Hypothyroidism
Levothyroxine is the mainstay of treatment.
3 main aims of therapy:
i. Resolution of signs and symptoms
ii. Normalization of serum TSH with improvement in thyroid hormone concentration
iii. Avoid iatrogenic thyrotoxicosis or overtreatment especially in elderly
Initiating levothyroxine
Factors to be considered
- Body weight
- Degree of TSH elevation
- Etiology of hypothyroidism
- Pregnancy status
- Age
- Co-morbids, e.g. cardiac disease
Dosing
a) Normal healthy adults – 1.6 mcg/kg/day when serum TSH levels are markedly elevated, lower doses of 25- 50 mcg/kg/day can be also be used in milder degrees of hypothyroidism
b) Elderly (start low) – 25 or 50 mcg/day, increase by 25 mcg/day every 2 – 3 weeks until a full replacement dose is reached.
– For older patients > 70 – 75 years old, higher treatment target for serum TSH (~ 1 – 5 mIU/L) is acceptable.
c) Pregnancy – Generally require higher dosing. Those who are already on treatment before conception are recommended to have their dosage increased by up to 30 – 50% upon conception.
L-thyroxine can be started as an initial full replacement or as a partial replacement with gradual dose increments.
Dose adjustments should be made when there are significant changes in body weight, with pregnancy and ageing.
How to administer L-thyroxine
- Empty stomach (1 hr before breakfast or at bedtime, at least 3 hours after the last meal of the day), as food intake impair absorption.
- Try to fix the same time so that compliance may be enhance.
Be wary of medications/food/supplements that may interfere with iron absorption
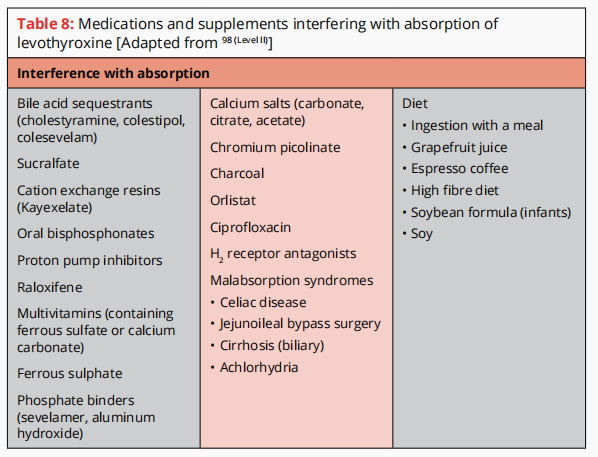
Medical conditions that may possibly affect L-thyroxine absorption
- Evaluation for GI disorders (H. pylori, atrophic gastritis, and coeliac’s disease) should be considered in patients requiring a much higher-than-expected dose of levothyroxine
Medication affecting metabolism of L-thyroxine
- Estrogen & androgens (may alter levothyroxine requirement)
- Tyrosine kinase inhibitors (affect thyroxine metabolism & thyroxin and tri-iodothyronine deiodination)
- Drugs that increase hepatic metabolism of T4 and T3
– Antiepileptics – phenobarbital, phenytoin, carbamazepine
– Rifampicin
– Sertraline - Reassessment of serum TSH should be done, if these medications/drugs were initiated.
Monitoring
Aim of treatment: Normalization of TSH and T3, T4 levels
Reassess serum TSH 4 – 8 weeks after initiating/dose adjustments.
Avoid overtreatment (iatrogenic thyrotoxicosis)/undertreatment
In cases of nonadherence, once weekly dosing (of the full week’s dose) has been shown to be effective and safe in reducing TSH levels and may be considered.
If patient was treated and serum TSH values have normalized, but still having persistent Sx, acknowledge their Sx and try to evaluate for alternative causes.
- Consider screening for other autoimmune diseases e.g. RA, SLE as the 2 most common causes of hypothyroidism are Hashimoto’s disease and thyroid ablation in Graves’ disease. Thus, there may be other associated autoimmune disorders.
For secondary hypothyroidism
- The primary biochemical goal is to maintain serum free thyroxine levels in the upper half of the reference range, but the level may be reduced in older patients or those with comorbidities and those at higher risk of complications of thyroid hormone excess.
Consider referral/endocrinologists involvement in:
- Children and infants
- Patients in whom it is difficult to render and maintain a euthyroid state
- Pregnancy
- Women planning conception
- Cardiac disease
- Presence of goitre, nodule, or other structural changes in the thyroid gland
- Presence of other endocrine diseases, e.g. adrenal and pituitary disorders
- Unusual constellation of TFT results
- Unusual cause of hypothyroidism, e.g. drug-induced hypothyroidism or by agents such as tyrosine kinase inhibitor
Subclinical hypothyroidism
Defined as raised serum TSH with normal serum T3 and T4 levels
Causes
Most common: Hashimoto’s disease (chronic autoimmune thyroiditis)
Other less common causes:
- Treated Graves’ diseases, TMNG and TA-radioactive iodine therapy
- Subtotal thyroidectomy
- Antithyroid drugs (intermittent, non-compliance)
- Head and neck surgery
- Radiation therapy to the head, neck or chest area
- Iodine deficiency
- Untreated primary adrenal insufficiency
- Medications: lithium, iodine, amiodarone
- Secondary hypothyroidism (hypopituitarism)
- Idiopathic
- Congenital
Transient elevations of TSH may be seen in:
- Subacute or painless thyroiditis
- Following withdrawal of L-thyroxine
- During recovery from a significant non-thyroidal illness
Clinical features
Patients with subclinical hypothyroidism may have Sx of mild thyroid failure e.g.
– Drier skin, poorer memory, slower thinking, weaker muscles, greater tiredness, more muscle cramps, more feeling cold, deeper and hoarser voice, puffier eyes, and more constipation (Colorado Thyroid Disease)
TSH level > 10 mIU/L predicts a higher rate of progression, and a level of < 6 mIU/L predicts a lower likelihood of progression.
Subclinical hypothyroidism is a/w elevated TC, LDL-C and TG levels and these lipid levels decrease with treatment.
Diagnosis
Subclinical hypothyroidism is a laboratory diagnosis
Investigation for raised TSH requires repeat measurements within 2 – 3 months to establish a firm diagnosis (as there may be transient elevation of TSH as mentioned above)
Determination of anti-TPO antibodies may be helpful in defining the risk of progression.
Course of disease
- Spontaneous recover – more likely in those with negative antithyroid antibodies and serum TSH levels < 10 mIU/L and within the first 2 years after diagnosis.
- Persist/unchanged
- Progression to overt hypothyroidism – more likely in those with positive antithyroid antibodies, serum TSH levels > 10 mIU/L, women)
Who are the population that would likely benefit from treatment in cases of subclinical hypothyroidism?
- High TSH level (> 10 mIU/L)
- Positive antibodies (anti-TPO)
- Presence of symptoms (fatigue, dry skin, constipation, etc)
- Pregnancy/infertility