Chronic Kidney Disease (CKD)
Chronic Kidney Disease
Definition
eGFR < 60 mL/min/1.73 m2 that is present for more than 3 months ± evidence of kidney damage
OR
Evidence of kidney damage for more than 3 months ± eGFR < 60 mL/min/1.73 m2
Markers of Kidney Damage
- Albuminuria
- Urine sediment abnormalities
- Electrolyte and other abnormalities due to tubular disorders
- Abnormalities detected by histology
- Structural abnormalities detected by imaging
- History of kidney transplantation
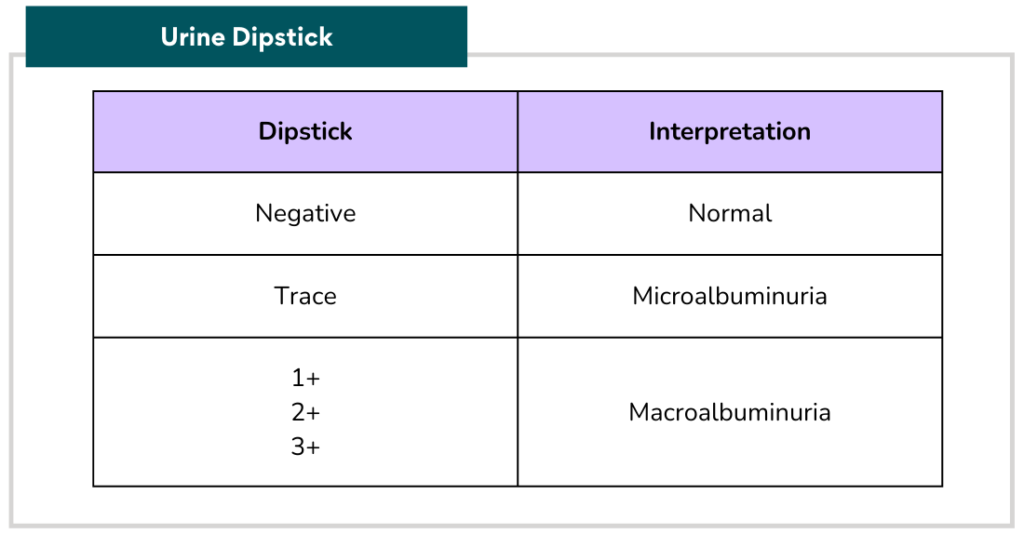
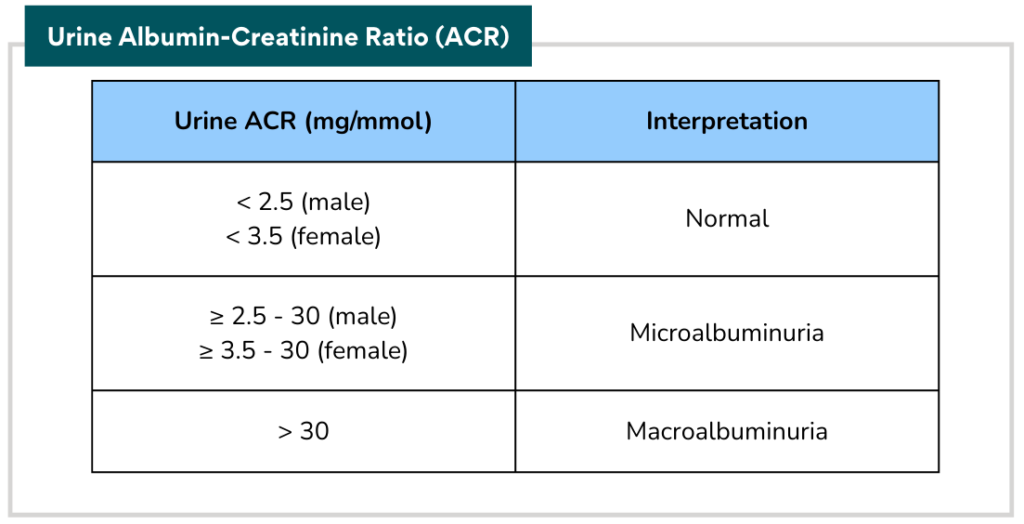
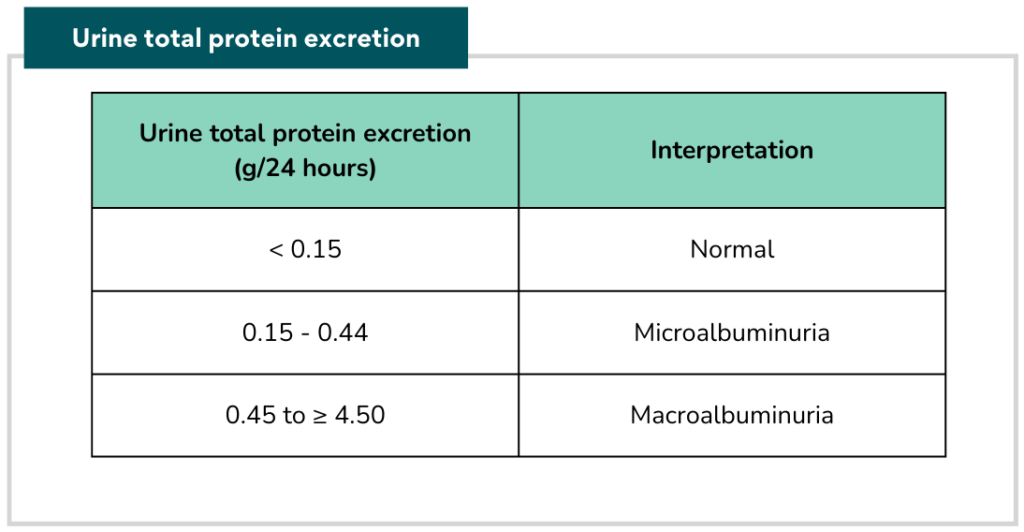
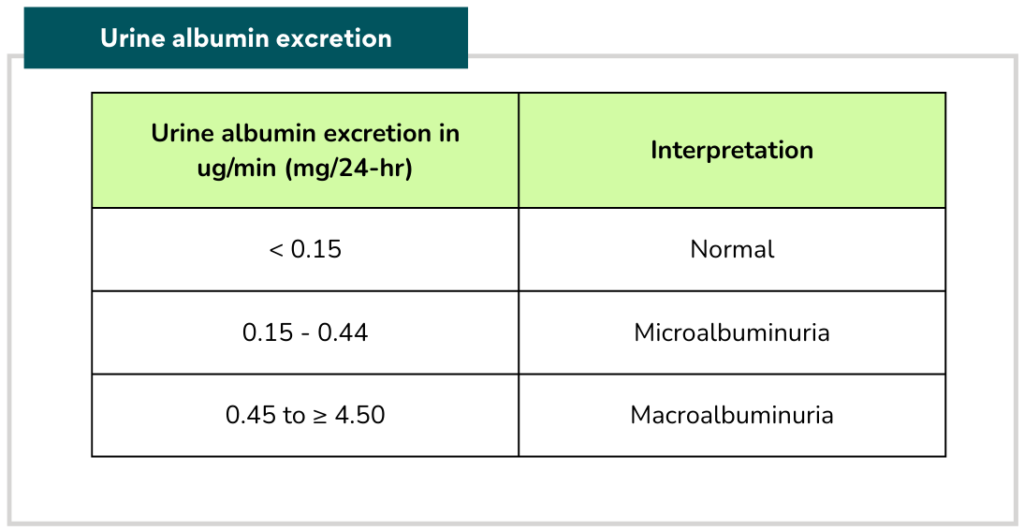
Diagnosis of proteinuria
Proteinuria can be detected by: Urine dipstick, Urine Albumin-Creatinine Ratio (ACR), Urine Protein-Creatinine Ratio (PCR), Urine total protein excretion and Urine albumin excretion.
Source: Ministry of Health Malaysia. Management of Chronic Kidney Disease in Adults. Putrajaya: MoH; 2011
Who to screen for CKD?
- Age > 65 years old
- Obesity CV disease
- Metabolic syndrome (pt with DM &/or HTN should be screened at least yearly)
- Drugs e.g. nephrotoxic drugs, long-term use of PPI or analgesics (e.g. NSAIDs, COX-2 inhibitors)
- Family h/o CKD or hereditary disease
- Gout
- Multisystem diseases with potential kidney involvement e.g. SLE
- Structural renal disease, renal calculi or prostatic hypertrophy
- Incidental detection of hematuria or proteinuria
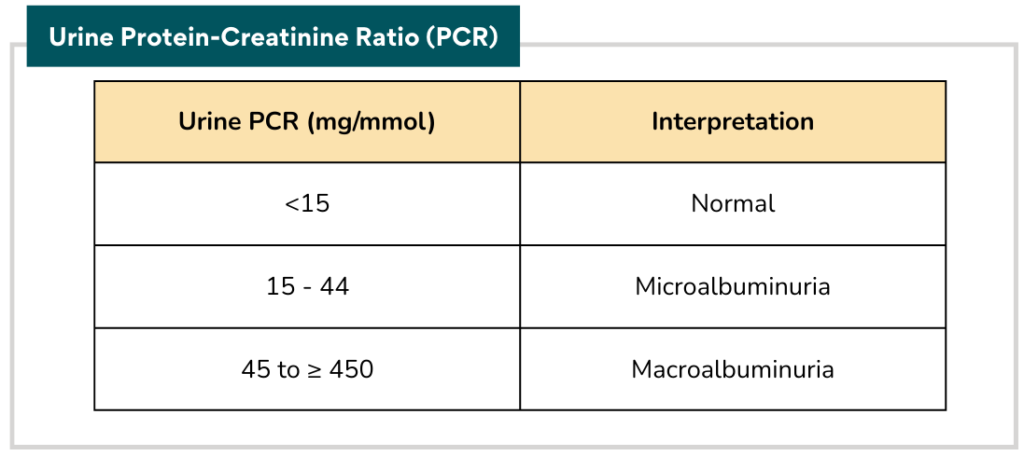
Screening algorithm
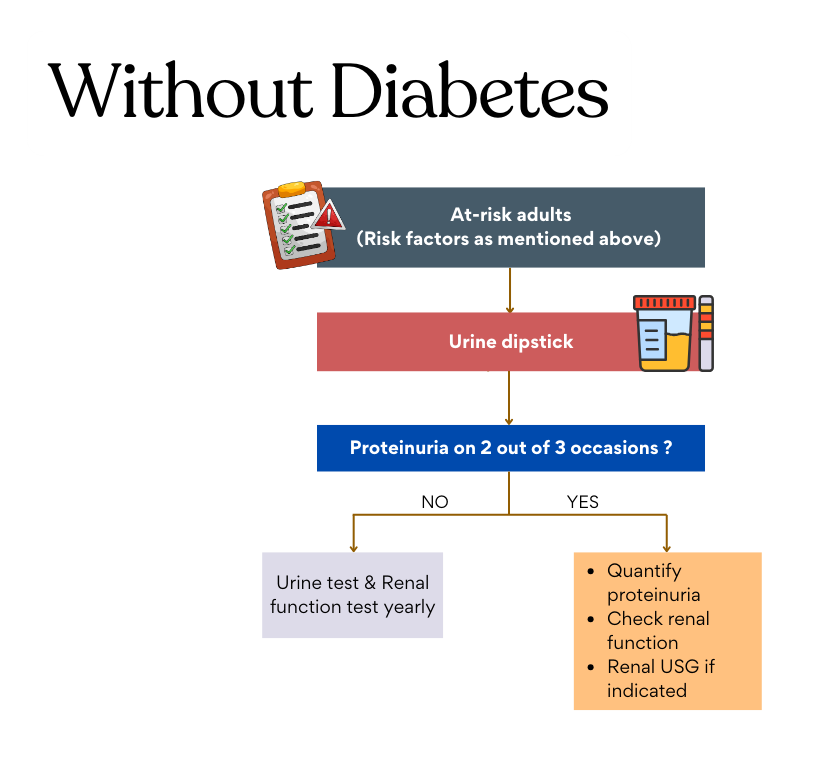
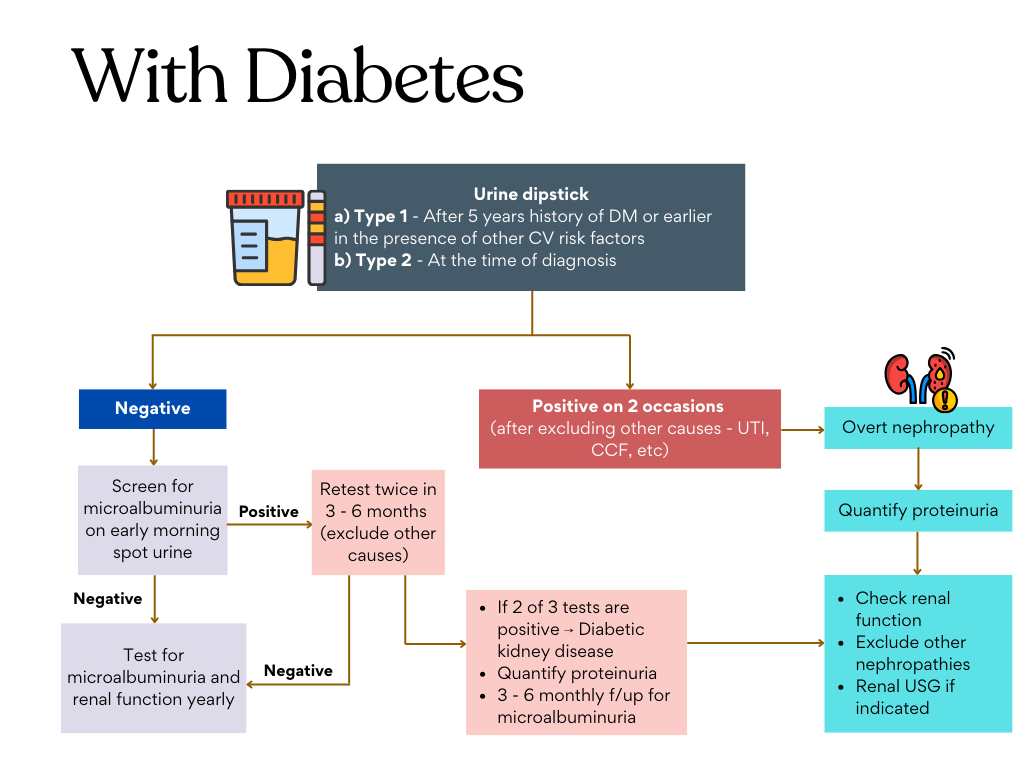
Source: Ministry of Health Malaysia. Management of Chronic Kidney Disease in Adults. Putrajaya: MoH; 2011
Approach to haematuria
Evaluation of hematuria in CKD in adults
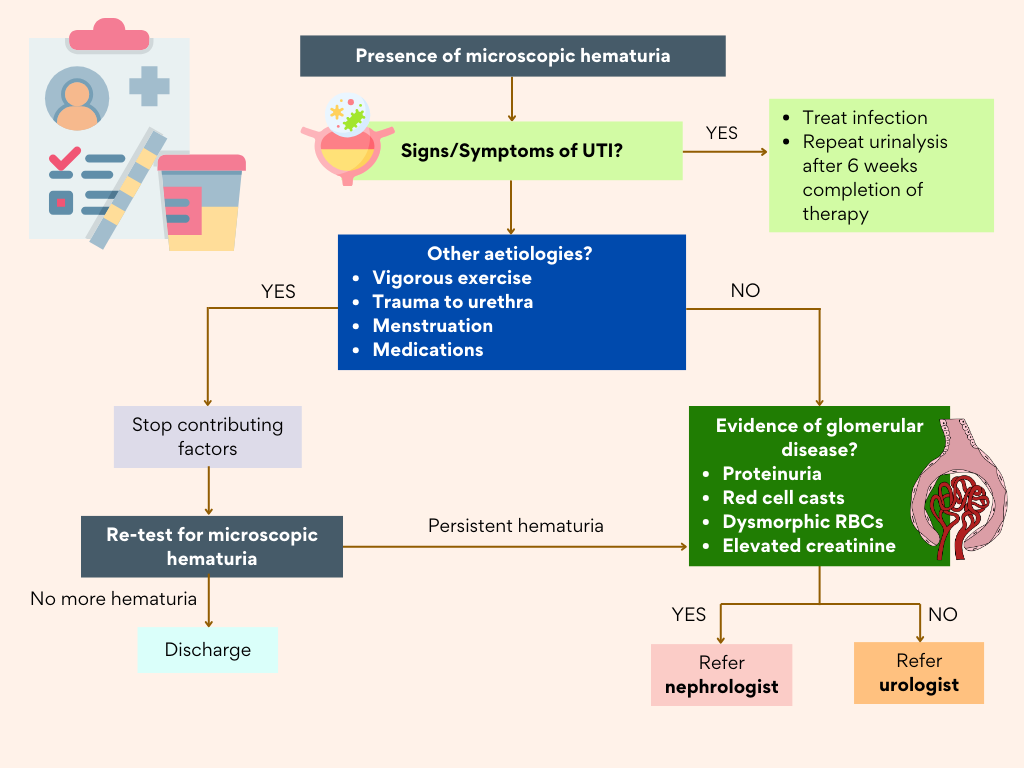
- A positive dipstick test for blood on 2 out of 3 occasions warrant a full microscopic examination.
- Urine microscopy can be used to differentiate hematuria of glomerular or non-glomerular origin.
- Some common causes of persistent microscopic hematuria: infection, glomerulonephritis, renal calculi, malignancy & other forms of kidney damage
Prognosis of CKD (Depends on 4 factors)
- Cause of CKD
- GFR category
- Albuminuria category
- Other risk factors and co-morbid conditions
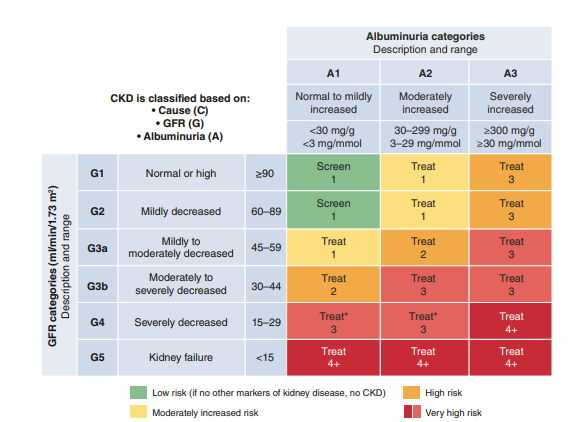
Risk stratification using KDIGO heatmap to guide treatment and follow up.
Clinicians should initiate appropriate management for patients at risk of CKD progression (e.g. BP, DM, dyslipidemia, proteinuria, etc)
The numbers 1, 2, 3 and 4+ suggest the frequency of monitoring (no. of times per year)
Managing CKD
The aim of CKD treatment is to delay its progression, reduce CV risk and manage CKD-related complications
General measures like lifestyle modification, optimizing other co-morbidities should be incorporated for all patients.
Algorithm on Treatment for CKD in adults
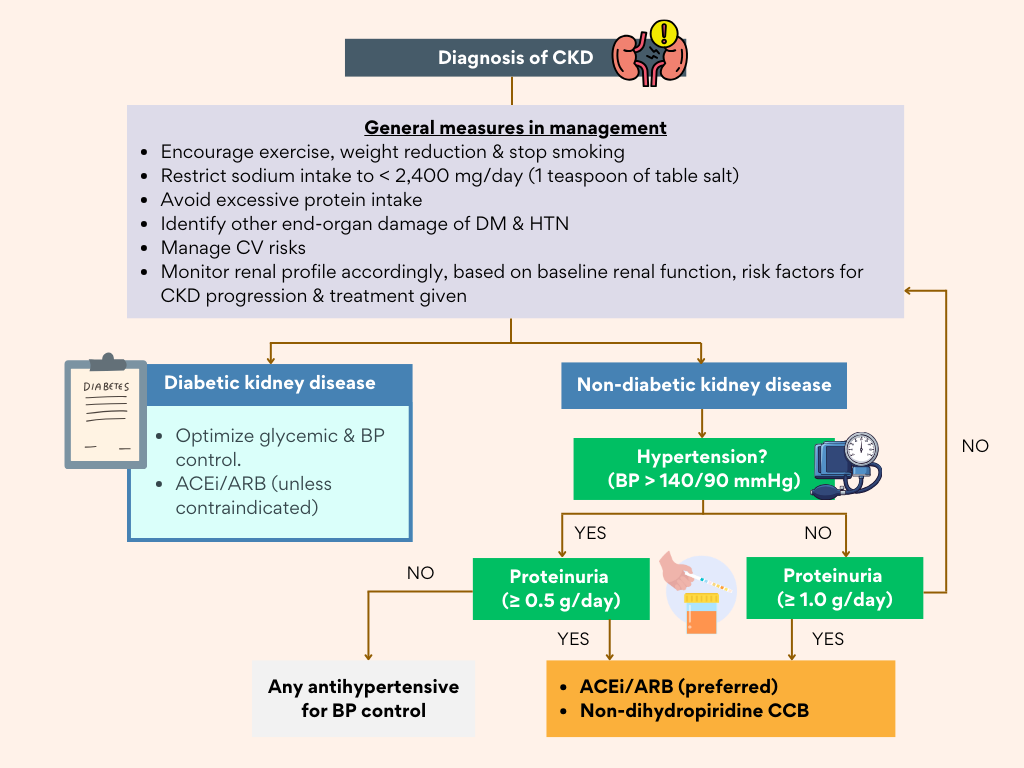
Source: Ministry of Health Malaysia. Management of Chronic Kidney Disease in Adults. Putrajaya: MoH; 2011
Clickable clinical decision tool based on the algorithm above:
CKD Treatment Pathway
This algorithm is adapted from our Malaysia CPG guidelines on management of CKD. It is has been well known that ACEi/ARB have a major role in the management of CKD and this is evident also from the recommendations by KDIGO 2024.
KDIGO 2024
Start ACEi or ARB if :
With diabetes: Moderately (A2) and Severely (A3) increased albuminuria –> Recommended
Without diabetes:
- Severely increased albuminuria (A3) –> Recommended
- Moderately increased albuminuria (A2) –> Suggest to start
(Applies to CKD stages G1 – G4)
Key takeaway: CKD (G1 – G4) + Albuminuria (A2 or A3) -> Start ACEi or ARB (regardless of diabetes status)
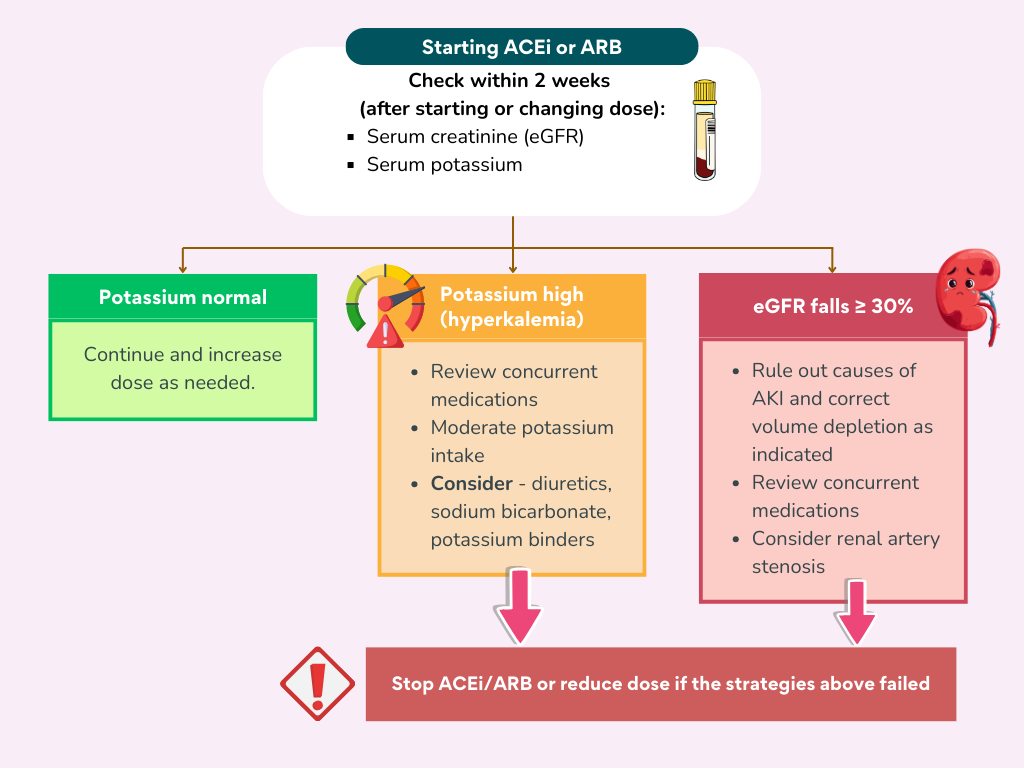
Once ACEi or ARB is initiated, the renal function should be repeated within 2 weeks, to look for any hyperkalemia, significant raised in creatinine and/or decrease if eGFR
Sodium-Glucose Transport 2 (SGLT2) Inhibitors
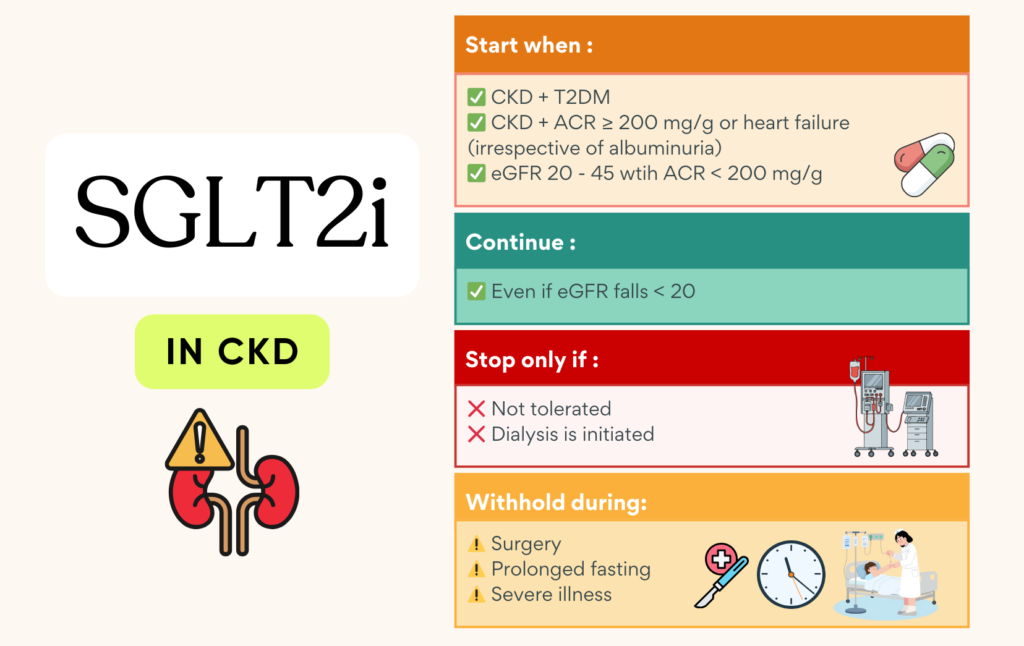
Though it has not been included as part of the algorithm in our Malaysia CPG guidelines yet (but was briefly mentioned in one of the section), I believe it will soon be incorporated in more detail in the coming edition.
SGLT2i has been strongly recommended in the KDIGO 2024 guidelines for its role in the management of CKD.
What else? (KDIGO 2024)
1. Nonsteroidal Mineralocorticoid Receptor Antagonist (MRA) – Finerenone
- Appropriate for adults with T2DM who are at high risk of CKD progression & CV events (persistent albuminuria despite treatment).
- May be added to RASi & SGLT2i for treatment of T2DM & CKD in adults.
- Select people with normal serum potassium concentration & monitor serum potassium regularly (risk of hyperkalemia).
2. GLP-1RA
- In patient with T2DM and CKD who have not achieved individualized target despite use of metformin and SGLT2i, or who are unable to tolerate those medication.
Holistic approach (KDIGO 2024 guidelines)
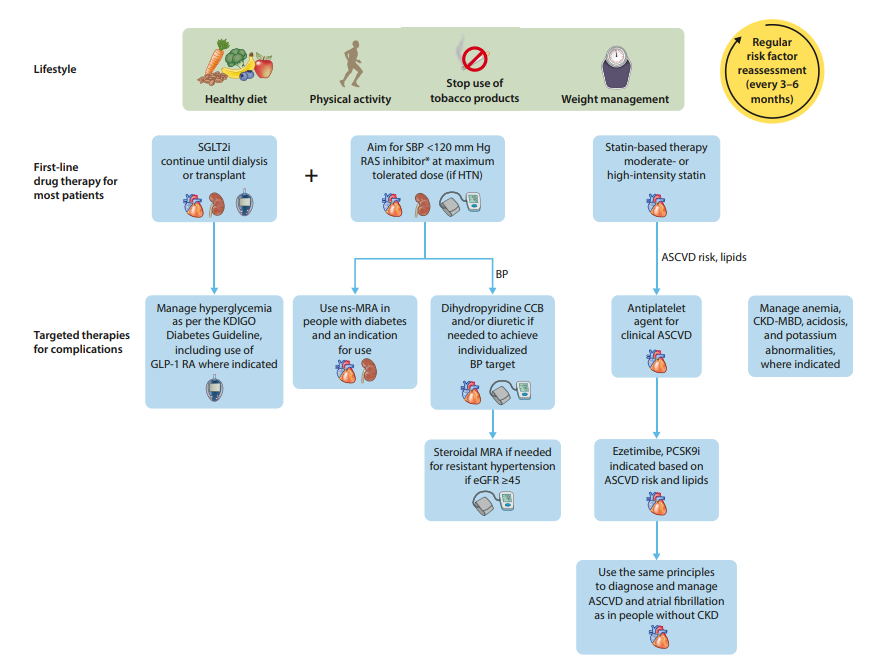
🎯Target BP control
Malaysia CPG
- Diabetic kidney disease [DKD] (regardless of proteinuria): ≤ 130/80 mmHg (SBP 120 – 130)
- Non-DKD with heavy proteinuria (≥ 1g/day): ≤ 130/80 mmHg (SBP 120 – 130)
- Non-DKD with proteinuria < 1g/day: ≤ 140/90 mmHg (SBP 120 – 140)
KDIGO 2024
- Suggest target SBP < 120 mmHg.
- Less intensive BP lowering therapy in people with frailty, high risk of falls & fractures, very limited life expectancy or symptomatic postural hypotension.
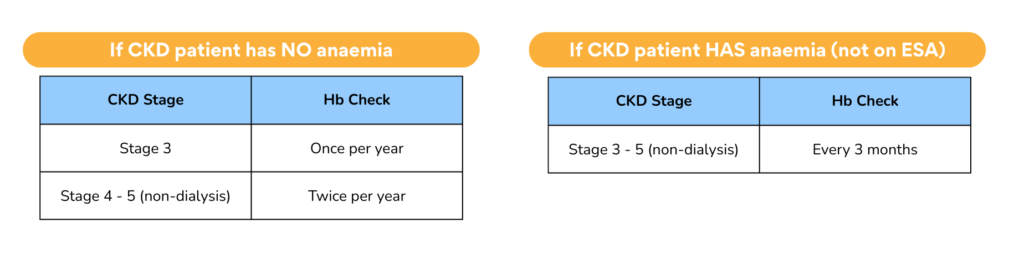
Screening for complications
1. Anemia (usually occurs when eGFR <60)
- Screening for anemia should be done when eGFR < 60.
- When the eGFR is >= 60 the anemia is likely to be due to other causes.
- Other causes of anemia should be excluded during the work-up for renal anemia
- Treatment with ESA must be commenced by or in consultation with a nephrologist
- Optimal Hb target: 10 – 12 g/dL, but should also be individualized based on symptoms and co-morbidities
Hb Monitoring
2. CKD-Mineral and Bone Disorder (CKD-MBD)
- Changes in the metabolism of calcium, phosphate, PTH and ALP typically start to occur when eGFR < 60.
- Screening for CKD-MBD should be done when eGFR < 45.
- Elevated phosphate level should be lowered towards the normal range & hypercalcaemia should be avoided in most stages of CKD.
- In hyperphosphataemia, dietary restriction of phosphate is recommended.
- If persistent, dietary compliance should be re-assessed before considering the use of phosphate binders.
- Excess calcium administration & vitamin D analogue should be avoided as there may be increased risk of vascular calcification in CKD.
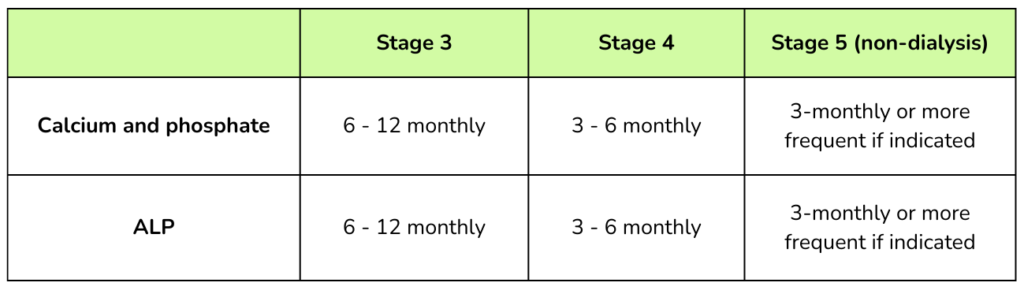
Monitoring
Indication for referral 📝
- Persistent heavy proteinuria [urine protein ≥ 1g/day or urine protein : creatinine ratio (uPCR) ≥ 100 mg/mmol] despite optimal treatment.
- Persistent isolated microscopic hematuria after excluding urogynae cause.
- Persistent hematuria + proteinuria (urine protein ≥ 0.5g/day or uPCR ≥ 50 mg/mmol)
- Rapidly declining renal function (loss of eGFR > 5 ml/min/1.73 m2 in 1 year or > 10 ml/min/1.73 m2 within 5 years)
- eGFR < 30 ml/min/1.73 m2
- Resistant hypertension
- Suspected renal artery stenosis
- Suspected hereditary kidney disease
- Pregnant or when pregnancy is planned
- Persistent abnormalities of serum potassium
- Unexplained cause of CKD
References
- Ministry of Health Malaysia. (2024). Clinical practice guidelines: Management of chronic kidney disease in adults. Putrajaya: Ministry of Health Malaysia.
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group (2024). KDIGO 2024 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney international, 105(4S), S117–S314. https://doi.org/10.1016/j.kint.2023.10.018
