Chronic Obstructive Pulmonary Disorder (COPD)
Definition (GOLD 2023 guideline)
- Heterogenous lung condition characterized by chronic respiratory symptoms (dyspnea, cough, sputum production &/or exacerbations)
- Due to abnormalities of the airways (bronchitis/bronchiolitis) &/or alveoli (emphysema)
- Causing persistent, often progressive airflow obstruction.
Pathophysiology

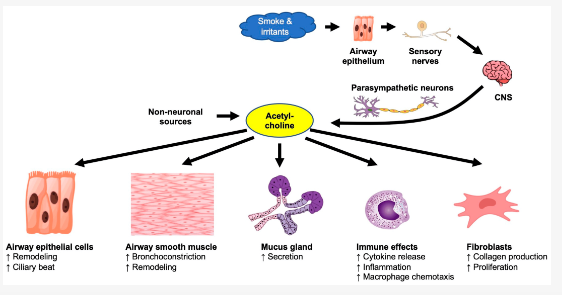
As seen above, acetylcholine plays a role in the pathophysiology in COPD and thus often time in the management of COPD we see the usage of SAMA or LAMA but not so in asthma management.
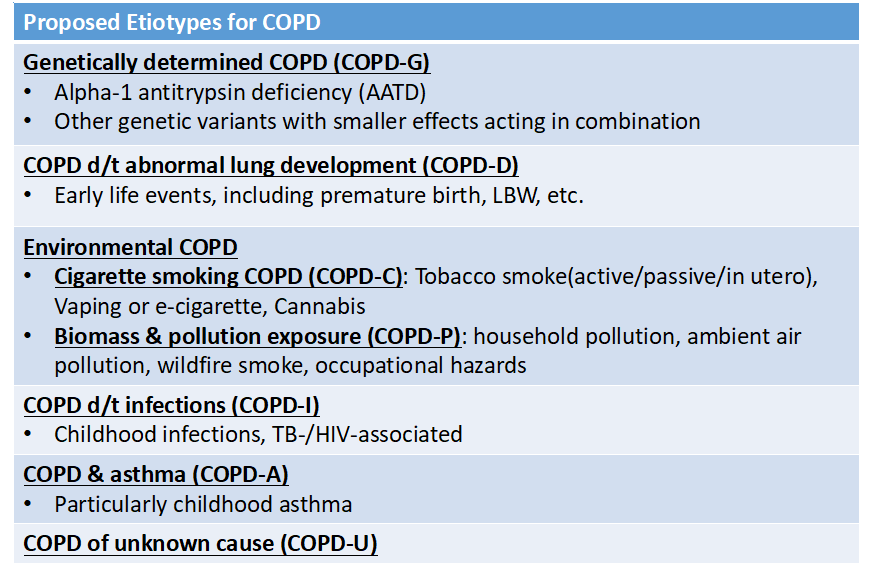
Risk factors
- Genes (severe alpha-1 antitrypsin enzyme deficiency –> panlobular emphysema)
- Exposure to particles
– Tobacco smoke (dose-related)
– Organic & inorganic occupational dusts
– Indoor air pollution from heating & cooking with biomass in poorly ventilated dwellings.
– Outdoor air pollution (air pollution from motor vehicle emissions is a/w decrease in lung function) - Lung growth & development
- Oxidative stress
- Respiratory infections (vicious cycle hypothesis)
- Socioeconomic status (inversely related)
The risk factors above are mentioned in our Malaysia CPG guidelines and it can be seen similarly as the proposed etiotypes for COPD in the GOLD 2023 guidelines
Clinical features
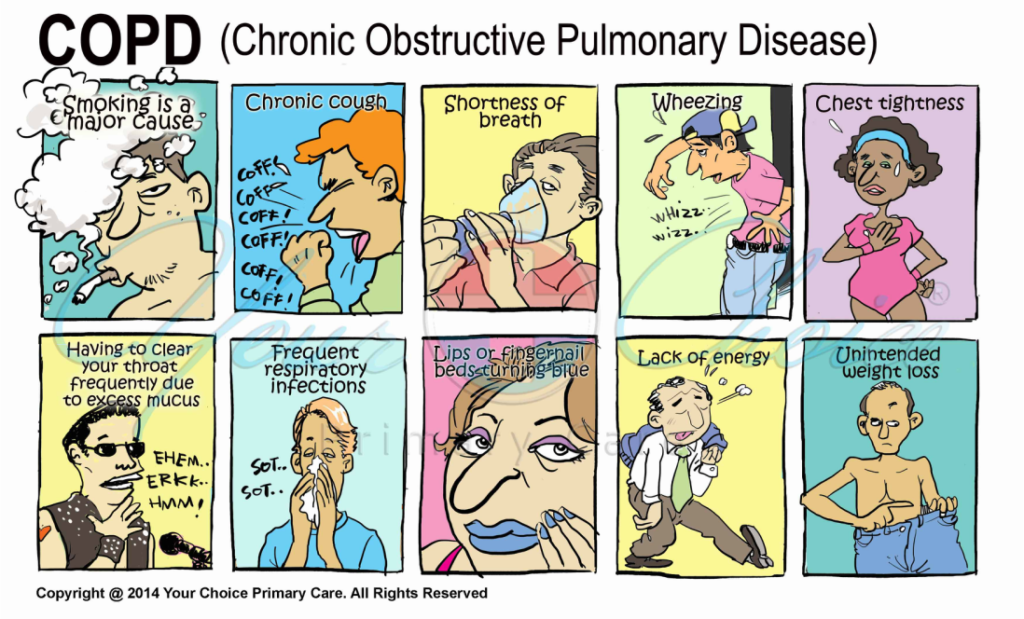
- Cough (often 1st symptoms) – may initially be intermittent but later present daily, often with sputum production.
- Dyspnoea (hallmark) – progressive & is persistent.
- +- wheezing & chest tightness
- Complications: malnourishment, cor pulmonale
Clinical indicators (GOLD 2023 guidelines)
- Dyspnea: progressive over time, worse with exercise, persistent
- Recurrent wheeze
- Chronic cough: may be intermittent & may be unproductive
- Recurrent LRTIs
- Presence of risk factors (tobacco smoke, occupational dust, genetic factors etc.)
Diagnosis
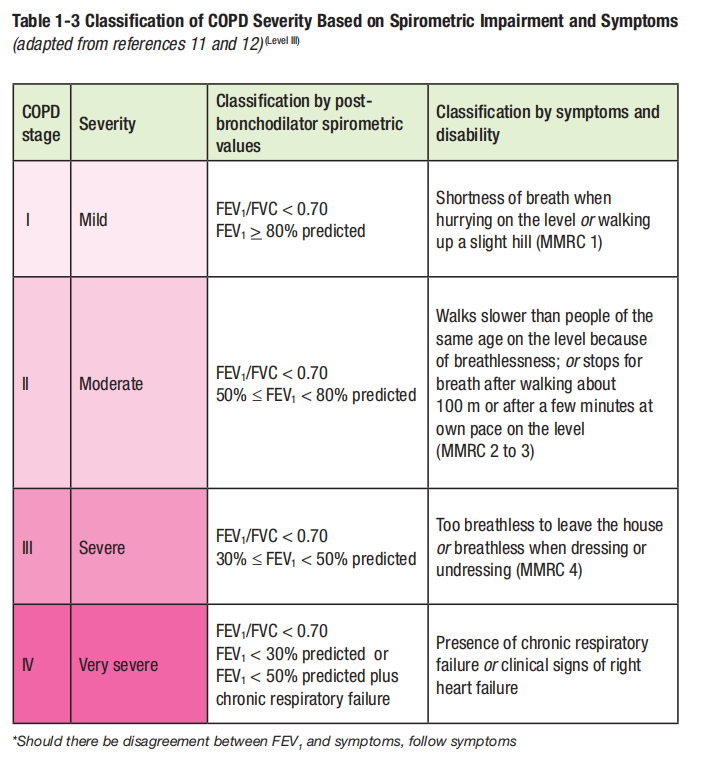
Diagnosis should be confirmed by spirometry showing a post-bronchodilator FEV1/FVC ratio of < 0.7
– Spirometry should be performed after an adequate dose of inhaled bronchodilator (e.g. 400 ug of salbutamol) in order to minimize variability.
– Peak flow measurements can detect airflow limitation but has poor specificity & correlates poorly with FEV1.
Severity assessment
Based on spirometric abnormality, pt’s symptoms (MMRC dyspnoea scale), exercise capacity & presence of co-morbidities & complications.
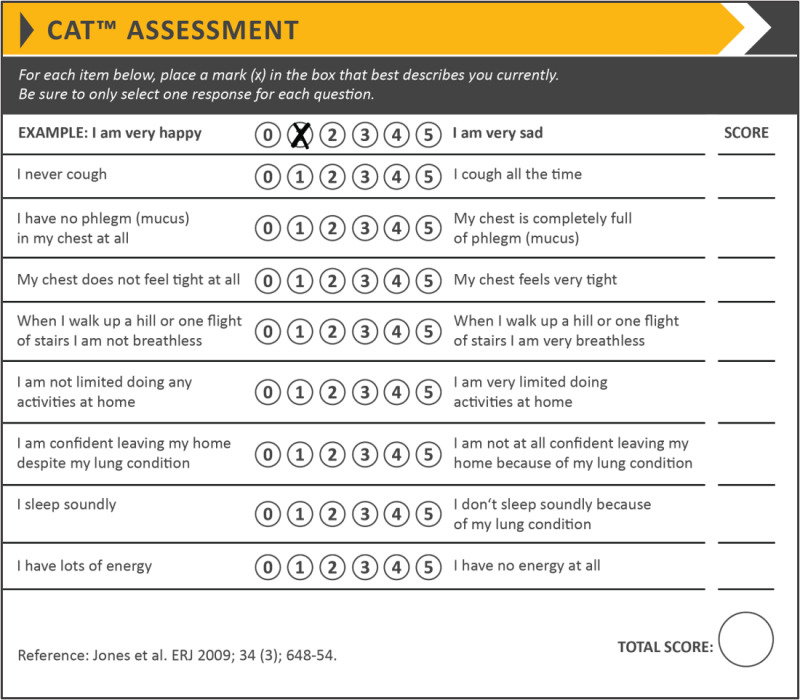
Various other instruments can be used for severity assessment:
– COPD Assessment Test (CAT): multidimensional questionnaire
– BODE Index (used to predict mortality, not for guiding treatment)
Investigations to consider at primary care
- CXR: Hyperinflation (flattened diaphragm & increased lung volume), bullae & hyperlucency of the lungs.
- FBC: anemia of chronic diseases/polycythemia/infection
- ECG: detecting pulmonary HTN (advanced disease) & concurrent IHD.
- Others: FBS, serum albumin, serum fasting lipids (co-morbidities)
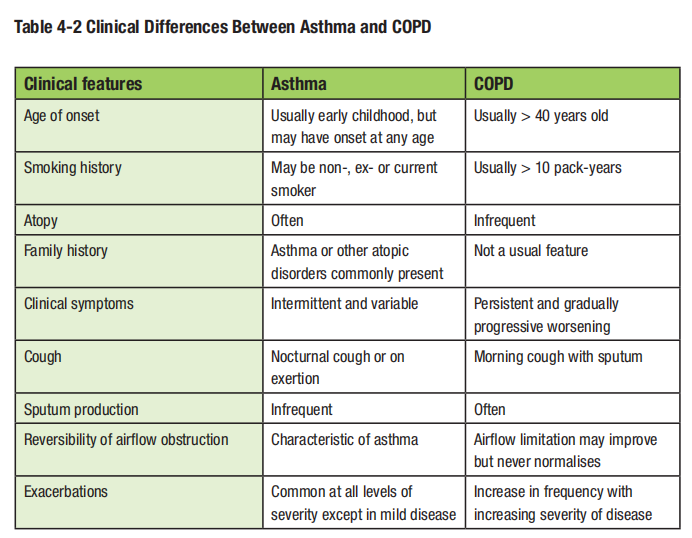
Differential diagnosis
- Bronchial asthma
- CCF
- PTB
- Bronchiectasis
- Diffuse parenchymal lung disease
- Pulmonary vascular disease
Management of stable COPD (CPG guidelines)
Pharmacological therapy: Bronchodilators remain the mainstay
Mild COPD: SABA/SAMA or combination of both may be prescribed.
Moderate to very severe COPD:
– Either LABA or LAMA, or combination of both.
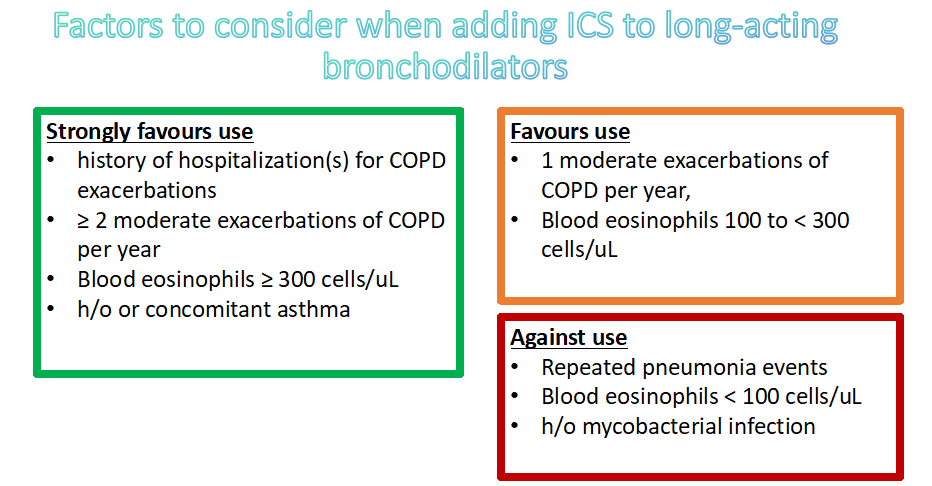
– If symptoms persist, then consider ICS/LABA+LAMA (However, according to GOLD 2023 guidelines, ICS is only added if certain indications are present – will be explained further below)
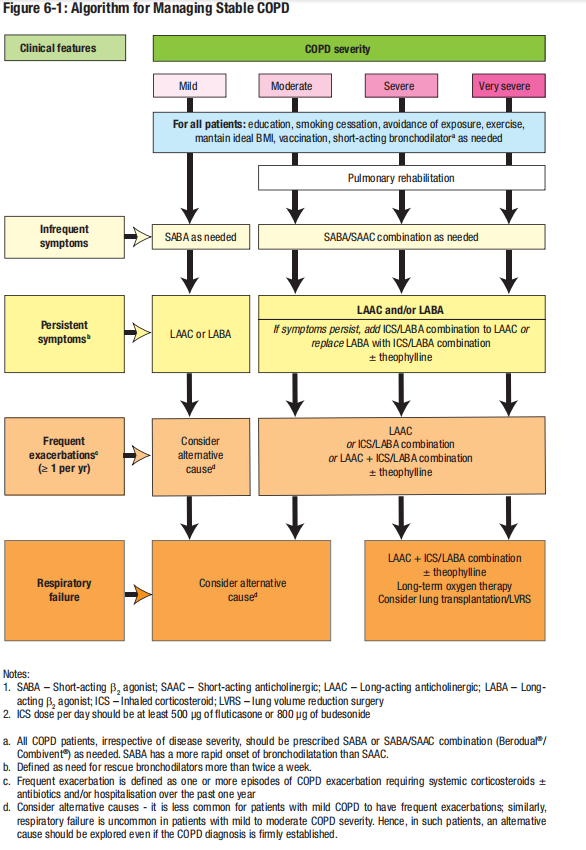
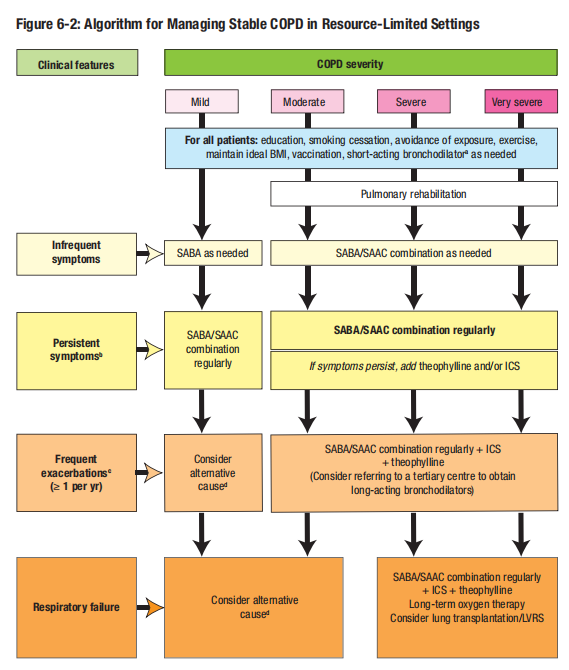
In places where LABA/LAMA may not be available, may consider to start SABA/SAAC combination regularly in moderate to severe COPD.
GOLD 2023 guidelines for stable COPD management
Patients are categorized into Group A, B or E based on severity assessment (mMRC, CAT) and history of moderate exacerbations and hospitalization.
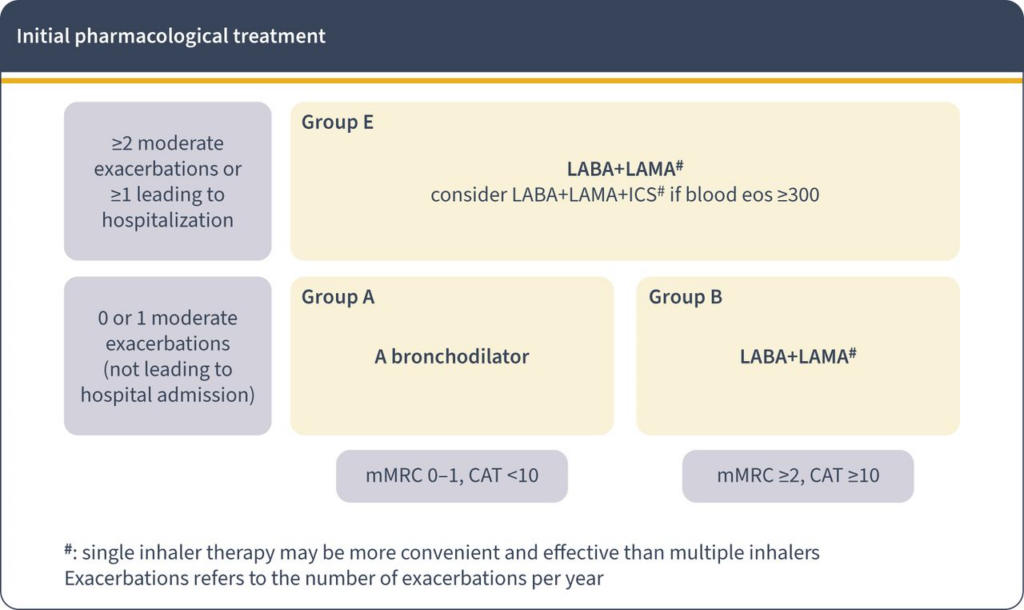
Use of LABA + ICS is not encouraged.
If there is an indication for ICS then LABA + LAMA + ICS has been shown to be superior to LABA + ICS and is therefore the preferred choice.
Non-pharmacological management
a) Recommended vaccination
– Influenza vaccination
– Pneumococcal vaccination: For all COPD patients at least once in their lifetime & have it repeated at least after 5 years (with a max of 2 doses in one’s lifetime)
– Other vaccine as recommended by CDC: COVID-19, dTaP vaccine (to protect against pertussis [Whooping cough] if not vaccinated before), Zoster vaccine (to protect against Shingles for COPD pt > 50 y/o)
b) Pulmonary rehabilitation – improves dyspnoea, health status & exercise tolerance
c) Nutrition – prevent cachexia/overweight
– Goal is to maintain a reasonable bodyweight & BMI (22 – 27 kg/m2) and serum albumin > 35 g/L.
– Excessive weight gain should be avoided.
d) Others (usually under hospital settings) – long term oxygen therapy, lung volume reduction (e.g. bullectomy), lung transplantation
When to refer for a stable COPD patient?
- When the diagnosis is in doubt.
- For spirometry testing when such a facility is not available on site.
- Onset of cor pulmonale.
- Assessment & prescribing of LTOT.
- When there is a rapid decline of FEV1 indicating severity of the disease.
- Pt aged < 40 y/o in whom an underlying genetic predisposition e.g. alpha-1 antitrypsin deficiency is suspected.
- When access to certain drugs/medication is a problem.
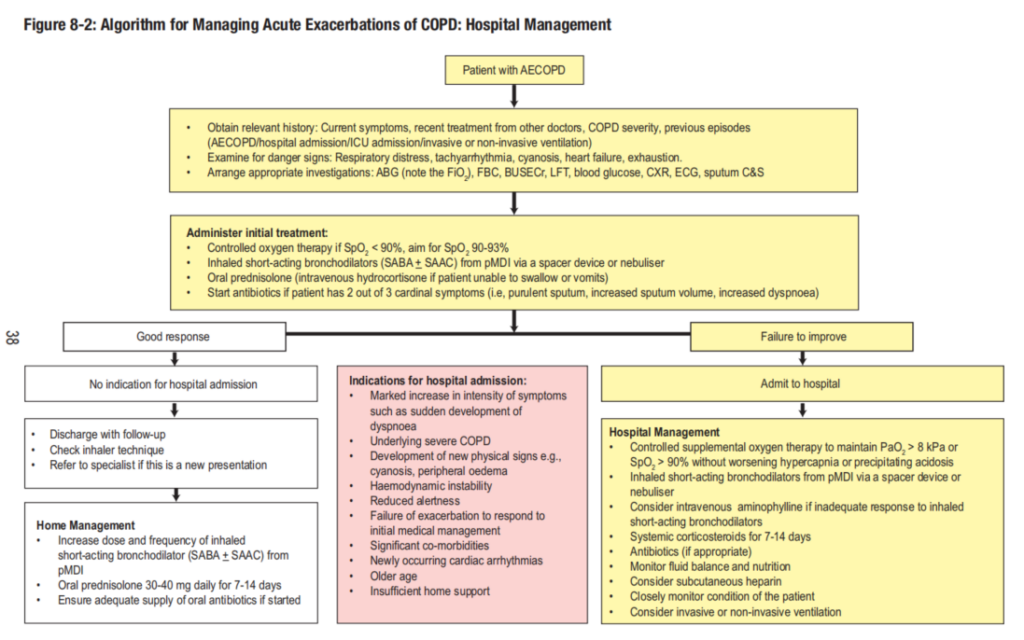
Management of acute exacerbation of COPD
Definition of acute exacerbation (GOLD 2023 guidelines)
Event characterized by increased dyspnoea &/or cough & sputum that worsens in < 14 days which may be accompanied by tachypnea &/or tachycardia and is often a/w increased local & systemic inflammation caused by infection, pollution or other insults to the airways.
Management
- Bronchodilator
– Neb salbutamol. Alternatively: MDI salbutamol (10 – 20 puffs via a spacer) has equal efficacy
– In severe exacerbations:
* Neb SABA + SAMA e.g Combivent 2.5 mL (ipratropium bromide 500 ug, salbutamol 2.5 mg) 6 hourly OR Duovent 4 mL (ipratropium bromide 500 ug, fenoterol 1.25 mg) 6 hourly.
* Can consider adding IV methylxanthines if not responding to neb (hospital settings) - Systemic steroids
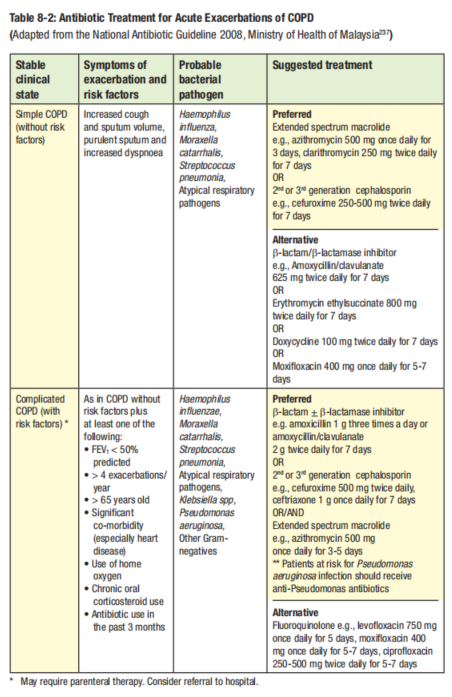
– Oral prednisolone 30 – 40 mg OD for 7 – 14 days - Antibiotics
– Indications:
* At least 2 out of 3 cardinal symptoms: purulent sputum, increased sputum volume &/or increased dyspnoea
* Patient that requires invasive/non-invasive ventilation (hospital settings)
Algorithm for managing acute exacerbation
Follow up visit
- Exposure to risk factors, esp. tobacco smoke & their willingness to stop.
- Any new/worsening symptoms.
- Any complications e.g. respiratory failure/cor pulmonale
- Body weight & BMI – provide information on the nutritional status of the pt.
- Spirometry measurement if symptoms worsen.
- Pharmacotherapy & other medical treatment: effectiveness, side effects, compliance, inhaler techniques.
- Exacerbation history
- Any hospitalization, including duration of stay & any use of invasive/non-invasive ventilation
- Pt education
