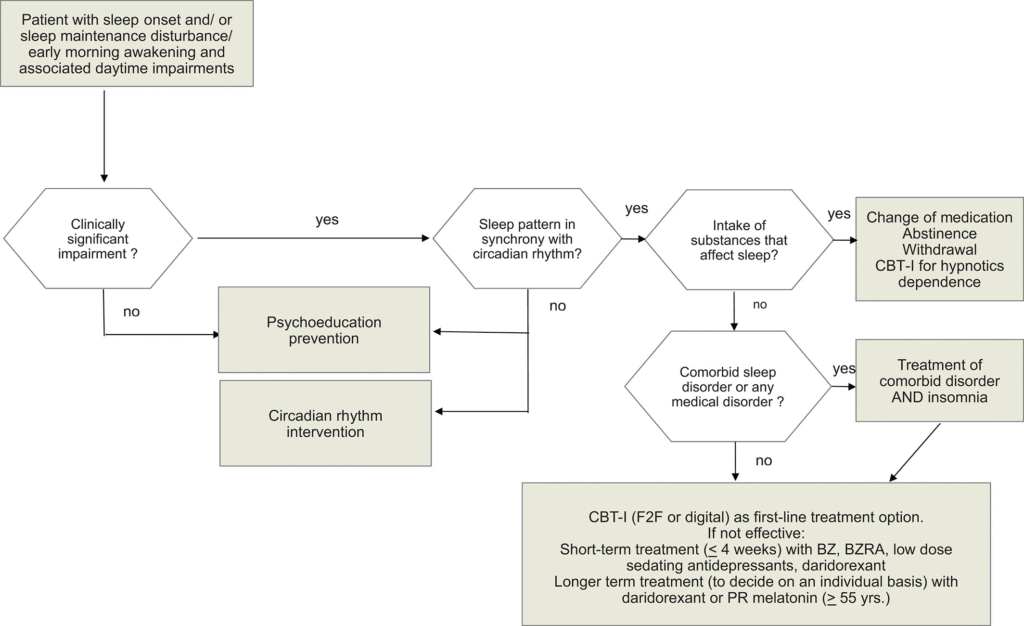
Algorithm
This is an algorithm adapted from the European Guideline which I find it useful and easier to follow. Kindly refer to the European Insomnia Guideline to read more about it.
References
- Schutte-Rodin S, Broch L, Buysse D, Dorsey C, Sateia M. Clinical guideline for the evaluation and management of chronic insomnia in adults. J Clin Sleep Med. 2008 Oct 15;4(5):487-504. PMID: 18853708; PMCID: PMC2576317.
- Riemann, D., Espie, C. A., Altena, E., Arnardottir, E. S., Baglioni, C., Bassetti, C. L. A., Bastien, C., Berzina, N., Bjorvatn, B., Dikeos, D., Dolenc Groselj, L., Ellis, J. G., Garcia-Borreguero, D., Geoffroy, P. A., Gjerstad, M., Gonçalves, M., Hertenstein, E., Hoedlmoser, K., Hion, T., … Spiegelhalder, K. (2023). The European Insomnia Guideline: An update on the diagnosis and treatment of insomnia 2023. Journal of Sleep Research, 32(6), e14035. https://doi.org/10.1111/jsr.14035
- Ng L, Cunnington D. Management of insomnia in primary care. Aust Prescr. 2021 Aug;44(4):124-128. doi: 10.18773/austprescr.2021.027. Epub 2021 Aug 2. Erratum in: Aust Prescr. 2021 Oct;44(5):177. doi: 10.18773/austprescr.2021.043. PMID: 34421177; PMCID: PMC8377300.
- Bastien, Celyne & Vallières, Annie & Morin, Charles. (2001). Validation of the Insomnia Severity Index (ISI) as an outcome measure for insomnia research. Sleep medicine. 2. 297-307. 10.1016/S1389-9457(00)00065-4.

