Erectile Dysfunction

Erectile Dysfunction
General features
Definition: Persistent inability to achieve or maintain an erection sufficient for satisfactory
ED can be due to organic, psychogenic & mixed aetiologies.
Organic causes may include:
- Vascular
- Neurologic
- Psychological (e.g. performance anxiety, psychological causes)
- Hormonal
- Medication & substance use
– SSRIs e.g. citalopram, fluoxetine, paroxetime, sertraline
– SNRIs
– Antihypertensives e.g. thiazide diuretics, ß-blockers
– 5α-reductase inhibitors (treatment for BPH)
– Tobacco, alcohol & illicit drug use
Conditions that are commonly associated with ED includes DM, HTN, hyperlipidemia, ESRD, obesity, testosterone deficiency, chronic prostatitis/chronic pelvic pain syndrome & prostate cancer treatment, etc.
Erectile Dysfunction (ED) and Cardiovascular Disease (CVD)
Both share similar risk factors e.g. older age, HTN, dyslipidemia, smoking, obesity & diabetes.
ED is likely an independent risk factor for CVD, with predictive value comparable to smoking or a family history of heart disease.
It may also serve as an early indicator of coronary artery disease (CAD), often appearing 2 – 5 years before CAD develops — offering a critical opportunity for early intervention & lifestyle changes.
In younger men & minorities, in which the conventional global risk assessment calculators may underestimate the actual risk, ED may be a useful marker for assessing their CV risk.
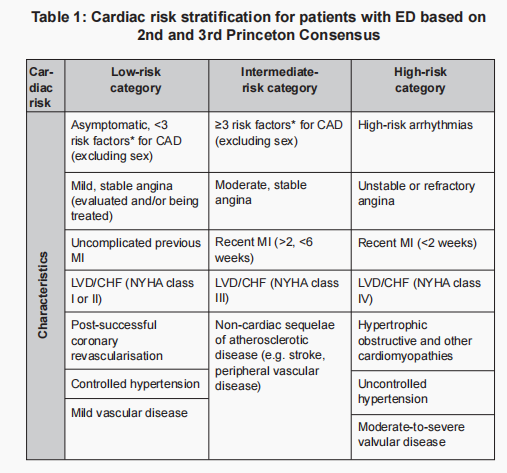
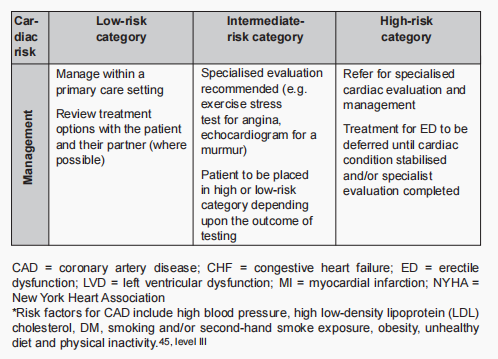
Patients with ED should have cardiac risk assessment (as below) & vice versa.
Cardiac risk stratification for patients with ED and its management plan (Malaysia CPG guideline)
History taking
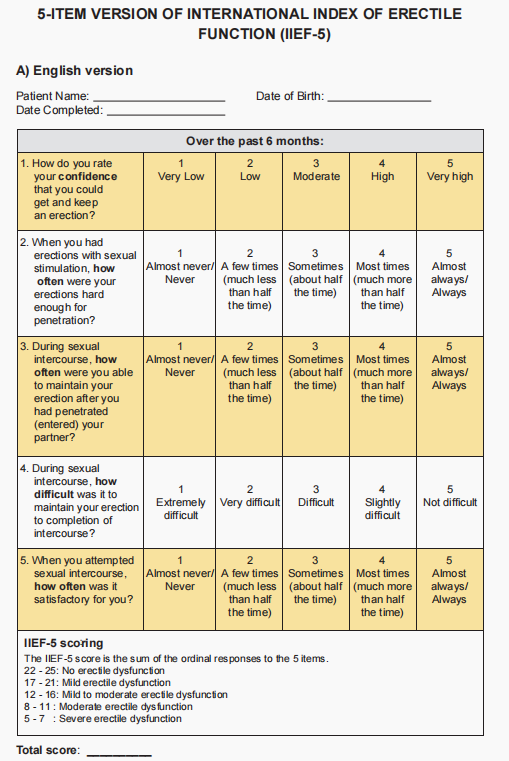
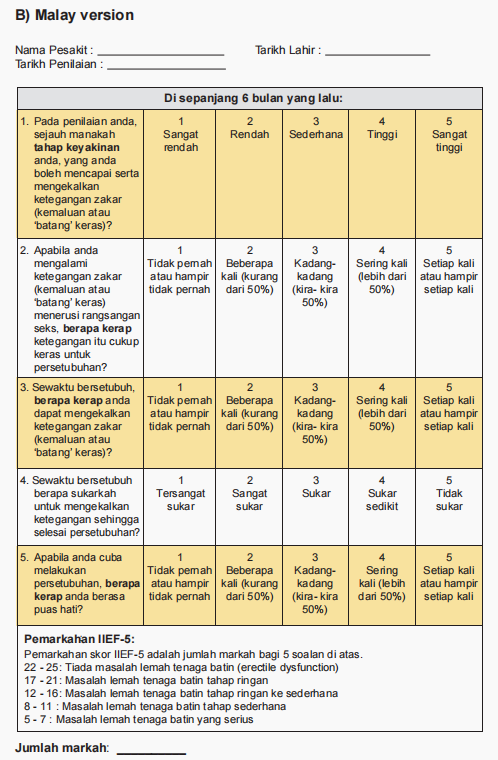
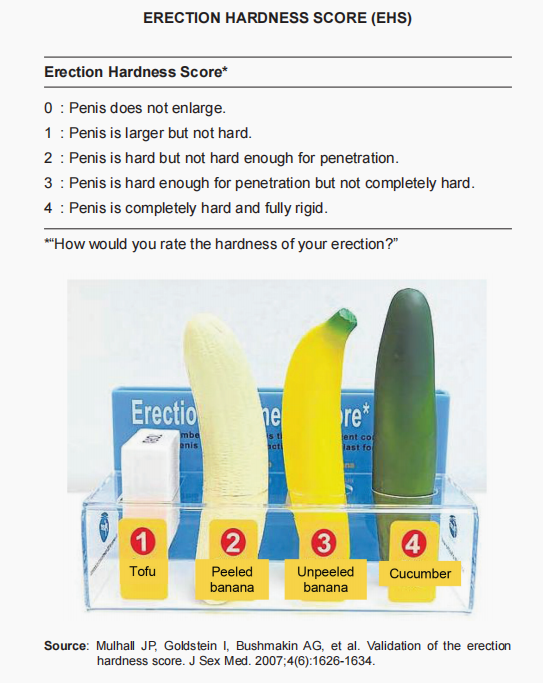
1. Using IIEF-15 or its short version IIEF-5 to assess ED severity (Can be used together with Erectile Hardness Score [EHS])
2. Medical & surgical history
3. Sexual related history/factors
- Education
- Trauma
- Experience e.g. masturbation, pornography usage
- Cultural & religious aspects
- Gender dysphoria & sexual orientation
4. Co-morbid sexual dysfunction (e.g. premature ejaculation)
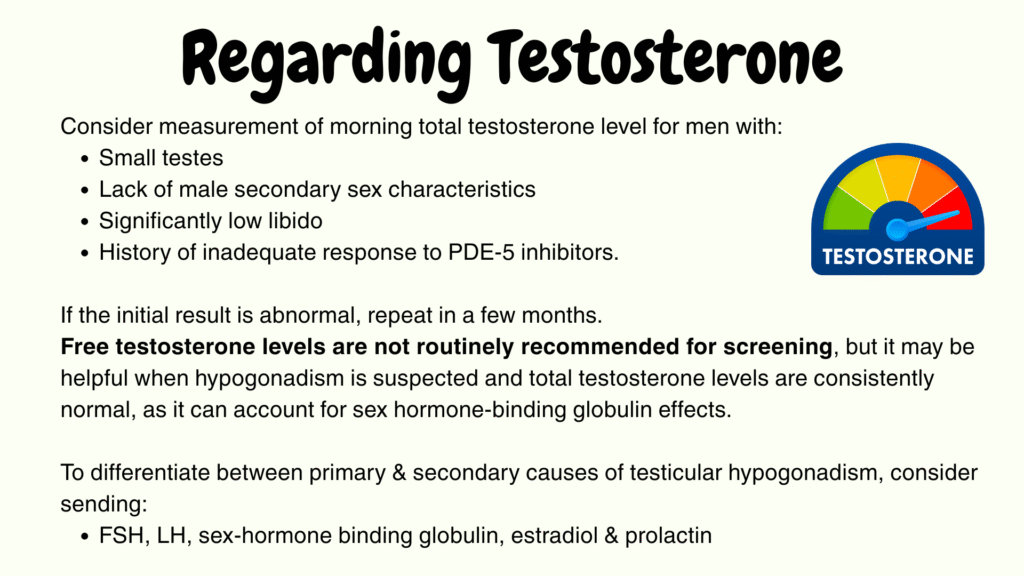
5. Screen for symptoms of possible hypogonadism, e.g. decreased energy & libido
6. Use of medications & other substances
7. Psychological & relationship health
- Current psychological state & co-morbid psychiatry conditions (e.g. anxiety, depression)
- Life stressors & coping abilities
- Cognitive factors – dysfunctional thinking style, expectations on sexuality & sexual performance & treatment preferences.
- Relationship history – issues, dynamics, durations & partner history
- Partner’s sexual functioning (e.g. FSD)
Physical examination
1. CV risk assessment: BP, BMI, waist circumference
2. Genital examination (include prostate)
- May reveal penile abnormalities (e.g. Peyronie’s disease), pre-malignant or malignant genital lesions, prostatic enlargement or small testes (signs suggestive of hypogonadism)
3. Male secondary sex characteristics (TRO hypogonadism)
4. The endocrine, vascular & neurological system should also be assessed.
Investigations
CV risk assessment: HbA1c, Fasting glucose, Lipid profile
TFT if having signs or symptoms of hypothyroidism
Testosterone (as needed)
Advanced work-up
Indications
- Primary ED (not due to acquired organic disease or psychogenic disorder)
- Young patients with h/o pelvic or perineal trauma suspected to have vasculogenic ED.
- Patients with penile deformities that might require surgical correction (e.g. Peyronie’s disease & congenital penile curvature)
- Patients with complex endocrine disorders
- Patients with complex psychiatric or psychosexual disorders
- Medico-legal reasons (e.g. implantation of penile prosthesis, to document end-stage ED and sexual abuse)
What are the advanced work-up?
- Nocturnal penile tumescence & rigidity test (NPTR)
- Vascular studies (to assess for potential vasculogenic aetiology) may include:
– Intracavernous injection test
– Duplex ultrasonography
– Arteriography - Specialised endocrinological studies
- Specialised psycho-diagnostic evaluation
Regarding NPTR
- The device has to be won by the patient overnight for at least 2 separate nights & gives the following information:
– Number of erectile episodes
– Tumescence (circumference change by strain gauges)
– Maximal penile rigidity
– Duration of nocturnal erections - An erectile event lasting >= 10 mins & with at least 60% stiffness observed on the penis is indicative of a functional erectile mechanism.
- Objective assessment of organic vs psychogenic ED. (Psychogenic ED usually have normal findings).
- Use may be limited due to potential confounding factors (e.g. dreams) which may affect nocturnal erection.
Treatment
Include lifestyle modifications, pharmacological management, mechanical devices, surgeries & psychological interventions.
Shared decision-making (preferably with a partner) is important in ED management.
A. Lifestyle & risk factor modification
Regular exercise, weight loss if obese or overweight, optimization of DM, HTN and hyperlipidemia.
Tobaccos cessation is highly recommended.
EAU guidelines 2023 recommends to modify risk factors & commence lifestyle changes prior to or concurrently with ED treatments.
B.💊 Medications (Pharmacological)
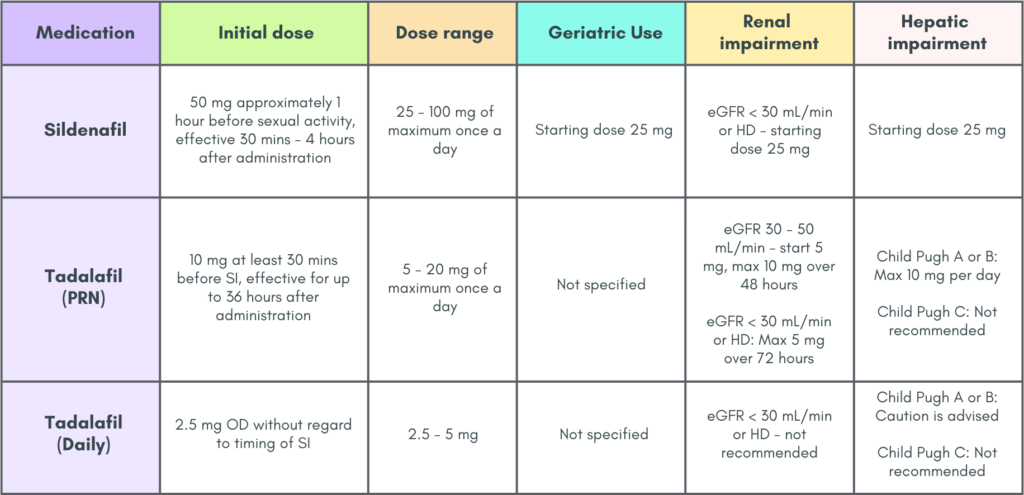
Oral PDE-5 inhibitors = first line. Should be offered to all patients with ED unless contraindicated. This is consistent with EAU Guidelines 2023 where PDE5i is recommended as a 1st line therapeutic option. Choice of agent is individualized.
- These agents are not initiators of erection. Sexual stimulation is needed to produce an erection where the erection is then sustained by oral PDE-5 inhibitors by enhancing the vasodilatory effects of endogenous nitric oxide.
- Examples of these agents: Avanafil (Stendra), Sildenafil (Viagra), Tadalafil (Cialis), Vardenafil (Levitra)
Common features
Common Adverse Effects
- Headache
- Flushing
- Dyspepsia
- Nasal congestion
- Nasopharyngitis
- Back pain
- Myalgia
- Visual abnormalities
Caution
- Patient should stop PDE5i immediately & seek medical attention when there is a sudden loss of vision in one or both eyes which could be a sign of non-arteritic anterior ischemic optic neuropathy (NAION)
- Advise patient to seek emergency treatment if erection last > 4 hours. Use PDE5i with caution in patients predisposed to priapism.
Caution
- If using nitroglycerin or other nitrates due to risk of catastrophic hypotension
(Gap of 24 hours is required between the last dose & usage of nitrate) - Known hypersensitivity to PDE5i or any component of the tablet.
Common dosage of PDE5i (Only Sildenafil and Tadalafil are mentioned here)
C. Procedural therapy (2nd line) – Alprostadil, vacuum therapy, shockwave therapy
Can be used to establish an erection before sexual stimulation.
Should be avoided in men who are on anticoagulants, have sickle cell disease or other bleeding/clotting disorders.
Alprostadil – the only FDA approved preparation
- Cause penile vasodilation by relaxing arterial smooth muscle.
- Available in 2 forms: injectable (administered intracavernosally into on side of the penis) & intraurethral (dissolvable pellet is placed into the urethra with an applicator)
- Can be used in combination with PDE-5 inhibitors.
- The lowest effective dose should be used.
- Patients should be warned to seek emergency urologic treatment if an erection last 4 hours or longer
- Penile fibrosis is a possible adverse effects.
- Not available locally yet
Vacuum device
- A vacuum pump removes air from the tube, pulling blood into the penis & creating an erection.
- A constricting ring is then slid off the base of the tube into the penis to maintain the erection.
- The constricting ring should generally not be left in place for > 30 mins to prevent ischemic damage.
- Can be used in combination with PDE-5 inhibitor or alprostadil for men who have not had success with single-component treatment.
- Useful in men receiving daily nitroglycerin or other long-term nitrate therapy where PDE-5 inhibitors are contraindicated.
Low-intensity extracorporeal shockwave therapy
- Should only be performed by urologists
- May be considered in patients with:
– Mild vasculogenic ED
– As an alternative therapy for those who do not wish to have/not suitable for oral PDE5is.
– Vasculogenic ED who do not respond to PDE5is
D. Surgical intervention
- Prosthesis (3rd line)
- Penile revascularization surgery – may be considered for vascular ED.
E. Others
There is insufficient evidence to recommend the use of TCM including Tongkat Ali in ED treatment (Malaysia CPG guideline)
Nevertheless, the EAU guidelines mentioned that supplements with L-arginine or ginseng daily may be considered for men with mild ED who refuse pharmacological treatment. However, it is a weak recommendation & patient should be informed & counselled that the improvement could be mild.
Management of Psychogenic ED 🧠
Occurs at all ages but is most common in men younger than 40 years.
Some factors that may lead to psychogenic ED:
- Premature ejaculation
- Genital pain
- Dyspareunia
- Cultural or religious taboos
- History of sexual abuse
Psychogenic cause are more likely when patient has normal erections with masturbation or when nocturnal penile tumescence is normal.
Psychological intervention can include:
- Psychoeducation
- Cognitive behavioral therapy – to reduce anxiety, challenge dysfunctional beliefs, increasing intimacy & communication skills in a relationship, etc
- Sex therapy (specific type of psychotherapy, focusing mainly on sexual experiences
When ED coexists with depression/anxiety, treatment of the mood disorder may be the most appropriate first step.
- Use antidepressant that is less likely to worsen ED (e.g. buproprion, mirtazapine, fluvoxamine)
- PDE-5 inhibitors are effective in men with depression & can be used in combination with treatments for mood disorders
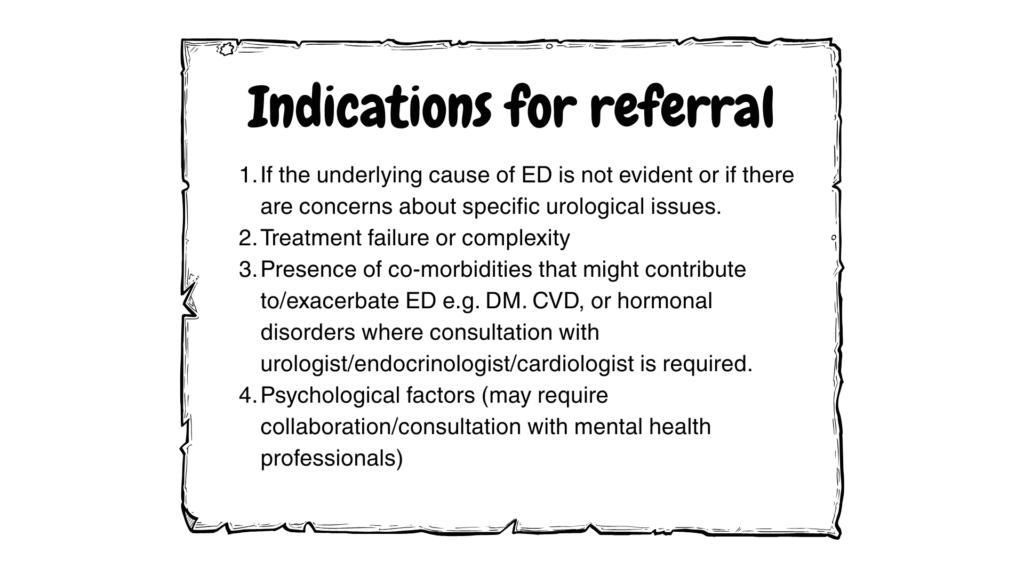
Follow up (should be individualized)
Short term (within few week to a couple of months): For patients started on oral medications, to assess response & tolerance to the medication.
Long term (at regular intervals): To assess treatment effectiveness, potential adjustments to treatment plan & monitoring for any emerging health issues.
As needed follow up: For patients using PRN treatments or lifestyle modifications
References
- Management of Erectile Dysfunction (2024) Malaysia Clinical Practice Guideline.
- Rew KT, Heidelbaugh JJ. Erectile Dysfunction. Am Fam Physician. 2016 Nov 15;94(10):820-827. PMID: 27929275.
- Salonia A, Bettocchi C, Boeri L, Capogrosso P, Carvalho J, Cilesiz NC, Cocci A, Corona G, Dimitropoulos K, Gül M, Hatzichristodoulou G, Jones TH, Kadioglu A, Martínez Salamanca JI, Milenkovic U, Modgil V, Russo GI, Serefoglu EC, Tharakan T, Verze P, Minhas S; EAU Working Group on Male Sexual and Reproductive Health. European Association of Urology Guidelines on Sexual and Reproductive Health-2021 Update: Male Sexual Dysfunction. Eur Urol. 2021 Sep;80(3):333-357. doi: 10.1016/j.eururo.2021.06.007. Epub 2021 Jun 26. PMID: 34183196.
