Gout
A disease caused be monosodium urate (MSU)
crystal deposition
Image of “The Gout”, by James Gillray. Wikimedia Commons, CC BY
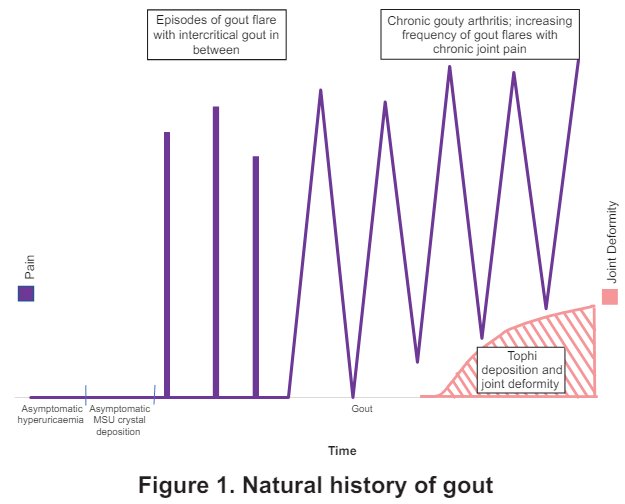
Natural History of Gout
- Asymptomatic hyperuricemia
- Asymptomatic MSU crystal deposition (without gout)
- Recurrent gout flares with intercritical gout
- Gout with chronic gouty arthritis/tophaceous gout/erosive gout
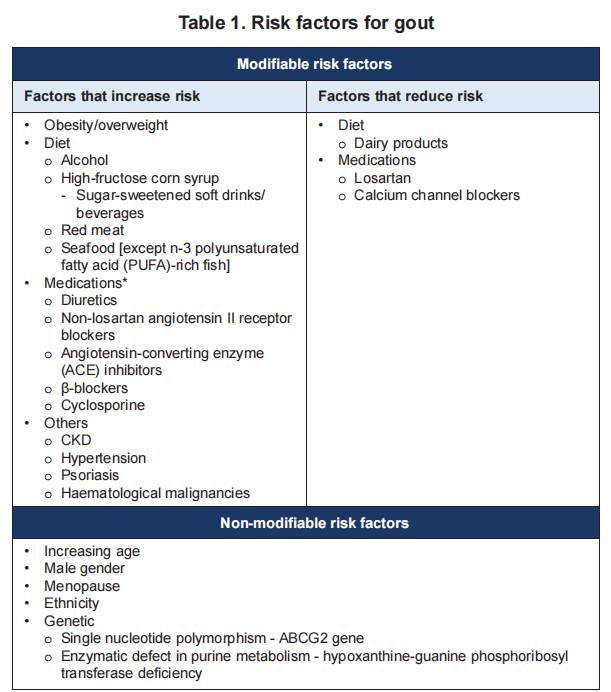
Risk factors
3 clinical classical stages
- Gout flare – acute arthritis induced by MSU crystals
- Intercritial gout – asymptomatic period after or between gout flare
- Chronic gouty arthritis +/- tophi – joint deformity e.g. fixed flexion deformity


- 1st presentation of acute gout: typically acute monoarthritis of the 1st MTP joint (podagra), midfoot or ankle. Less commonly with oligoarthritis; Self-limiting, lasting about 1 – 2 weeks.
- If hyperuricemia persist –> recurrent flares –> polyarticular gout (including those of upper limb)
- Common sites of tophi: 1st MTP joint, Achilles tendon, peroneal tendon, helix of the ear, olecranon bursa & finger pad.
Extra-articular manifestation: Urolithiasis, Chronic nephropathy (Thus, don’t forget to assess also patient’s Renal Function)
Diagnosis 🔬
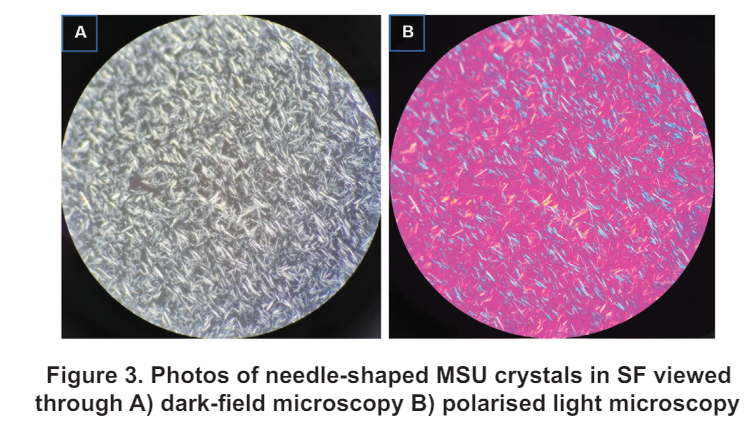
Definite (gold standard): Demonstration of MSU (negative birefringent crystals) in synovial fluid or tophus.
Often time, this may not be possible, thus diagnosis can be made from clinical presentation, lab investigations & imaging modalities.
Laboratory investigations
Mainly serum uric acid (SU)
– Cut-off level to diagnose hyperuricemia: > 6.8 mg/dL (408 umol/L; 0.408 mmol/L) at physiological pH & body temperature.
Keep in mind that:
– Diagnosis of gout should not be made based on hyperuricemia alone.
– A normal/low SU during flare does not exclude gout as level may be normal during flare. If clinical suspicion is high, SU may be repeated 2 weeks or more after complete resolution of flare.
Imaging modalities
X-ray & ultrasound
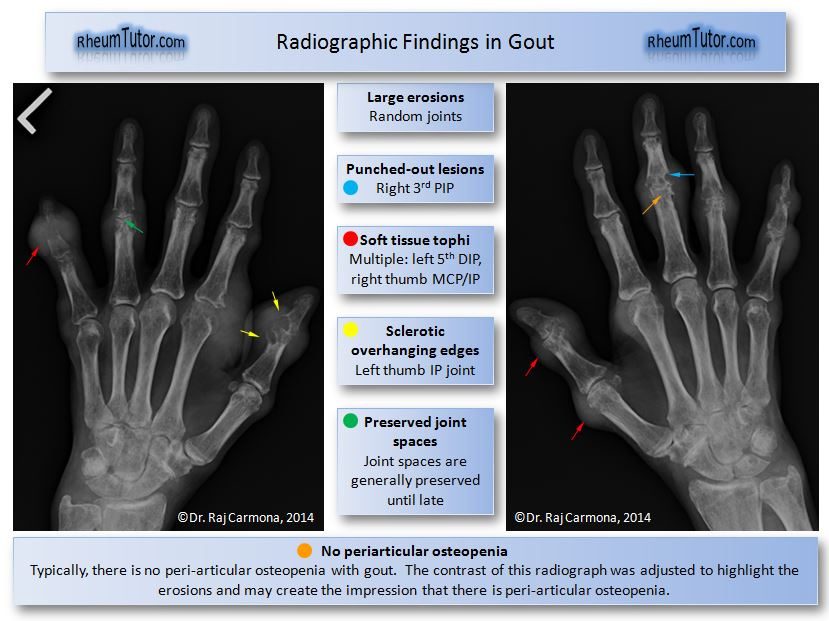
Typical radiographic features of gout on plain radiograph:
– Bone erosions with overhanging edges and a sclerotic rim (“punched out”/”rat bite” erosions)
– Bony proliferation
– Joint space are generally preserved until late stages of the disease
– No peri-articular osteopenia
– Soft tissue tophi +/- calcification
ACR/EULAR gout classification criteria
Utilizes laboratory, imaging and clinical criteria to aid in diagnosis
Score of >= 8 can be classified as having gout
Accessible via: https://goutclassificationcalculator.auckland.ac.nz/
Co-morbidities
Gout is an independent risk factor for mortality due to coronary heart disease & kidney disease.
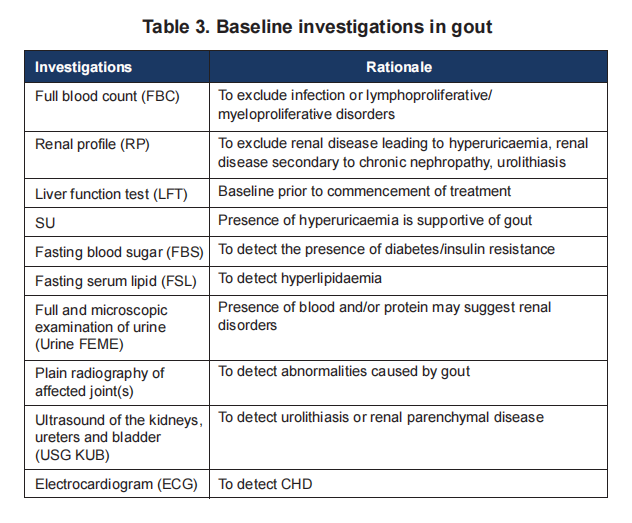
Screening for comorbidities e.g. HTN, DM, Dyslipidemia, CHD, & renal disease including urolithiasis should be done upon diagnosis & during follow up.
Below are the suggested baseline investigations which include screening for comorbidities as given in our Malaysia CPG guidelines.
Differential diagnosis
- Septic arthritis
– Commonly involves knee joint (other sites: hip, shoulder, ankle, wrist)
systemic features e.g. fever, ill or septic-looking
– Risk factors e.g. concomitant bacteria infection, recent intra-articular injection
– Leucocytosis and increased CRP - Acute calcium pyrophosphate crystal arthritis
– Age > 60 y/o
– Involvement of a degenerative joint
– Plain radiograph: chondrocalcinosis - Psoriatic arthritis
- Reactive arthritis
– Recent genitourinary or GI infection.
– Presence of urethral discharge or ulcer, rash on soles, conjunctivitis.