Acne Vulgaris
Pathogenesis
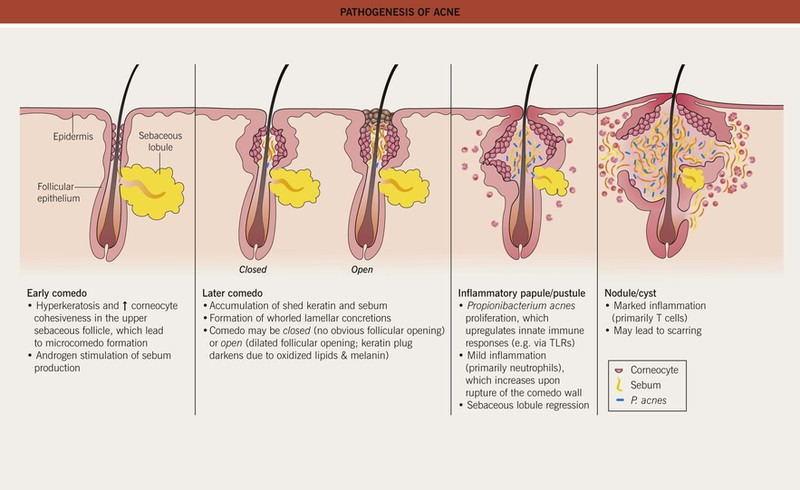
Involves 4 key pathogenic factors
1. Increased sebum production
2. Altered follicular keratinisation leading to comedones formation
3. Follicular colonization by Cutibacterium acnes (C. acnes), previously known as Propionibacterium acnes
4. Inflammation around pilosebaceous unit
Clinical presentation
Non-inflammatory lesion (NIL): open (blackheads) & closed (whiteheads) comedones
Inflammatory lesion (IL) : papules, pustules, nodules & cysts
Comedone

Inflammatory lesions

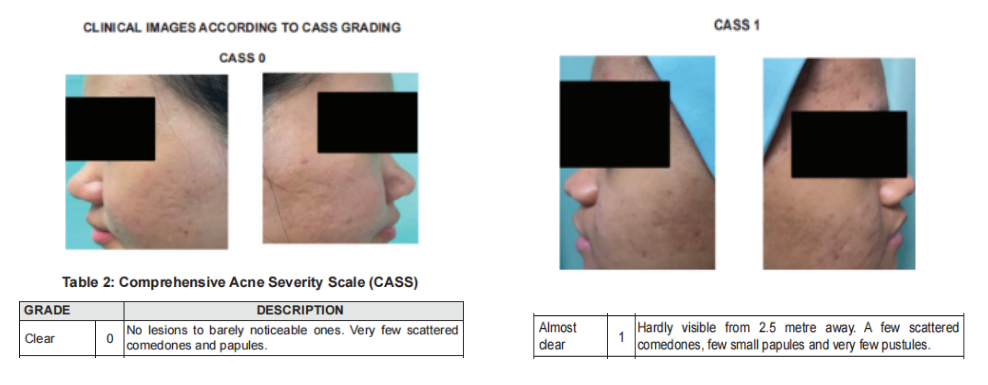
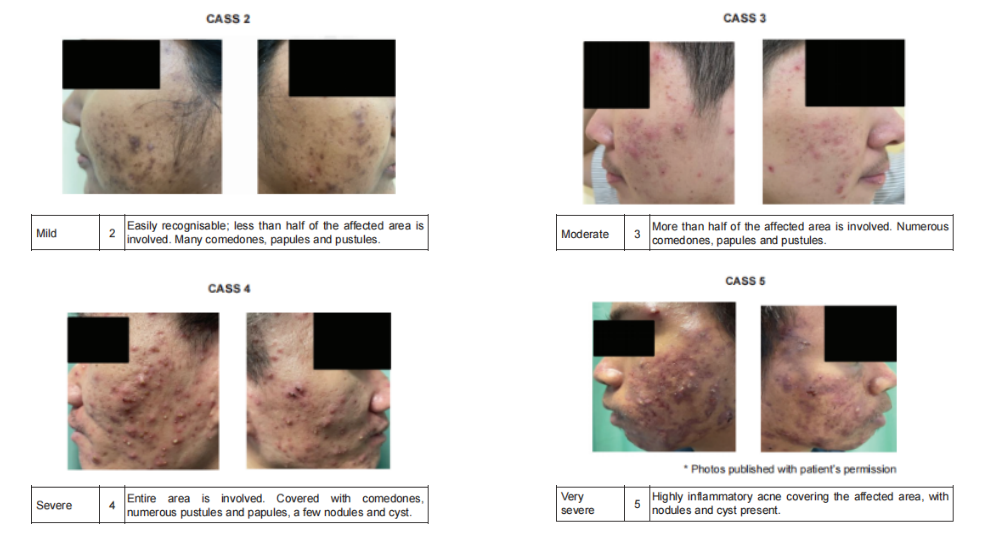
Severity assessment
Using the Comprehensive Acne Severity Scale (CASS)
Treatment (topical)
Commonly used:
a) Topical Benzoyl Peroxide (BPO)
b) Topical Retinoids
c) Topical Antibiotics
d) Fixed combination therapy
Topical agents are the mainstay of treatment in mild-moderate acne vulgaris.
The commonly used agents are topical BPO, retinoids, Abx & fixed combination preparations.
Combination treatment with either topical BPO, retinoids or topical Abx is more effective than monotherapy
Topical Benzoyl Peroxide (BPO)
- Available in 2.5%, 5% & 10% concentrations
- Topical BPO monotherapy or in combination with other topical therapy should be given in mild to moderate acne vulgaris.
- Practical advice on topical BPO:
– Start at lower concentration of 2.5% & titrate gradually to 5 – 10% if no improvement.
– Apply once daily on affected areas only. (May increased up to twice daily if needed)
– If skin irritation develops, withhold treatment & restart on alternate days once AE has subsided.
– Concomitant use of moisturizer may improve tolerability.
– Bleaching of clothes may occur & the pt should be advised accordingly.
Topical retinoids (synthetic derivatives of Vitamin A)
- Include tretinoin, adapalene, tazarotene & isotretinoin.
- In Malaysia, only topical tretinoin & adapalene are currently available.
- Topical retinoids (e.g. tretinoin & adapalene) monotherapy should be used in non-inflammatory acne vulgaris or in combination with other therapies in inflammatory acne vulgaris.
- Contraindicated in pregnancy
- Practical advice:
– It can cause photosensitivity, thus should be applied at night.
– Apply a thin layer on the affected areas or the entire face.
– If skin irritation develops, withhold treatment & restart on alternate days once the AE has subsided.
– Concomitant use of moisturiser may improve tolerability.
– Adequate sun protection (e.g. using broad-spectrum sunscreen, umbrella or hat) is advisable.th other topical therapy should be given in mild to moderate acne vulgaris.
Topical Antibiotics
- Useful in treatment of mild-moderate inflammatory acne.
- The use of topical Abx as monotherapy should be avoided to prevent bacterial resistance.
- Topical clindamycin & erythromycin are the most widely prescribed Abx. (Only topical clindamycin is available in Malaysia for the treatment of acne).
Fixed combination therapy
- Available fixed combination therapy:
– Clindamycin/BPO
– Adapalene/BPO
– Erythromycin/BPO
– Clindamycin/Tretinoin
Other topical agents
- Topical Azelaic Acid (anti-microbial & anti-comedonal properties)
– Also inhibits tyrosinase, thus effective for post-inflammatory hyperpigmentation - Topical Salicylic Acid (keratolytic & comedolytic effects)
Treatment (systemic)
- Oral antibiotics
- Oral isotretinoin (prescribed only by dermatologist)
- COCP (may be beneficial in female patient especially those with hyperandrogenism)
- Spironolactone (anti-androgen & aldosterone antagonist) – competes with DHT for androgen receptors in the skin
- Metformin (may be beneficial as adjuvant treatment; enhances insulin sensitivity –> reduce androgenic hormone)
Oral antibiotics
- Indicated for moderate-severe papulopustular/inflammatory acne vulgaris.
- Topical retinoid, BPO or AA should be used after discontinuation of Abx.
- Commonly used:
– Tetracycline group (1st line) – contraindicated in pregnancy, lactation, age < 8 y/o or allergic to tetracyclines.
– To reduce the AE of doxycycline, pt should be advised to take medication after meal with plenty of water; practice adequate sun protection.
– Macrolides (Erythromycin, Azithromycin)- safe to be used in pregnancy & lactation
– Trimethoprim-sulfamethoxazole (Co-trimoxazole) – should only be used when other Abx have failed or are contraindicated because of its potential serious AEs. - Oral abx in combination with other topical treatment e.g. BPO, retinoid & AA is advocated as it prevents development of bacterial resistance, achieves faster resolution of lesions & targets multiple pathogenesis of acne.
- Oral doxycycline, tetracycline or erythromycin should be used for moderated to severe acne vulgaris.
- Response to these Abx should be evaluated at 6 – 8 weeks.
- Target duration therapy should not exceed 3 – 4 months to reduce resistance.
Oral isotretinoin
- Reduces sebaceous glands activity & size markedly, normalises follicular keratinisation, indirectly inhibits C. acnes growth in hair follicle & exerts an anti-inflammatory action.
- Should be prescribed for nodulocystic or severe acne vulgaris & treatment-resistant moderate acne vulgaris.
- Should only be prescribed by dermatologists
- Teratogenic & strict contraceptive practice is required for females who may become pregnant.
Cosmeceuticals
- May be used as an adjunct in the management of acne vulgaris.
- However, stronger evidence is warranted before cosmeceuticals can be recommended.
- Types: cleanser, sonic cleansing device, moisturiser, sunscreen (UVB cause inflammation, increase sebum production & proliferation of keratinocytes), hydrocolloid acne patches
- Active ingredients in Cosmeceutical for Acne Vulgaris:
– Comeolytics – e.g. retinaldehyde, retinol. AHA (e.g. GA), beta-hydroxy acids (e.g. salicylic acid) & polyhydroxy acids (e.g. lactobionic acid & gluconolactone)
– Sebum controller with anti-inflammatory properties – e.g. nicotinamide/niacinamide
– Antibacterial agents – e.g. tyrothricin, tea tree oil, aloe vera, propolis, licochalcone A & cedar
– Antioxidant – e.g. Green tea extract
– Vitamin C (ascorbic acid)
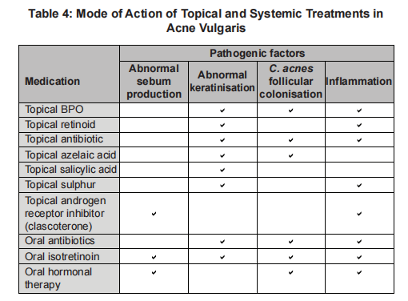
Summary on mode of action of topical and systemic treatment
Management for special groups
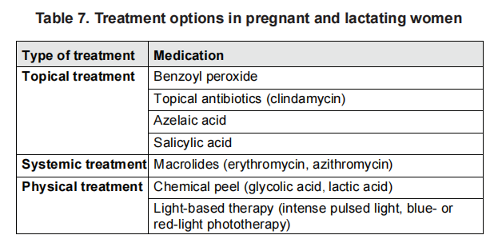
Pregnant and lactating women
Hormonal therapy, tetracyclines, co-trimoxazole & isotretinoin should be avoided.
Adolescent
- Topical BPO & topical retinoids (tretinoin & adapalene) may be used safely in adolescents.
- Oral tetracycline derivatives (e.g. tetracycline, doxycycline, & minocycline) should not be used in patients aged < 8 y/o.
- Oral isotretinon can be used safely in pt >= 12 y/o.
Complications
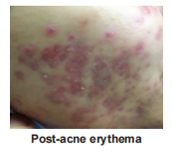
1. Post-acne erythema (PAE)
– Presents as telengiectasia & erythema post-acne treatment.
– May improve over time, but some may remain & cause undesirable aesthetic effect.
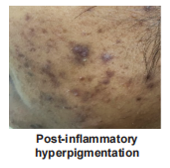
2. Post-inflammatory hyperpigmentation
– Commonest site: cheek
3. Acne scars
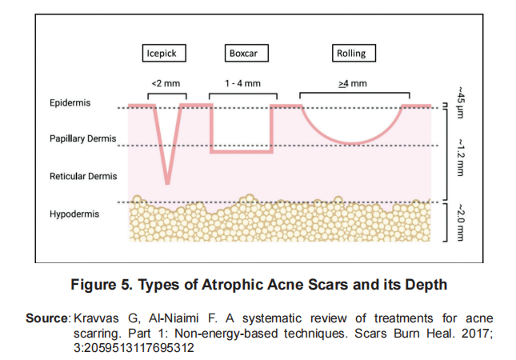
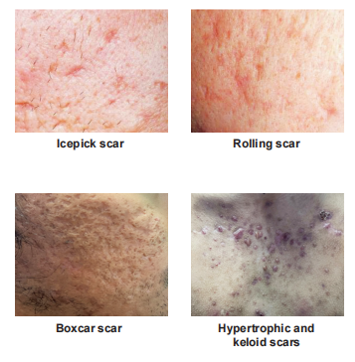
– Can be divided into atrophic, hypertrophic or keloid scars.
– Atrophic scars can be divided into icepick, rolling & boxcar scars.

Referral
Urgent: within 24 hours
- Acne fulminans (rare skin disorder)
– Acute, painful, ulcerating & haemorrhagic form of acne.
+- systemic Sx e.g. fever & polyarthritis
+- bone lesions & laboratory abnormalities. - Urgent referral to PSY if have major depression/exhibiting suicidal behaviour
Seen early: within 2 weeks
- Moderate to severe acne (e.g. nodulocystic acne)
- Severe social or psychological problems including a morbid fear of deformity (dysmorphophobia)
Non-urgent: based on available date
a) Diagnostic uncertainties, e.g.
– Suspected rosacea
– Suspected drug-induced acne
– Suspected occupational causes
– Suspected underlying endocrinological cause (e.g. PCOS) requiring further assessment
– Suspected Staph folliculitis, pityrosporum folliculitis or gram -ve folliculitis
– Rare variants of acne e.g. acne excoriae & chloracne
b) Dermatologist consultation & services.
– Failed oral Abx therapy
– Resistance or intolerance to current treatment
– Scarring or pigmentary changes
– Pregnancy with moderate & severe acne vulgaris
– Indication for specialised physical treatment (e.g. incision, drainage of cysts & laser)
Summary
Mild cases
- Topical bpo – apply in the morning OD, staining of shirt
- Topical retinoid (adapalene) – active lesion with pigmentation, not to be used in pregnancy and lactation, photosensitive – use at night
- Apply moisturizer before/after topical treatment to reduce irritation
- Do not use topical abx as monotherapy
Moderate to severe acne
- Oral abx, review in 6 to 8 weeks, if effective, consider taking for up to 3 to 4 months. Not to be used for more than 4 months. Used with topical bpo and retinoids
- If not responding to systemic abx, refer derm kiv to start isotretinoin.
- Consider start with oral tetracycline group (for more than 8 years above)
- Oral erythromycin can be used for all age group
- Reserved macrolide for pregnant patient
Oral isotretinoin – only prescribed by dermatologist
Algorithm

