MAFLD/MASLD

Metabolic-dysfunction Associated Fatty/Steatotic Liver Disease (MAFLD/MASLD)
Terminologies
In recent years, there has been a shift in terminologies from Non-Alcoholic Fatty Liver Disease (NAFLD) to Metabolic-dysfunction Associated Fatty Liver Disease (MAFLD) and the latest Metabolic-dysfunction Associated Steatotic Liver Disease (MASLD)
This shift in terminology is a reflect of the underlying pathophysiology whereby metabolic dysfunction has been shown to link with liver disease (rather than just labelling as non-alcoholic).
Changing the term “nonalcoholic” to “metabolic dysfunction” thus better reflect the etiology
Under MAFLD :
- There are no “primary” or “secondary” causes of fatty liver, only MAFLD & alternative causes of fatty liver.
- Covers dual liver pathology as MAFLD can coexist with other chronic liver disease (CLDs) e.g. MAFLD with Hep. C virus, MAFLD with alcoholic liver disease, etc.
- Enhanced detection of patients with significant or advanced hepatic fibrosis, CV risk, as well as a higher all-cause mortality.
MASLD was introduced in 2023 where the “fatty” in MAFLD is replaced with “steatotic”. The term “fatty” was considered to be stigmatizing, thus the rationale for changing to “steatotic” instead. However, there are still some differences in terms of the definition rather than just wordplay alone.
If you are interested in knowing more about the rationale in changing terminologies and further understanding the definition of each terminologies, you may refer to this article [link], which I think explained about it well.
In the context of this article, MAFLD and MASLD are used interchangeably.
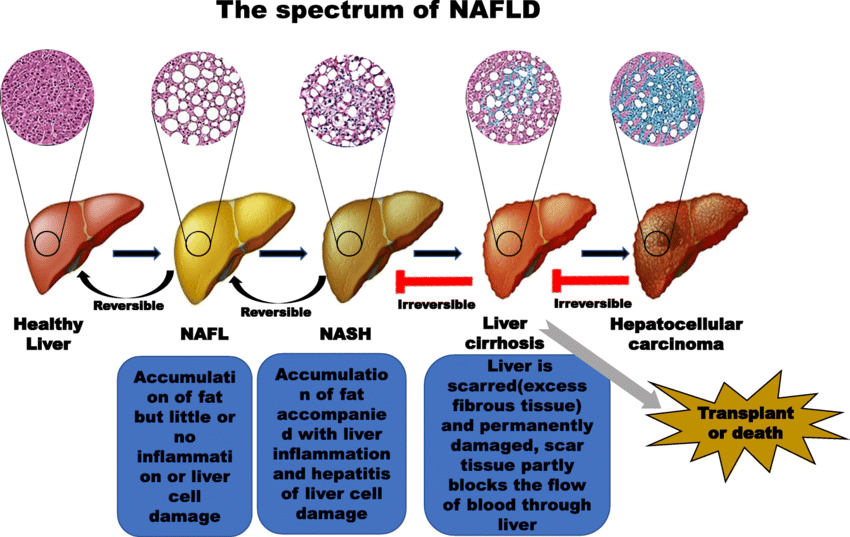
Spectrum of liver disease
In general, fatty liver progress through: Simple steatosis –> Steatohepatitis –> Cirrhosis –> Hepatocellular carcinoma (HCC)
The aim of detecting and managing MASLD is to hopefully reverse the steatosis and halt the progression of steatohepatitis to the stage of irreversible liver cirrhosis.
MAFLD diagnosis
Liver steatosis + metabolic comorbidities constitute MAFLD.
Once diagnosis is confirmed, evaluation of prognostic factors should be done (e.g. no fibrosis vs fibrosis vs cirrhosis)
It is important to note that a person who is having a normal BMI can also have MAFLD/MASLD –> Lean MASLD
Lean MASLD
- Seen in person with BMI < 23 kg/m² (cutoff for Asian populations)
- Probable cause:
– Genetic, e.g. PNPLA 3 mutation
– Insulin resistance/increased visceral adiposity (most common)
– Infections e.g. HIV, HCV (G3), coeliac disease, SIBO
– Drugs e.g. Tamoxifen, Amiodarone, Diltiazem
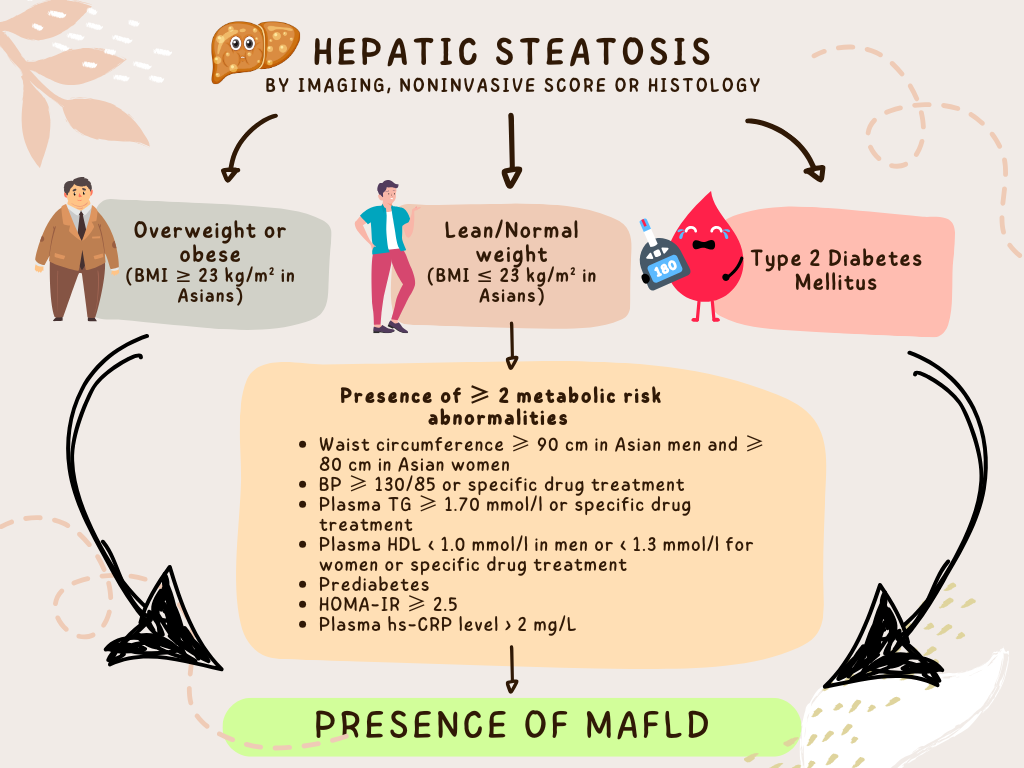
TG: Triglyceride
HDL: High-density lipoprotein
HOMA-IR: Homeostatic model assessment for insulin resistance
hs-CRP: high-sensitivity C reactive protein
The assessment of MASLD consist of:
- Diagnosis of fatty liver in the presence of metabolic dysfunction
– Fatty liver assessment can be done by using noninvasive score, imaging, or histology. - Fibrosis severity assessment – single most important predictor of liver-related complications & mortality.
- Determining risk of progression which is related to fibrosis stage at screening (especially if there is MASH), co-existing liver disease (alcohol, viral hepatitis, genetics, PNPLAs), other CV risk (particularly T2DM).
Fibrosis severity
Once MAFLD is diagnosed, the next step is to determine the severity of fibrosis.
This can be done by using either:
- Calculated scores (blood test) – FIB-4 score, NAFLD fibrosis score
- Imaging – Transient elastography (Fibroscan), MR elastography
Liver biopsy is considered the gold standard for assessment but it has its limitations (sampling variability, intra-/inter-observer variability & small risk of serious complications), and is reserved for patients with:
- Discordant noninvasive test
- TRO another liver pathology
- Diagnosis of steatohepatitis is uncertain or needs to be confirmed.
Fib-4 score
Can be calculated using patient’s age, AST, ALT and platelet count and is easily accessible through website like mdcalc.com.
Has a modest accuracy but high negative predictive values for advanced liver fibrosis.
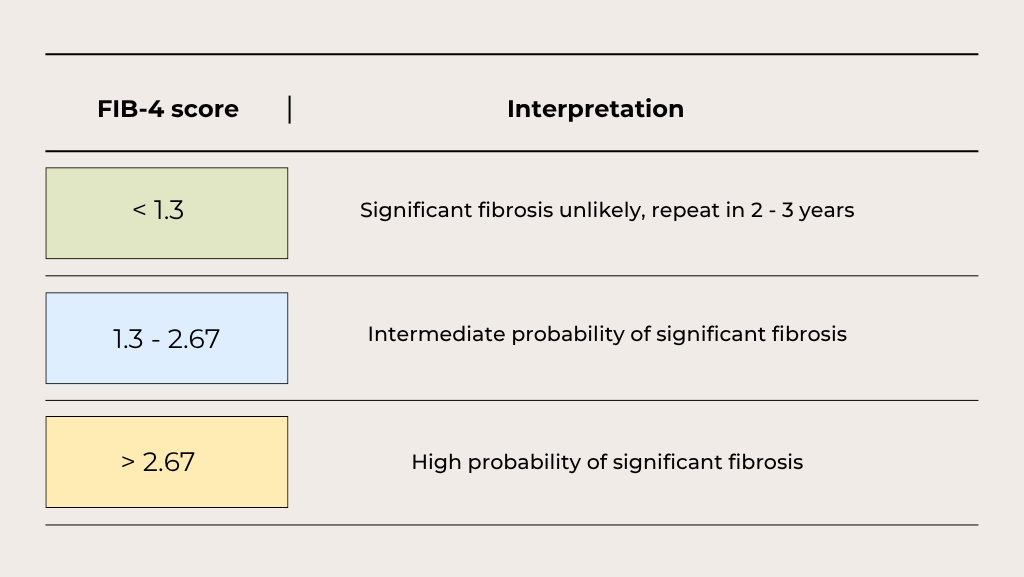
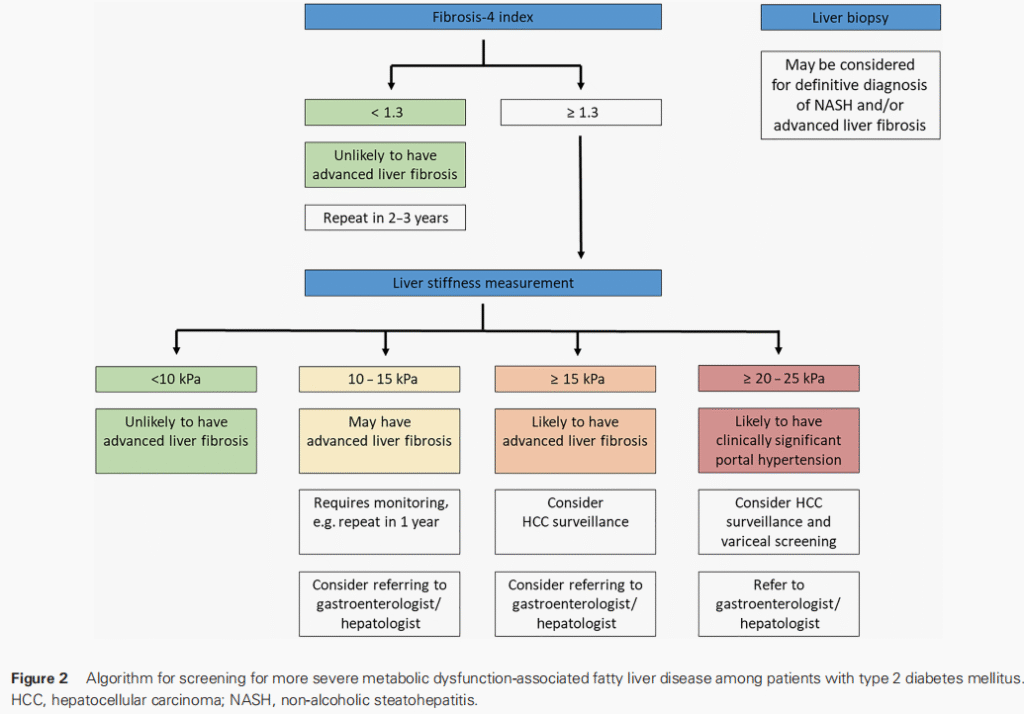
Generally, FIB-4 score of ≥ 1.3 requires measurement of liver stiffness (often by transient elastography) to decide on subsequent course of management.
FIB-4 followed by TE has been shown to have high diagnostic accuracy, avoiding unnecessary referral to specialist &/or liver biopsy.
This algorithm can serve as a guide in using FIB-4 score and liver stiffness measurement in the assessment of MAFLD.
Management of MASLD/MASH
MASH = Metabolic-dysfunction associated steatohepatitis
The goal of management is to reduce the progression +/- regression of the liver disease and at the same time reducing the cardiovascular risk. (Cardiovascular disease is the leading cause of mortality in MAFLD patients)
Diet and lifestyle remains the mainstay of management, this includes
Weight loss up to 1kg/week (7 – 10% in 12 months)
- Weight loss of ≥ 10% has led to NASH resolution in 90% and fibrosis improvement in 45 – 81% of subjects enrolled in a comprehensive lifestyle program.
- This works for both obese & nonobese individuals, though the amount of weight loss needed to achieve liver benefits is less in the nonobese patient.
- Greater weight loss is associated with greater disease improvement.
Calorie deficit
Exercise 30 mins/day, 5 times per week.
- Resistance exercise is preferred to aerobic exercise in the presence of poor cardiorespiratory fitness.

Management of metabolic risk factors
CVD risk is proportionate to the severity of fatty liver disease.
Management includes:
- Healthy & active lifestyle
- Smoking cessation
- BP management (use of ACEi or ARB is relatively contraindicated in patients with decompensated cirrhosis)
- Diabetes optimization
– SGLT2-I and GLP1-RA have been shown to have CV benefits beyond glucose lowering, with the added advantage of weight reduction.
– Both of these agents have been found to show improvement in hepatic steatosis - Lipid lowering
– Statins are safe to start if ALT/AST < 3x upper limit of normal
– Fibrates do not improve CVS outcome
Pharmacological treatment for MASH
Consist of novel classes of drugs with ongoing studies.
These classes of drugs include:
- Thyroid hormone receptor beta agonist – Resumetiron (MAESTRO study)
- Peroxisome proliferator-activated receptor agonists
- Dual glucagon-like peptide01 and glucagon receptor agonists
- Fibroblast growth factor 21
Bariatric surgery
Indicated for BMI > 35 kg/m² who failed lifestyle changes
When to refer?
- Significant fibrosis (FIB-4 score, liver stiffness measurement)
- Liver cirrhosis
- Hepatocellular carcinoma
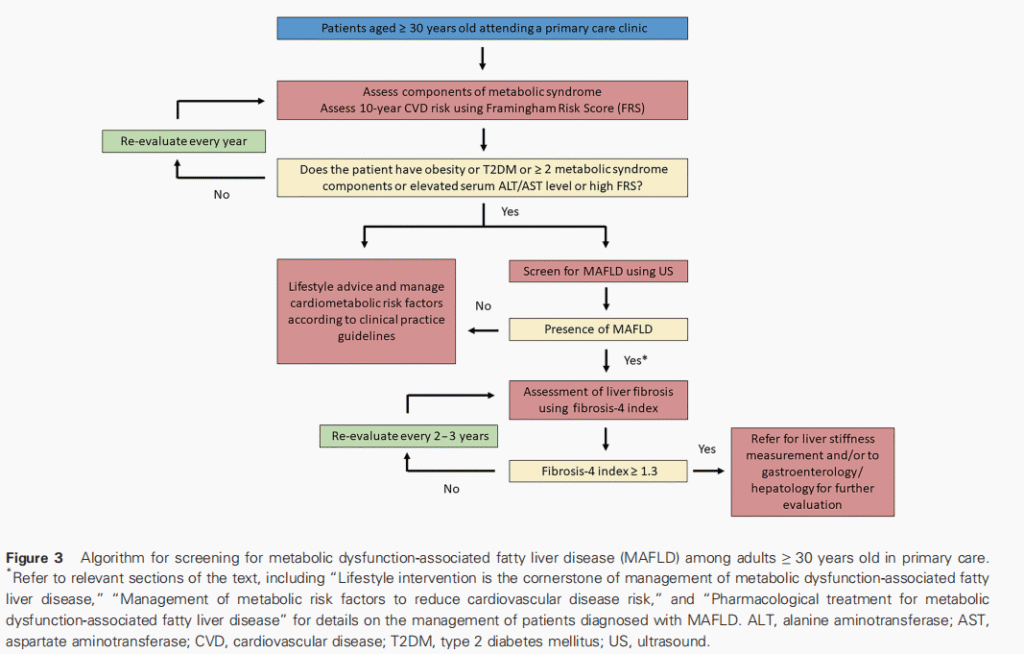
Role of primary care
Early identification & adequate treatment of cardiometabolic risk factors in patients with MAFLD.
Patients ≥ 30 years old should be assessed for the presence of metabolic syndrome and risk stratified using the Framingham risk score.
Patients with MAFLD & coexisting cardiometabolic risk factors should be targeted for aggressive lifestyle intervention & risk factor management.
Ultimate goal: prevent progression of MAFLD and improve CV outcomes.
MAFLD patients with less severe liver disease should remain in primary care or endocrinology when they are best managed.