Gout
Gout
(A disease caused be monosodium urate (MSU)
crystal deposition)
Image of “The Gout”, by James Gillray. Wikimedia Commons, CC BY
Natural History of Gout
- Asymptomatic hyperuricemia
- Asymptomatic MSU crystal deposition (without gout)
- Recurrent gout flares with intercritical gout
- Gout with chronic gouty arthritis/tophaceous gout/erosive gout
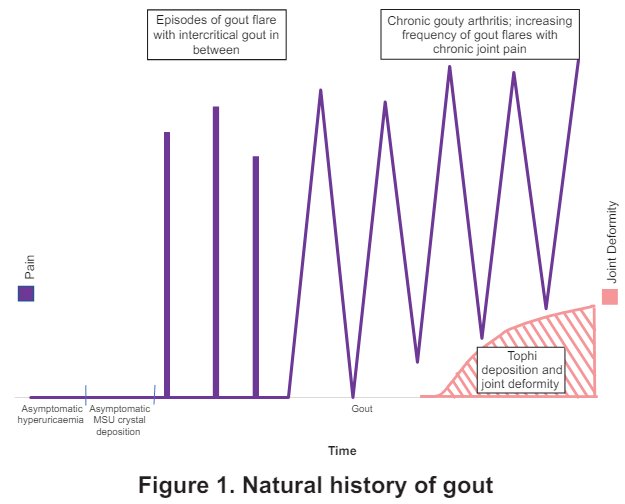
Not all individuals with hyperuricemia develop asymptomatic MSU crystal deposition or gout
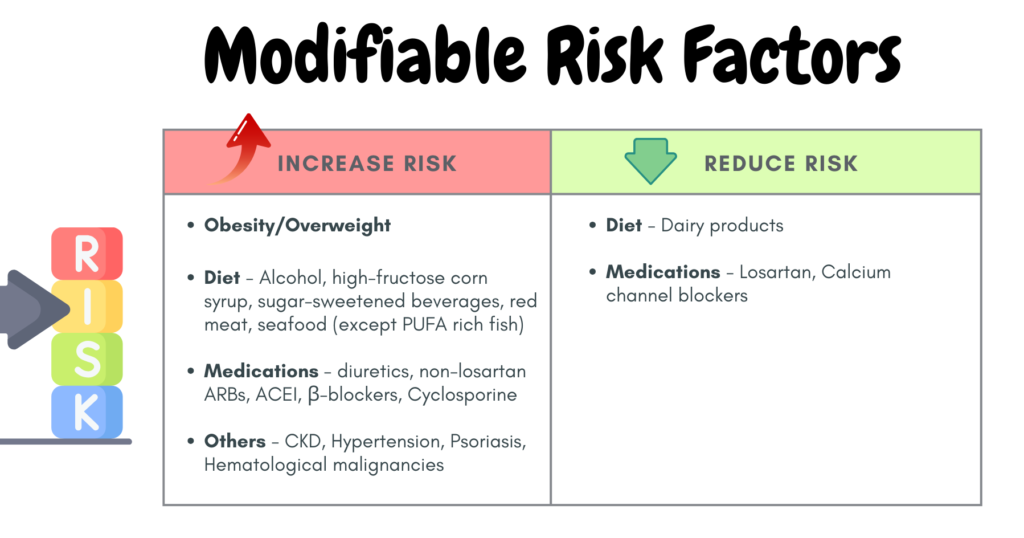
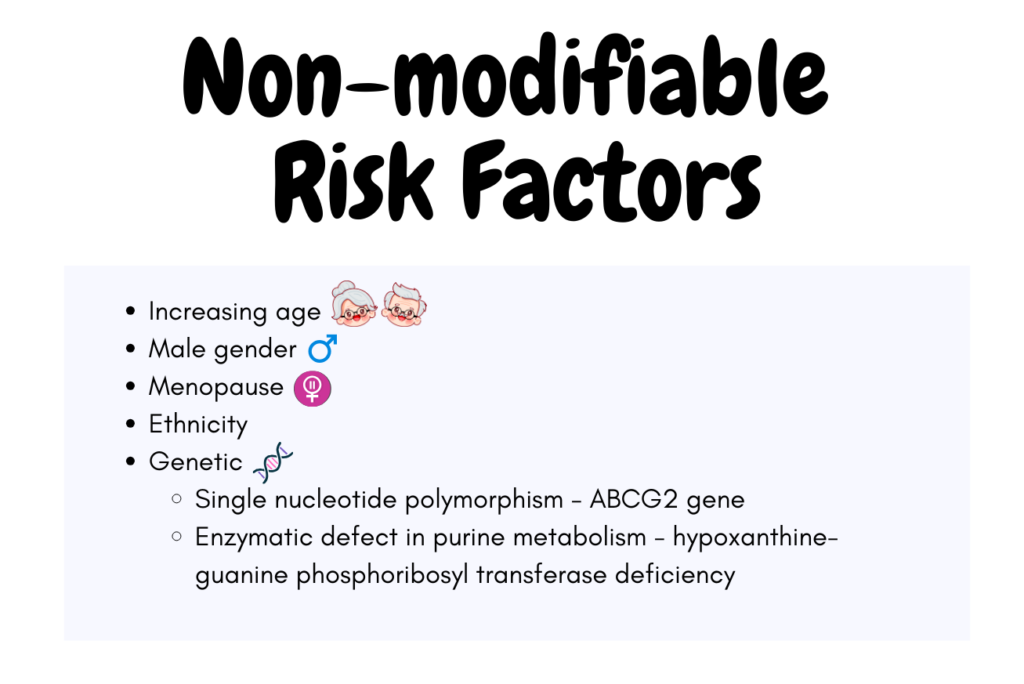
Risk factors for gout
3 clinical classical stages
- Gout flare – acute arthritis induced by MSU crystals
- Intercritial gout – asymptomatic period after or between gout flare
- Chronic gouty arthritis +/- tophi – joint deformity e.g. fixed flexion deformity


- 1st presentation of acute gout: typically acute monoarthritis of the 1st MTP joint (podagra), midfoot or ankle.
- Less commonly with oligoarthritis;
- Acute gout is generally self-limiting, lasting about 1 – 2 weeks.
- If hyperuricemia persist –> recurrent flares –> polyarticular gout (including those of upper limb)
- Common sites of tophi: 1st MTP joint, Achilles tendon, peroneal tendon, helix of the ear, olecranon bursa & finger pad.
Extra-articular manifestation: Urolithiasis, Chronic nephropathy (Thus, don’t forget to assess also patient’s Renal Function)
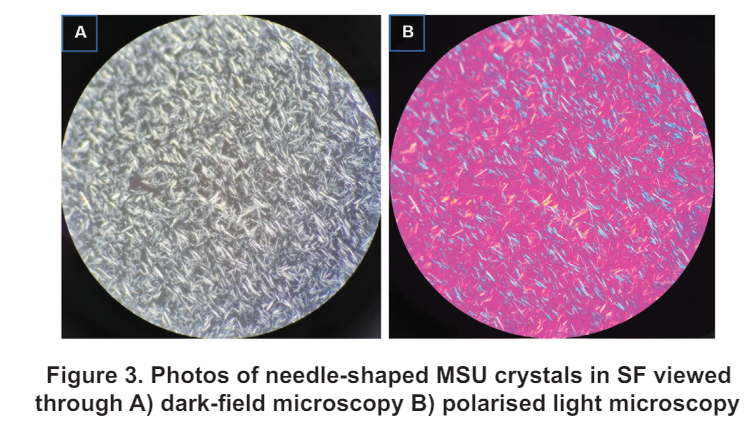
Diagnosis 🔬
Definite (gold standard): Demonstration of MSU (negative birefringent crystals) in synovial fluid or tophus.
Often time, this may not be possible, thus diagnosis can be made from clinical presentation, lab investigations & imaging modalities.
Laboratory investigations
Mainly serum uric acid (SU)
– Cut-off level to diagnose hyperuricemia: > 6.8 mg/dL (408 umol/L; 0.408 mmol/L) at physiological pH & body temperature.
Keep in mind that:
– Diagnosis of gout should not be made based on hyperuricemia alone.
– A normal/low SU during flare does not exclude gout as level may be normal during flare. If clinical suspicion is high, SU may be repeated 2 weeks or more after complete resolution of flare.
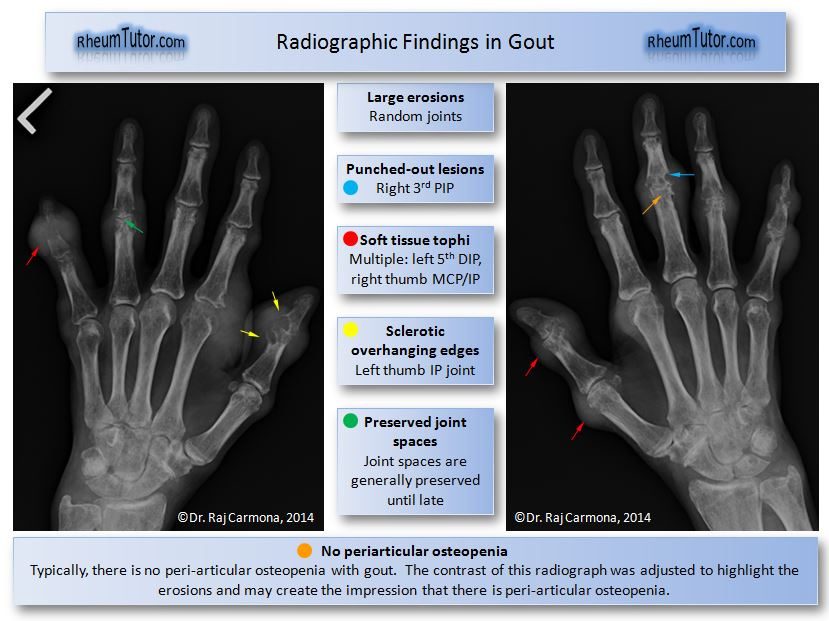
Imaging modalities – X-ray & ultrasound
Typical radiographic features of gout on plain radiograph:
– Bone erosions with overhanging edges and a sclerotic rim (“punched out”/”rat bite” erosions)
– Bony proliferation
– Joint space are generally preserved until late stages of the disease
– No peri-articular osteopenia
– Soft tissue tophi +/- calcification
ACR/EULAR gout classification criteria
Utilizes laboratory, imaging and clinical criteria to aid in diagnosis
Score of ≥ 8 can be classified as having gout
Accessible via: https://goutclassificationcalculator.auckland.ac.nz/
Co-morbidities
Gout is an independent risk factor for mortality due to coronary heart disease & kidney disease.
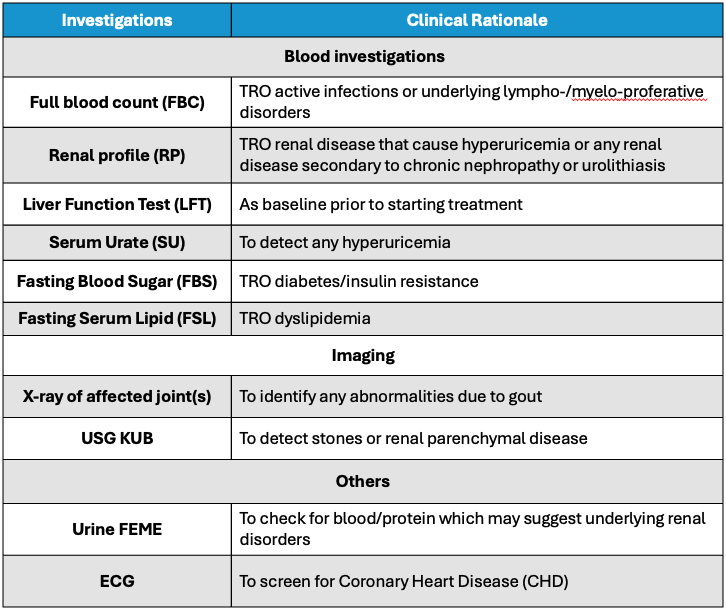
Screening for comorbidities e.g. HTN, DM, Dyslipidemia, CHD, & renal disease including urolithiasis should be done upon diagnosis & during follow up.
Below are the suggested baseline investigations which include screening for comorbidities as given in our Malaysia CPG guidelines.
Baseline investigations
Differential diagnosis
- Septic arthritis
– Commonly involves knee joint (other sites: hip, shoulder, ankle, wrist)
systemic features e.g. fever, ill or septic-looking
– Risk factors e.g. concomitant bacteria infection, recent intra-articular injection
– Leucocytosis and increased CRP - Acute calcium pyrophosphate crystal arthritis
– Age > 60 y/o
– Involvement of a degenerative joint
– Plain radiograph: chondrocalcinosis - Psoriatic arthritis
- Reactive arthritis
– Recent genitourinary or GI infection.
– Presence of urethral discharge or ulcer, rash on soles, conjunctivitis.
Prevention of gout
- Maintenance of healthy body weight
- Avoid alcohol
- Adherence to Dietary Approaches to Stop Hypertension (DASH) which:
– Discourages purine-rich red meat, fructose-rich foods, full-fat dairy products & saturated fat.
– Encourages vegetables, fruits, whole grains, fat-free or low-fat dairy products, fish, poultry, beans, nuts & vegetable oils. - Diuretics should be avoided if possible, or replaced by an alternative drug when used as an antihypertensive agent.
Dietary recommendations🥗


Notes:
- Benefits of n-3 PUFA-rich fish outweigh the potential risk.
- Plant-based purine-rich foods are not associated with increased risk of gout.
- Nuts & seeds are not associated with increased risk of gout.
Management of gout flare 🔥
Mainstay of treatment: pain relief
The following monotherapy may be used:
- Colchicine
- NSAIDs/COX-2 inhibitors
- Corticosteroids
Combination of the above may be used if response to monotherapy is insufficient.
Indications for Urate-Lowering Therapy (ULT)
Established indications:
- Recurrent gout flares (≥ 2 flares in 12 months) OR
- Presence of ≥1 tophi OR
- Presence of radiographic damage attributable to gout
Other conditional recommendations for ULT initiation after first gout flares:
– Moderate to severe CKD (Stage ≥ 3) OR
– SU concentration of > 9mg/dL (540 umol/L) OR
– Urolithiasis
Available ULT options
- Xanthine oxidase inhibitors – allopurinol & febuxostat
- Uricosuric agents – benzbromarone & probenecid
– Contraindicated in patient with urolithiasis & are not recommended in severe renal impairment. - Recombinant uricase – pegloticase
- Others – ? Ural sachet
Allopurinol
- 1st line
- Start at low dose & increase gradually.
- Severe cutaneous adverse reaction (SCAR) is the more serious A/E. There was a strong dose-response relationship between starting dose of allopurinol and Allopurinol Hypersensitivity Syndrome (AHS). Therefore always start low, go slow.
- Start low dose 50 mg or 100 mg & increase slowly every 4 weeks.
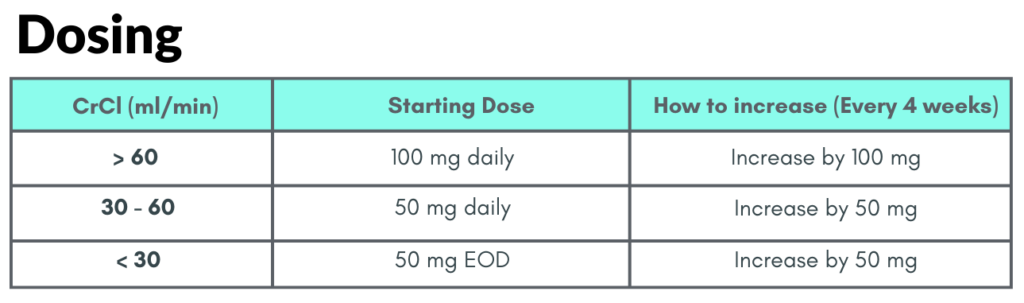
For healthy individuals:
Maintenance Dose: Usually ≥300 mg daily.
Maximum Dose: 900 mg daily.
Note: If the daily dose exceeds 300 mg, it should be split into 2 or 3 smaller doses throughout the day.
Allopurinol is generally well-tolerated, but some reactions can be very serious.
Warning: Patients with the HLA-B*58:01 gene are at a much higher risk for severe, life-threatening skin reactions.
Febuxostat
2nd line
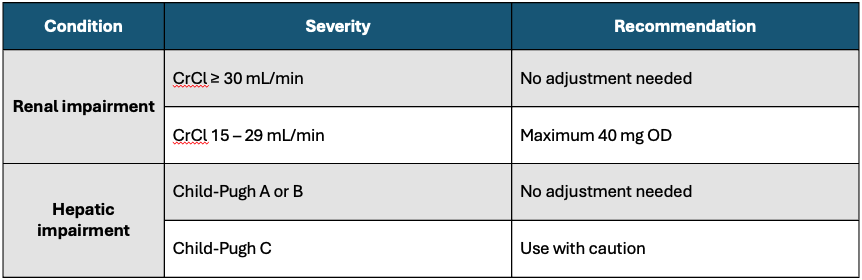
Can be used in patient with renal impairment (eGFR 15 – 89)
Dosing & Titration
- Initial dose: 40 mg OD
- Titration: if SU is still > 6.0 mg/dL after 2 – 4 weeks, consider increasing to 80 mg OD
- Maintenance: 40 mg or 80 mg OD
- Maximum: 120 mg OD if clinically indicated
Dosage modifications
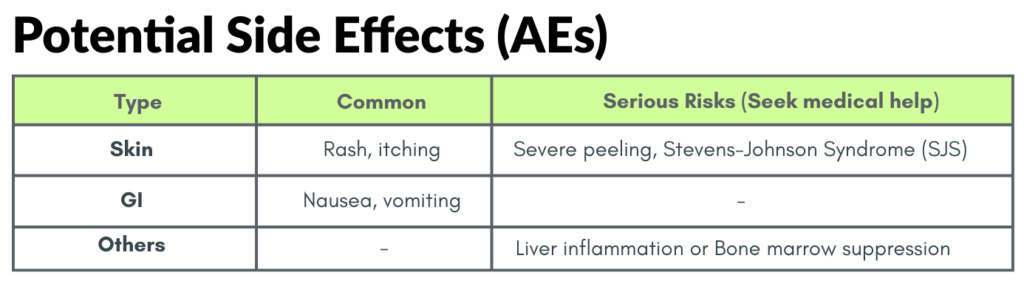
Potential Side Effects (AEs)
- Common: Rash, diarrhea, nausea & liver function abnormalities
- Serious skin reactions: Risk of DRESS, Stevens-Johnson Syndrome (SJS), & Toxic Epidermal Necrolysis (TEN)
- Cardiovascular Black Box Warning: Gout patients with established CV disease treated with Febuxostat have shown a higher rate of CV death compared to Allopurinol.
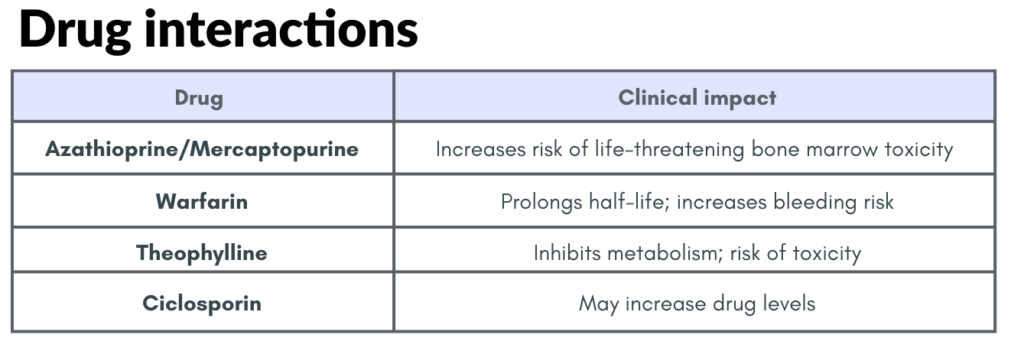
Major Drug Interactions
- Azathioprine/Mercaptopurine: Contraindicated. Concurrent use increases plasma concentrations of these drugs which can lead to severe toxicity.
- Methotrexate: May enhance hepatotoxic effects of methotrexate
Flare prophylaxis
Initiation of ULT leads to dissolution of MSU deposits which causes dispersion of crystals resulting in increased gout flares.
Concomitant anti-inflammatory agents should be started to reduce flares.
Preferred choice: Stepwise dose increase of ULT &/or concomitant colchicine (0.5 mg OD or BD).
Prophylaxis should be used for at least 3 – 6 months when initiating ULT.
Treat-to-Target (T2T) 🎯
Aim for serum urate< 360 umol/L (0.36 mmol/L) should be applied in treatment of all patients.
– A lower SU target of < 5mg/dL (300 umol/L; 0.30 mmol/L) for faster dissolution of crystals is recommended in severe gout (tophi, chronic arthropathy, frequent flares)
– However, some studies have suggested that urate might be protective against various neurodegenerative disease, thus prolonged SU < 3 mg/dL (180 umol/L; 0.18 mmol/L) is not recommended.
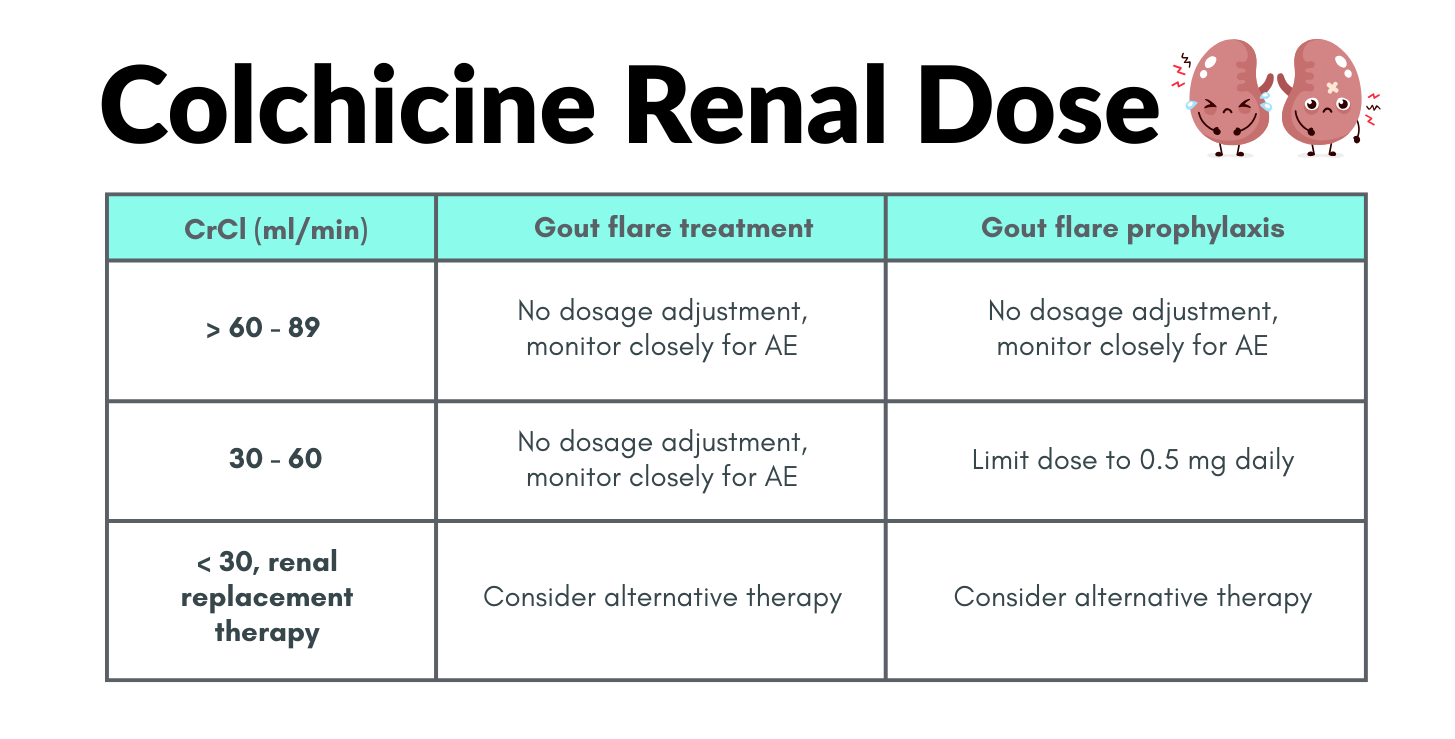
Gout in CKD patients
T2T strategy with renal dose adjustment.
ULT: Allopurinol (1st line), Febuxostat (2nd line), Uricosuric agent (contraindicated)
Gout flare: Corticosteroids may be used. Avoid NSAIDs. Colchicine (use with caution). Topical ice therapy safe to use.
Flare prophylaxis: Stepwise dose escalation of ULT, colchicine at reduced dose.
Follow up
Monitoring during Treat-to-Target
- SU, RP, LFT, FBC: Every 4 weeks during dose titration, then every 6 months once dose is stable.
- Screen/Monitor comorbidities at least annually: FBS, FSL, HbA1c
Indications for referral
- Diagnosis uncertainty
- Refractory to conventional therapy despite drug adherence
- Complicated gout with destructive joint changes
- Hypersensitivity or intolerance to allopurinol
- Gout in pregnancy
- Surgical management of tophi when there is uncontrolled infection, entrapment neuropathy & risk of permanent joint damage
- Gout with urolithiasis should be assessed by urologist
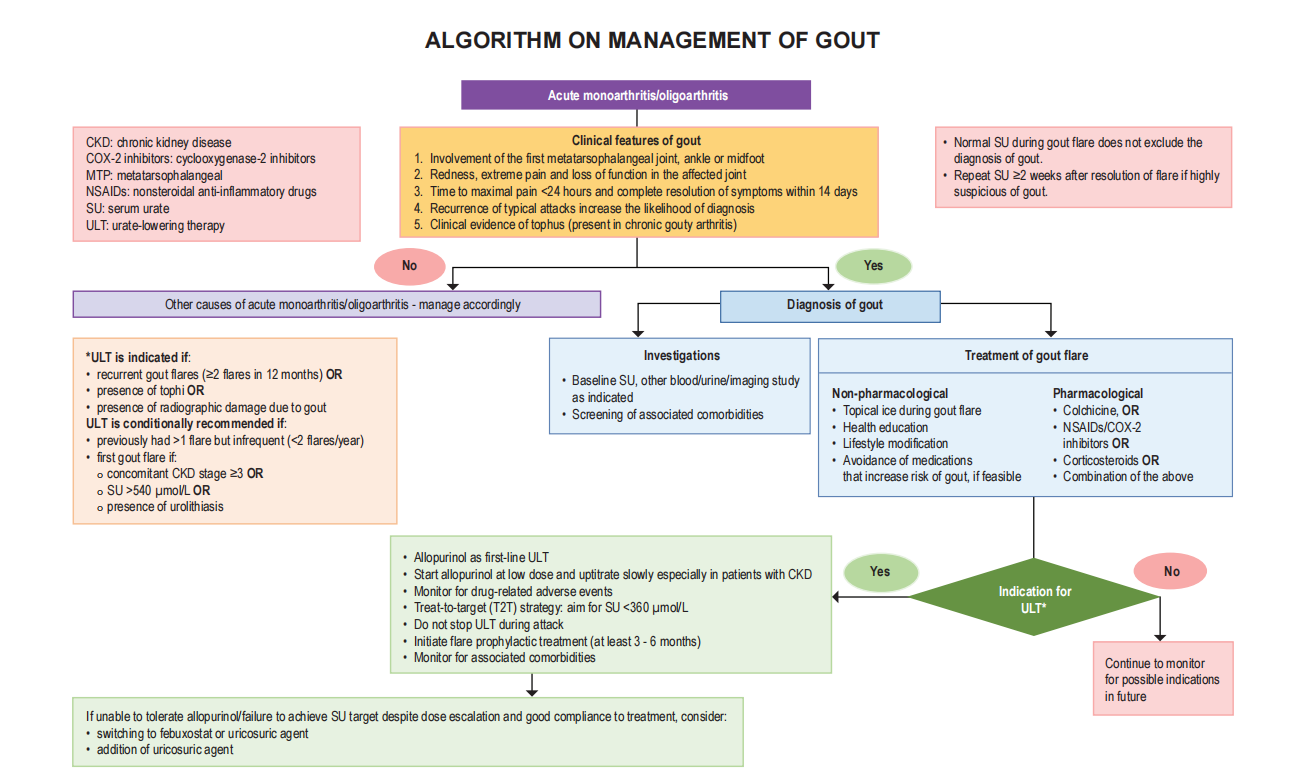
Summary Algorithm
References
Ministry of Health Malaysia. (2021). Clinical practice guidelines: Management of gout. Putrajaya: Ministry of Health Malaysia.
