GERD

Gastroesophageal Reflux Disease
Occurs when reflux of stomach contents lead to troublesome symptoms &/or complications
Pathophysiology
The normal antireflux barrier consists of – intrinsic pressure of lower esophageal sphincter (LES) , the extrinsic compression of the LES by crural diaphragm and the acute angle of His.
Multiple mechanism that may cause reflux

- Transient LES relaxation (have been thought of as the most common mechanism) – mainly a postprandial phenomenon whereby gastric distension due to gastric air/presence of meal triggers transient relaxation.
- Acid pocket – presence of pocket of unbuffered gastric acid just below the EG junction which is exclusively postprandial & can be found in both normal person & GERD patients.
- LES hypotension (frequently in patients with scleroderma)
- Anatomical disruption of the esophago-gastric junction due to hiatal hernia
- Esophageal motility disorders
- Delayed gastric emptying (Gastroparesis)
Understanding these mechanisms can help us to understand the treatment options better.
Clinical features
Typical symptoms: Heartburn and regurgitation
Others (less common) – chest pain & dysphagia
Extra-esophageal symptoms: chronic cough, hoarseness, throat clearing, laryngitis, pharyngitis, asthma, dental erosions
(It is important to rule out other potential causes first for these symptoms before attributing to GERD)
Complications: reflux esophagitis, strictures, Barrett’s oesophagus
GERDQ questionnaire 📃
Can aid in the clinical diagnosis of likelihood GERD
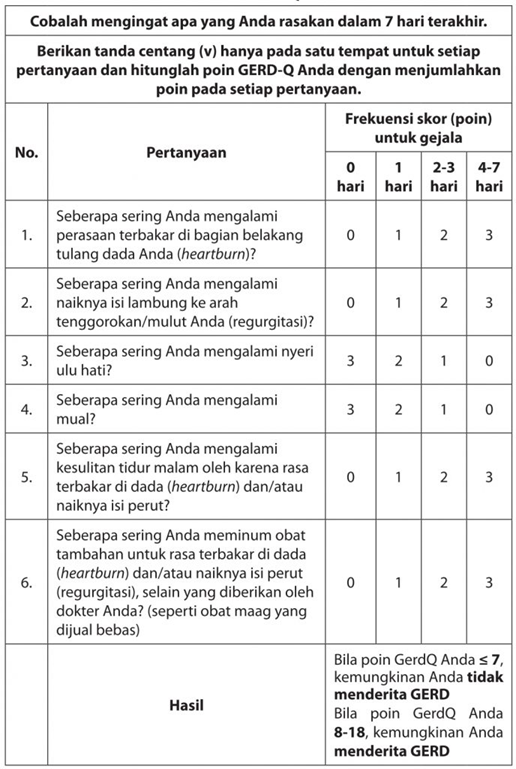
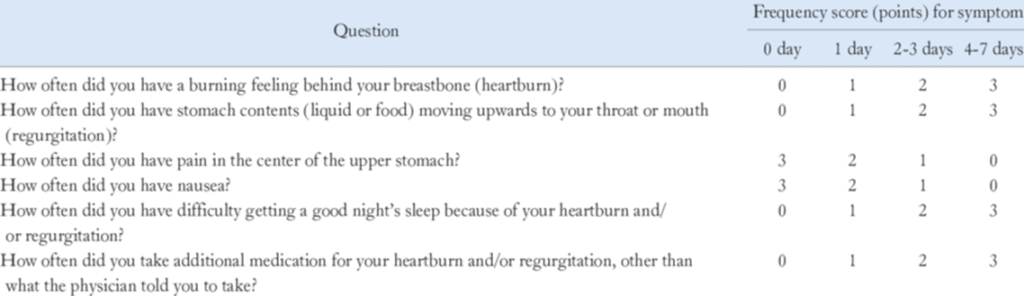
Score of 0 – 2 points: likelihood of GERD is 0%
Score of 3 – 7 points: likelihood of GERD is 50%
Score of 8 – 10 points: likelihood of GERD is 79%
Score of 11 – 18 points: likelihood of GERD is 89%
Alarming features 🚨
- New onset dyspepsia in patient ≥ 60 years old
- Evidence of GI bleed (hematemesis/melena/hematochezia/occult blood in stool)
- Iron deficiency anemia
- Anorexia
- Unexplained weight loss
- Dysphagia
- Odynophagia
- Persistent vomiting
- GI cancer in 1st degree relative
Investigations 🔎
GERD can be objectively defined by presence of:
– Characteristic mucosal injury seen at endoscopy &/or
– Abnormal esophageal acid exposure demonstrated on reflux monitoring study.
Nevertheless, there are no gold standard test.
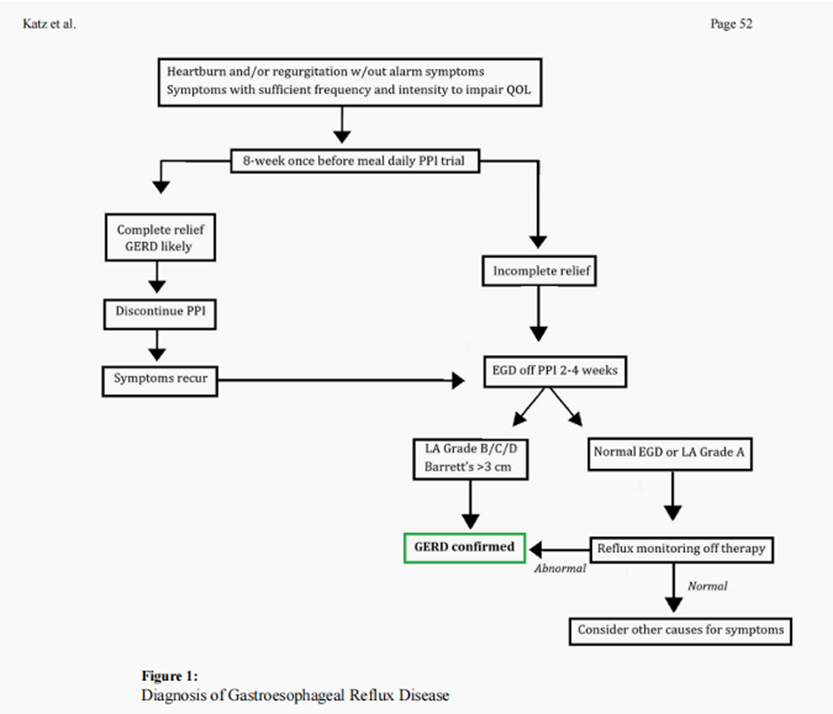
Diagnosis is often based on combination of symptoms, endoscopic evaluation of esophageal mucosa, reflux monitoring, & response to therapeutic intervention.
- Therapeutic trial of PPI as diagnostic “test” – may be more applicable at primary care setting.
- Endoscopic evaluation – The Los Angeles (LA) classification of erosive esophagitis.
- Ambulatory Reflux monitoring (pH or impedance-pH) – wireless telemetry capsule or transnasal catheter-based testing
- Esophageal Manometry – TRO esophageal motility disorder and important to perform prior to any antireflux procedure.
The diagnosis of GERD in pregnancy is almost always symptoms based (heartburn), rarely requiring endoscopy & pH monitoring.
Non-pharmacological management (Lifestyle modifications)

- Weight loss for overweight & obese patients.
- Avoiding meals within 2 – 3 hours of bedtime.
- Avoidance of tobacco products.
- Avoidance of potential “trigger foods” based on individuals,
i.e to avoid these foods only if it is known to trigger GERD symptoms for that individual. These foods may include coffee, chocolate, carbonated beverages, spicy foods, acidic foods like citrus & tomatoes, & foods with high fat content. - Elevating head of bed for nighttime GERD symptoms. In addition, lying right-side down increases nocturnal reflux & reflux aftermeals and thus should be avoided.
Pharmacological treatment
Acid control is considered as the 1st line of pharmacological treatment. Available options include proton pump inhibitors (PPI), H2 blocker and antacids.
In regards to all the available options, PPIs have been considered 1st line as it is more potent than H2-receptor antagonists in reducing acid secretion.
Regarding PPIs
- Can bind only to proton pumps that are actively secreting acid (usually stimulated by meals)
- Thus, PPIs should ideally be given 30 – 60 mins before meals (either before breakfast for OD dosing or before breakfast and dinner for BD dosing)
- Conventionally the regimen is OD dosing, but may be increased up to BD dosing if symptoms not improving
- BD PPI therapy is superior to OD double dose PPI therapy.
- There might be a wide variation in pH control between PPIs, thus the rational for considering switching PPIs.
- In terms of managing extra-oesophageal symptoms, the role of PPI is still controversial (no strong evidence).
- Maintenance PPI therapy should be administered for patients with GERD complications e.g. severe EE & Barrett’s oesophagus.
- For those without complications but who continue to have symptoms when PPI is discontinued, PPIs can be given on-demand (only when symptoms occur).
Long-term use of PPIs
There are concern regarding the adverse effects on prolonged used including intestinal infections, pneumonia, stomach cancer, osteoporosis related bone fracture, CKD, heart attacks, stroke, vitamins/mineral deficiency (e.g. Magnesium)
Nevertheless, high-quality studies have found that PPIs do no significantly increase the risk for any of these conditions except intestinal infection. (Established benefits outweigh their highly questionable CV risks).
Switching PPIs can be considered for patients who have minor side effects e.g. headache, abdominal pain, nausea, vomiting, diarrhea, constipation & flatulence.
PPIs can be used in patient with renal insufficiency with close monitoring of RP or consultation with nephrologist.
Antacids
Used mainly for on-demand symptom relief.
There has been consensus that alginate containing antacids may be more effective in treating GERD symptoms and could be considered for patient with mild to moderate GERD. Nevertheless, PPIs are still usually the mainstay of treatment for true GERD.
Regarding prokinetic agents
Examples: metoclopramide, domperidone, itopride, etc
Should not be routinely used in GERD management as there are no high-quality evidence to support its use. However, it may be considered especially when GERD is attributed to gastroparesis.
Refractory GERD
It is considered refractory only if the patient has been on PPIs BD dose for 8 weeks and still symptomatic without improvement.
Consider these conditions:
- Regarding PPI – Suboptimization, improper timing, non-compliance
- Difference in PPI metabolism – activity of CYP2C19 is determined by genetic polymorphism
- Non-erosive reflux disease, whereby there are typical reflux symptoms but with weakly acidic content. (No erosive esophageal lesion demonstrated at endoscopy)
- Reflux hypersensitivity
- Functional heartburn – Symptoms without any reflux
- Esophageal motility disorders
In cases of Refractory GERD, it is advisable to refer Gastro for further diagnostic assessment.
These may include:
- Upper GI endoscope: to assess any erosive esophagitis (LA classification),
- Impedance-pH monitoring: to assess on symptoms association with either acid or weakly acidic refluxes (NERD)
- Esophageal manometry: TRO esophageal motility disorders
For Refractory GERD who is true GERD after assessment, management options may include:
- Optimize PPI therapy & check for patient’s compliance.
- Consider adding to PPIs:
– Alginate – mucosal protective & able to neutralize or displace the acid contained in the acid pocket.
– Medical devices containing hyaluronic acid
– H2-receptor antagonists (e.g. ranitidine, cimetidine) – may be more beneficial for those with nocturnal symptoms
– Bile acid sequestrants (IW-3718) - Consider vonoprazan (Potassium Competitive Acid Blockers – P-CABs) as an alternative to PPIs
- Consider pain modulators in case of hypersensitivity
- Consider anti-reflux surgery
Treatment of GERD in pregnancy
Start with lifestyle modification.
If fail, consider starting antacids as first line (aluminium-, calcium-, or magnesium-containing), alginates, and sucralfate.
All H2 blockers are FDA category B.
All PPIs are FDA category B except omeprazole, which is category C.
Extra-oesophageal symptoms
Evaluate for non-GERD causes first.
In those with extra-esophageal Sx without typical GERD Sx (heartburn, regurgitation), it is recommended to undergo reflux testing for evaluation prior to PPI therapy.
For those with extra-esophageal Sx and typical GERD symptoms, consider trial of PPI BD for 8 – 12 weeks prior to further test (low level of evidence).
Surgical/Endoscopic anti-reflux procedures are only recommended in patients with objective evidence of reflux.
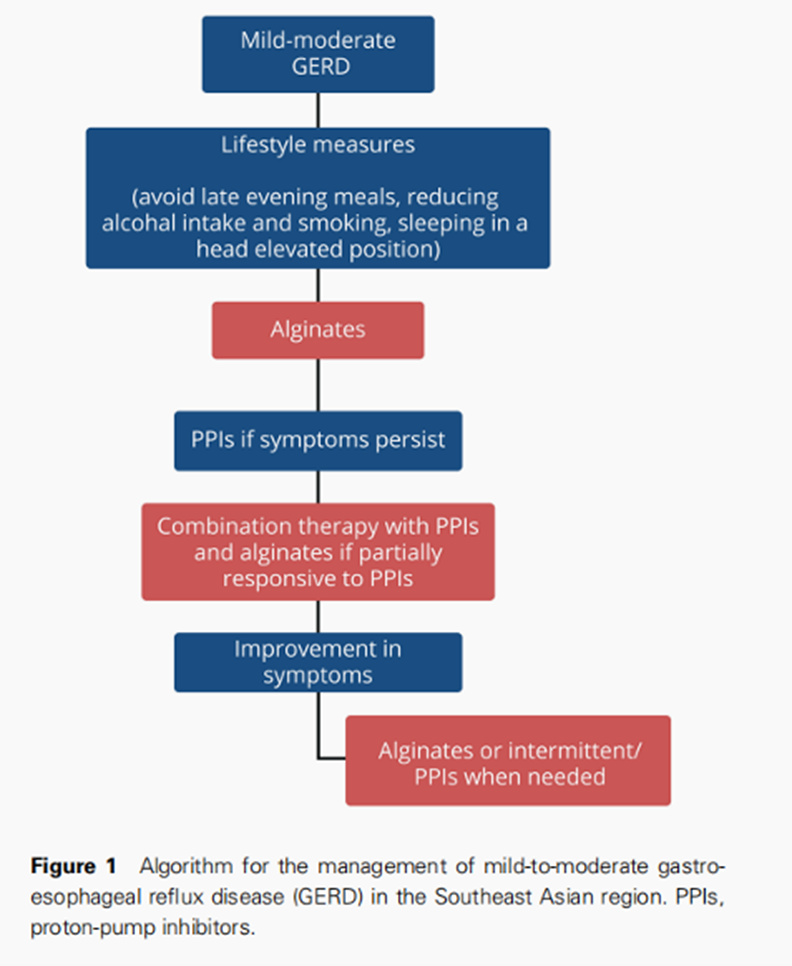
Algorithm