
Dyslipidemia
Definition
- Total cholesterol (TC) > 5.2 mmol/L
- HDL-C < 1.0 mmol/L (males); < 1.2 mmol/L (females)
- TG > 1.7 mmol/L
- LDL-C levels (will depend on the patient’s CV risk)
– Optimal values for both gender is < 2.6 mmol/L
Risk stratification
The Framingham Risk Score can be used to risk stratify patients.
All individuals should be risk stratified.
The intensity of risk factor reduction & target lipid levels will depend on their CV risk.
- Those with high or very high risk should be treated aggressively from the outset with non-pharmacological measures & pharmacotherapy to achieve treatment targets.
- In low or intermediate risk patients, the decision to initiate pharmacotherapy should be individualized following a mutual discussion with the patient.
Target LDL-C according to CV risk
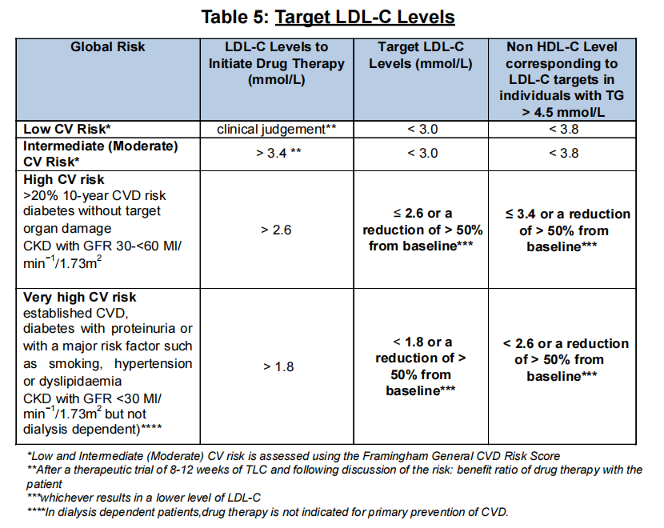
LDL-C is the primary target of therapy
Non-HDL-C may be considered as a secondary target when treating patients with:
- Combined hyperlipidemias
- Diabetes
- Cardio metabolic risk
- CKD
- Non-HDL-C becomes the primary target of therapy in individuals where the TG > 4.5 mmol/l.
For pt with HTN, initiate statins for primary prevention if they also have elevated cholesterols (LDL-C > 3.4 mmol/L).
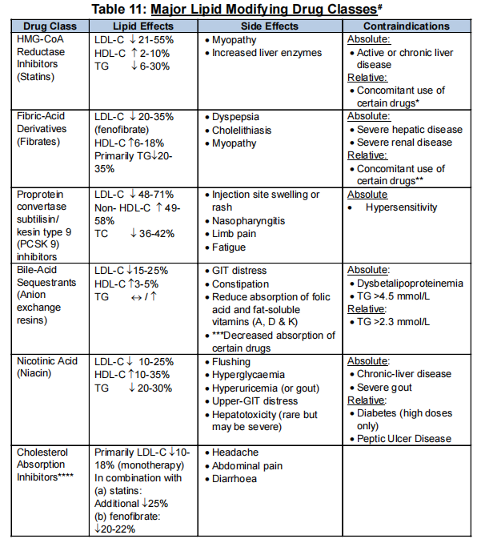
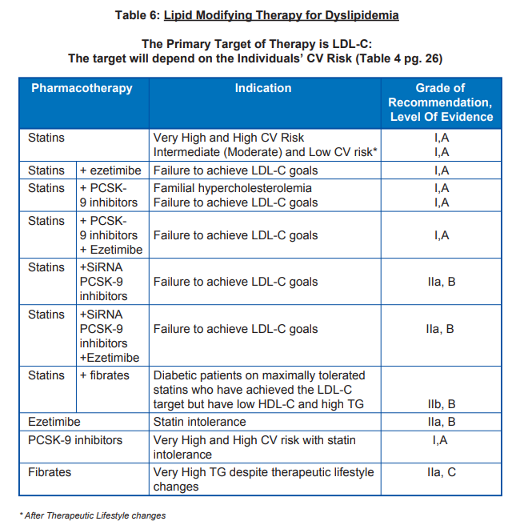
Medications
In concurrent with medications, all patients regardless of CV risk should be counselled & advised for therapeutic lifestyle changes including diet, exercise & quit smoking.
Statins
Contraindications
- In pregnancy & lactation.
- Should not be prescribed to women of child bearing potential unless adequate contraception is taken. If pregnancy is planned, then statins should be discontinued.
Decision to start which type of statin and its appropriate dosage depends on the patient’s CV risk.
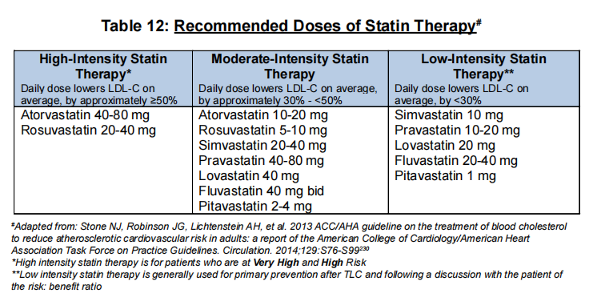
Main adverse effects of concern
1. Liver function
- Hepatic transaminases should be measured at baseline & at 1 – 3 months.
- If levels are elevated prior to therapy, other causes (e.g. fatty liver, hepatitis) should be excluded. If d/t fatty liver, lipid lowering therapy is not contraindicated.
- When transaminase levels (esp ALT) are > 3 times the upper limit of normal on 2 occasions, the drug should be stopped.
- Cautious reintroduction may be considered under close monitoring after ALT values normalized.
- Progression to liver failure is rare. Routine monitoring of ALT during long term statin treatment is no longer recommended.
2. Muscle symptoms – statin-associated muscle symptoms (SAMS) 💪🏻
- Includes:
- Myalgia (normal creatine kinase [CK])
- Myositis (CK > ULN)
- Rhabdomyolysis (CK > 10X of ULN)
- CK is not routinely measured unless myositis is suspected. If the level is > 5x the ULN on 2 occasions, the drug should be discontinued.
- When a statin myopathy is suspected, the 1st step is statin discontinuation for 2 – 3 weeks.
- If symptoms have not resolved, then unlikely statin related & pt can continue on same dose of statin.
- If symptoms resolved, then consider:
– Lowering dose/frequency to less than daily.
– Alternative dosing e.g. EOD or twice a week with atorvastatin/rosuvastatin.
– Highest tolerable dose of statin + cholesterol absorption inhibitor (ezetimibe)
– PCSK9 inhibitor - Alternative approach: consider co-enzyme Q10 to alleviate myalgia Sx.
- Care should be taken when prescribing high doses of simvastatin (> 20 mg/daily) together with certain other medications that inhibit cytochrome P450 pathway. It has the potential of increasing the risk of muscle injury.
Cholesterol absorption inhibitors (ezetimibe)
- Used in combination with any dose of any statin to further lower LDL-C if targets are not achieved.
- May be considered as monotherapy in pt who cannot tolerate statins.
- Recommended dose: Ezetimibe 10 mg OD
PCSK9 inhibitors
- Decreases the degradation of the LDL-receptors –> higher LDL-receptors density at the cell surface.
- Only available as SC injection at 2 – 4 weeks interval.
- Common A/E: injection-site swelling, flu-like Sx, nausea & joint pains.
- Possible indications:
– Pt with high CV risk who have persistently elevated LDL-C despite optimum lipid-modifying therapy.
– Familial hypercholesterolemia
– Very high risk & high risk patient with true statin intolerance & persistently high levels of LDL-C - Recommended dose:
– Evolocumab: 140 mg SC every 2 weeks or 420 mg SC monthly.
– Alirocumab: 75 – 150 mg SC every 2 weeks.
Fibrates
- PPAR-a agonist: fatty acid oxidation.
- Reduce serum TG effectively & increase HDL-C modestly.
- Use is limited to those with very high TG levels who do not respond to non-pharmacological measures.
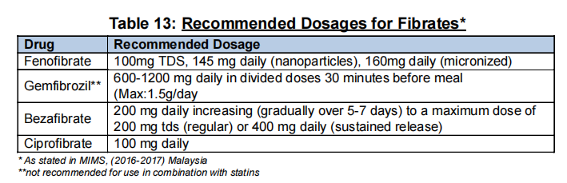
Dose need to be adjusted in the presence of CKD. Serum ALT should be monitored when starting therapy or when doses are increased.
Combination therapy
Combination therapy is used when LDL-C targets are not achieved despite optimal statin dose or maximally tolerated statin dose.
Combinations that may be used:
- Statin + cholesterol absorption inhibitors (ezetimibe)
- Statin + fibrates
– Fibrates increase the risk of myopathy with statins, & the risk is highest for gemfibrozil.
– The risk with gemfibrozil is 15 times higher when compared to fenofibrate.
– Combinations of statin + gemfibrozil is discouraged.
– Risk of myopathy with fenofibrate seems to be small.
– Fibrates should preferably be taken in the morning & statins in the evening to minimize peak dose concentrations & decrease the risk of myopathy. - Statin + bile acid exchange resins
- Statin + PCSK-9 inhibitors
Others
Bile Acid Sequestrants (Anion exchange resins)
- Effective in lowering LDL-C.
- May increase TG & HDL-C slightly. Its use is discouraged in pt with TG >= 3.4 mmol/L
- GI A/E are often present even at low doses, which limit their practical use. Other medications should be taken 1 hr before &/or 4 hrs after resins.
- Recommended dose:
– Cholestyramine: 4g/day increased by 4g at weekly intervals to 12-24 g/day in 1 – 4 divided doses. Max: 24 g/day.
Nicotinic Acid (Niacin) & its derivatives.
- Decreases mobilization of free fatty acids from adipose tissues –> increases HDL-C & lowers TG levels.
- May be considered as alternative therapy to fibrates in individuals with elevated TG not responsive to non-pharmacological methors.
- Recommended dosages:
– Starting dose: 150 – 300 mg daily in divided doses, titration of dose up to 2g/day (usual dose). Should be taken with meals to reduce GI side effects.
Medication summary
Response to therapy
Lipid profile should be measured at 1 – 3 months following initiation & following a change in the dose of statin therapy.
- If LDL-C targets achieved: Maintain same dose of statin. Lipid profile can be repeated at 6 – 12 month intervals.
- If LDL-C target not achieved: Titrate dose of statin up to maximal tolerated dose. If still not achieved, a non-statin drug can be added.
Management of elevated TG
At present, fasting TG > 1.7 mmol/L continue to be considered a marker of increased risk, but concentration <= 1.7 mmol/L are not evidence-based target levels for therapy.
Targets of therapy
- Primary target: Still remains achieving LDL-C goal depending upon the individual’s global risk.
- In individuals where:
– TG 2.3 – 4.5 mmol/L the secondary target of therapy is non-HDL-C.
– TG > 4.5 mmol, the primary target of therapy is non-HDL-C
(However, for patient with TG > 4.5 mmol/L, they should a repeat lipid panel tested in the fasting state first)
Management
Mild-to-moderate elevations (> 1.7 – < 10.0 mmol/L)
- Lifestyle changes.
- Drug therapy should be considered in high risk individuals. 2 options:
– Intensifying statin therapy, especially if LDL-C target is not achieved. More potent statins (atorvastatin, rosuvastatin, & pitavastatin) demonstrate a robust lowering of TG levels, especially at high doses.
– Statin + fibrates (avoid gemfibrozil)
Severe elevations (> 10 mmol/L)
- In asymptomatic individuals:
– Repeat fasting TG (after an interval of 5 days, but within 2 weeks)
– Review for potential secondary causes & seek specialist advice if TG concentration remains above 10 mmol/L - Treatment
– Drug of choice: statins
– Can consider Fish oil, doses of 3 – 4 g/day can lower TG by 20 – 50%
– In those who have suspected pancreatitis, treatment include fibrate or nicotinic acid - Severe hyperTG associated with uncontrolled DM warrants initiation of IV insulin infusion.
– IV insulin stimulates intravascular lipoprotein lipase that helps to clear TG at a faster rate. The TG level will improve within 2 – 5 days, but may not normalize.
Management of dyslipidemia in specific conditions
Diabetes mellitus
- In T1DM, high TG is common. HDL-C levels are often normal & even high unless glycaemic control is poor or nephropathy is present.
- In T2DM, high TG concentration, reduced HDL-C & increased level of small dense LDL particles is the usual pattern.
- Screening:
– In adult patients with DM, a lipid profile should be measured at least annually & more often if needed to achieve goals. - All pt with DM > 40 y/o should be treated with a statin regardless of baseline LDL-C levels.
- In T2DM pt < 21 y/o and without clinical CVD, statin is generally not recommended.
- The target LDL-C levels will depend upon their CV risk.
- In pt who have achieved LDL-C targets, the following are secondary targets of therapy:
– Non-HDL-C < 3.4 mmol/L (when TG > 4.5 mmol/L)
– HDL-C > 1.0 mmol/L for males, > 1.2 mmol/L for females
– TG < 1.7 mmol/L
Renal disease
- Main lipid abnormality:
– In CKD: elevated TG, low HDL-C. TC is usually normal or low.
– In nephrotic syndrome: both TC & LDL-C are elevated (usually improve/resolve after treatment. If persists, consider drug therapy) - Initiating dose of statin or fibrates should be lower in CKD patient (eGFR < 60) as the risk of muscle related Sx is higher.
– Combination with fibrates should be avoided. - Statins or ezetimibe/simvastatin combination should be initiated in CKD patients (Stages 3 – 5) for primary & secondary prevention of CKD.
- Pt with CKD stages 1 – 2 should be assessed using the FRS-General CVD Risk score.
- Target LDL-C will depend on their CV risk.
- Statins should not be commenced for primary prevention of CVD in patients on dialysis.
- In patients with established CVD already on statins or an ezetimibe/statin combination at the time of initiation of dialysis, these drugs should be continued.