Urolithiasis

Urolithiasis
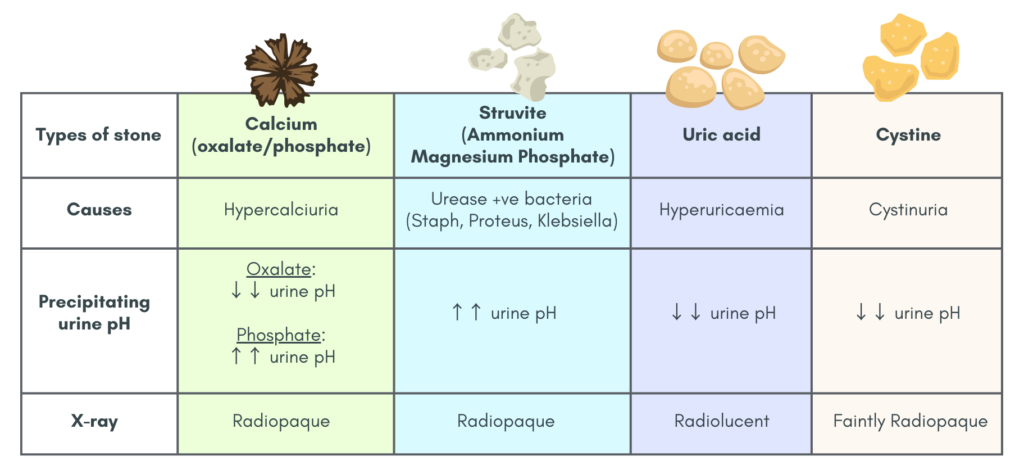
Types of stones
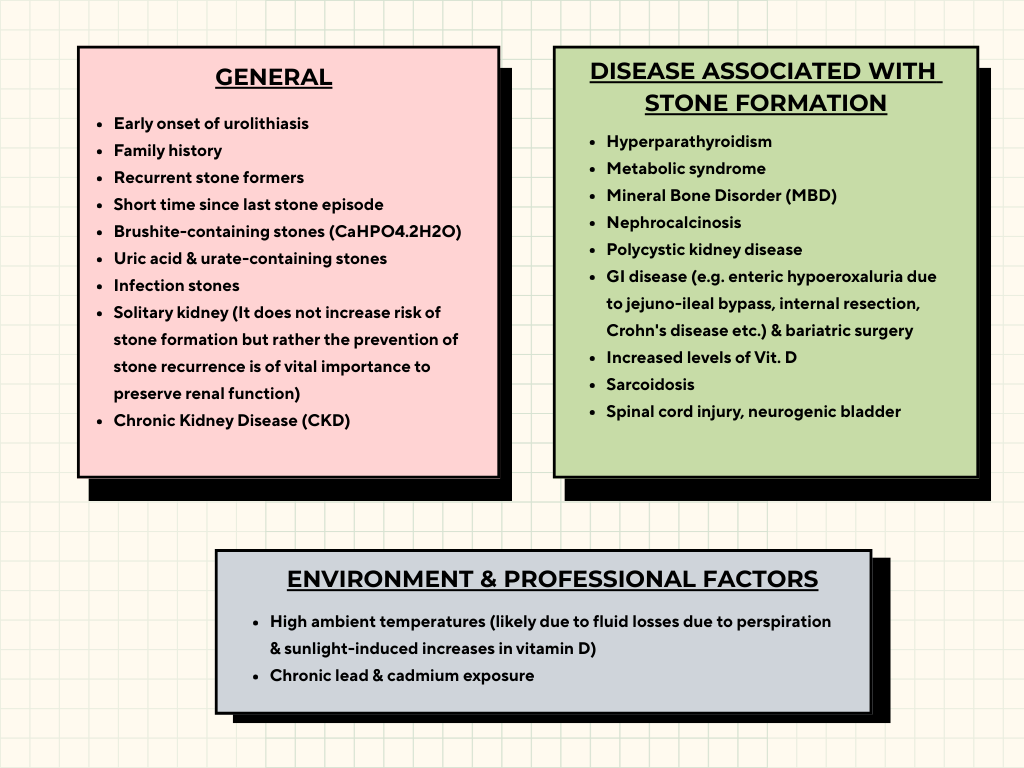
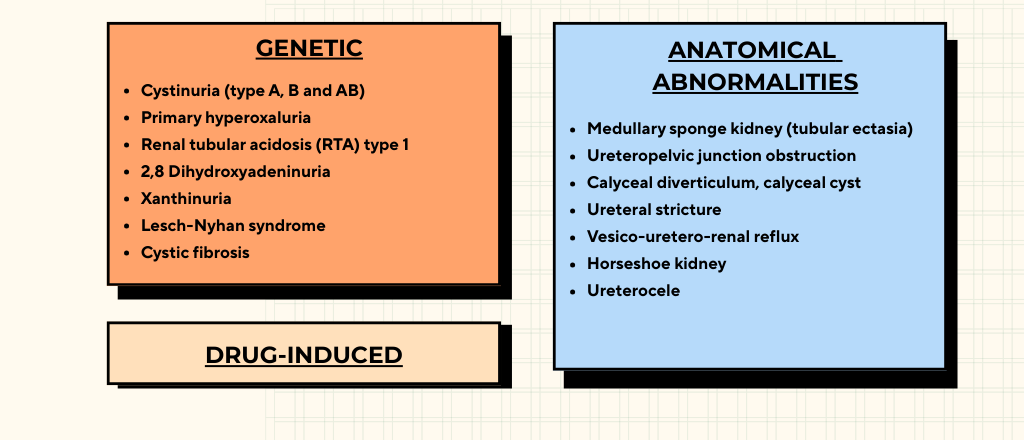
Risk factors
Clinical history
Patient can present with symptoms of
- Flank or abdominal pain (Loin-to-groin pain)
- Nausea or vomiting
- Hematuria
- Pyelonephritis secondary to obstructive uropathy
Remember also to enquire about risk factors e.g.
- Previous stone episodes, including age of onset.
- Family history (Positive family history is associated with earlier disease onset & higher risk of recurrence).
- Lifestyle – physical activity, diet
Basic investigations
1. UFEME
2. First-time stone-former: FBC, RP, stone analysis (using valid procedure, e.g. X-ray diffraction or infrared spectroscopy)
3. For recurrent stone-former, addition of:
- Stone analysis (should be done for each stone episodes as there may be changes in stone content)
- Serum (ionized) calcium, phosphorus, uric acid, magnesium
- Urinary calcium, phosphate, uric acid, magnesium, citrates & cystine level
4. If planned for intervention: PT, INR, blood grouping
24 hour urine tests (2 separate sample collections)
For biochemical workup – pH, minerals, oxalate, citrate & amino acids.
Recommended for patients with high risk of recurrent stone formation.
This can be used to guide medical prevention.
Collection of samples should be done for patients who have been stone-free for at least 20 days.
Repeat evaluation is recommended for patients on pharmacological treatment for recurrence (most consensus recommend 8 – 12 weeks after treatment).
Spot urine tests may be an alternative for those unwilling or unable to carry out 24 hour urine collection.
Imaging
USG is recommended as first line (however, sensitivity/specificity for diagnosing ureteric stones is low)
X-ray KUB is not sensitive & specific enough for the diagnosis of stone.
Non-contrast CT (best sensitivity & specificity), risk of radiation exposure should be considered.
- Low-dose NCCT protocol should be used for patients with BMI < 30 kg/m2, to minimize radiation risk to patients.
USG tips
Renal calculus
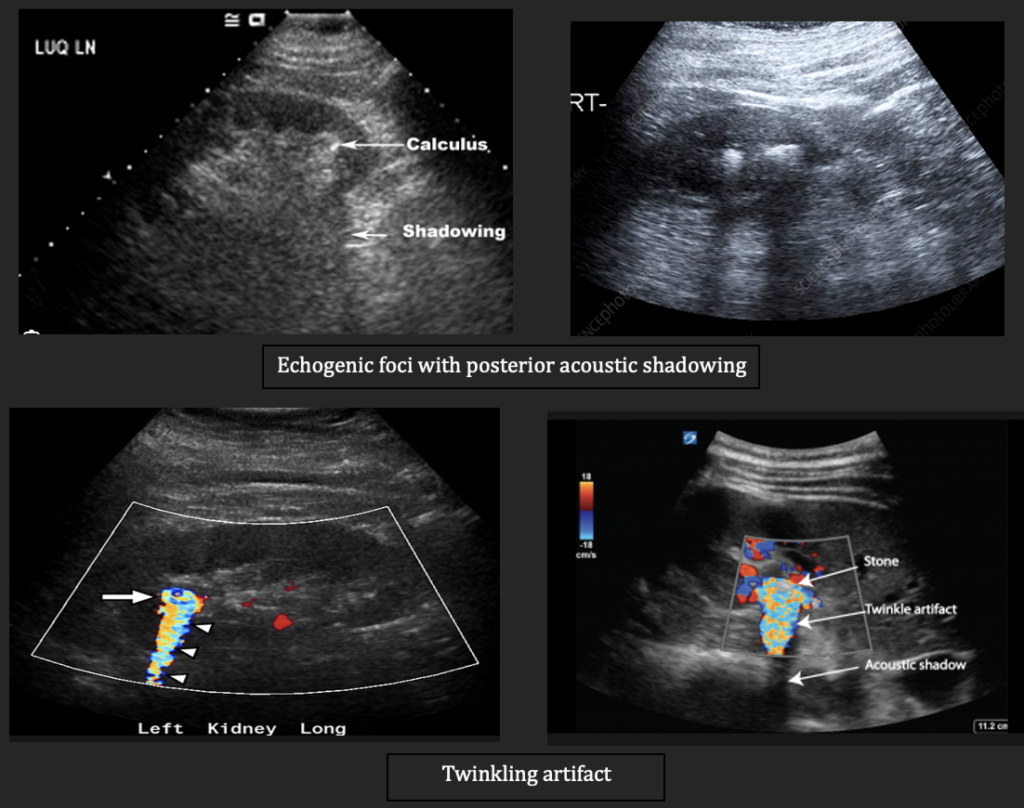
Calculus are often seen as echogenic focus that is associated with posterior acoustic shadowing.
In addition, if you put color doppler over the echogenic focus, twinkling artifact may be present which supports the diagnosis of renal calculus.
Ureteric calculus
In terms of ureteric calculi, it may be difficult to visualize unless they are located in the upper/proximal ureter or at the ureterovesical junction.
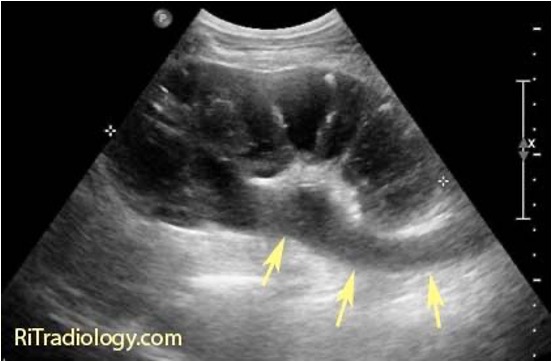
Instead look for these indirect signs:
- Hydronephrosis
- Dilated ureter (hydroureter)
- Decreased/absent ureteral jet (may be helpful, but are controversial)
Side note: If you are interested in further exploring the application of USG in primary care settings, you may consider this ebook which covers mainly on USG HBS and KUB and also some other common conditions encountered in primary care 👍🏼 [USG at the Point of Care – Focusing on HBS & KUB].
Determining renal function of each kidney
- Radionuclide scan
- Determining the creatinine clearance of urine obtained during percutaneous nephrostomy with or without self-void urine
- Assessment of cortical thickness using USG or NCCT
Investigation in special groups
Pregnant women 🤰
USG is the first line, followed by MRI as 2nd line. Low-dose CT is reserved as last option only if really indicated.
USG may not be able to differentiate between acute ureteral obstruction & physiological hydronephrosis of pregnancy, whereas MRI is able to.
Children 🧒
- Stone analysis
- Metabolic evaluation based on stone analysis
- USG as 1st line
- KUB radiography/low dose NCCT if USG unable to provide the required information
Medical treatment
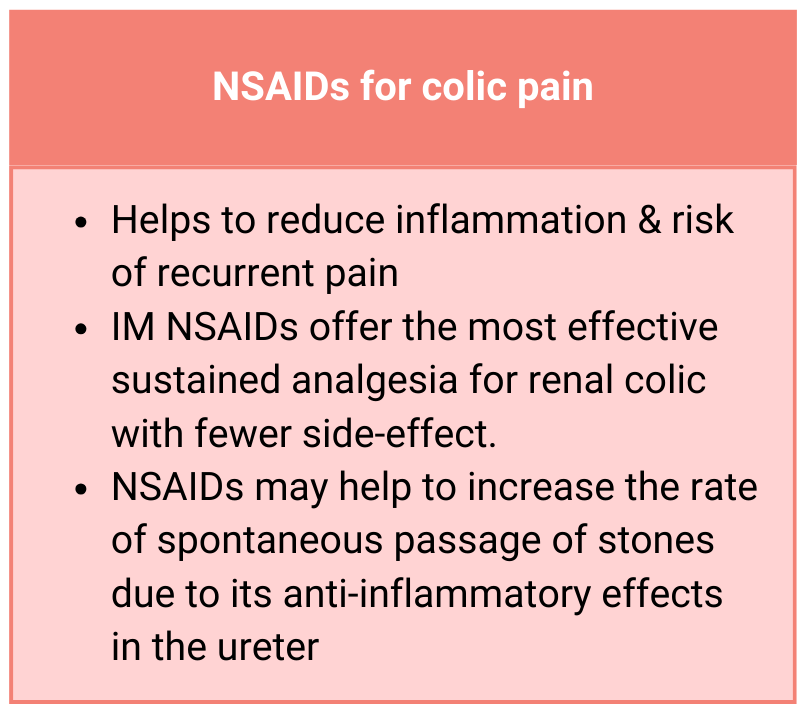
Additional comments on pain management:
- Opiates like tramadol are 2nd choice if patient is unable to tolerate/contraindicated to NSAIDs.
- Renal decompression or ureteroscopic removal of stone may be needed for refractory pain.
If patient’s symptoms are not improving/worsening, referral for further assessment & intervention (e.g. SWL/URS/PCNL) should be done.
Emergency treatment (urgent decompression + antibiotics) is required for an obstructed & infected kidney. Patient should be referred to tertiary center immediately.
Approach to stones according to location
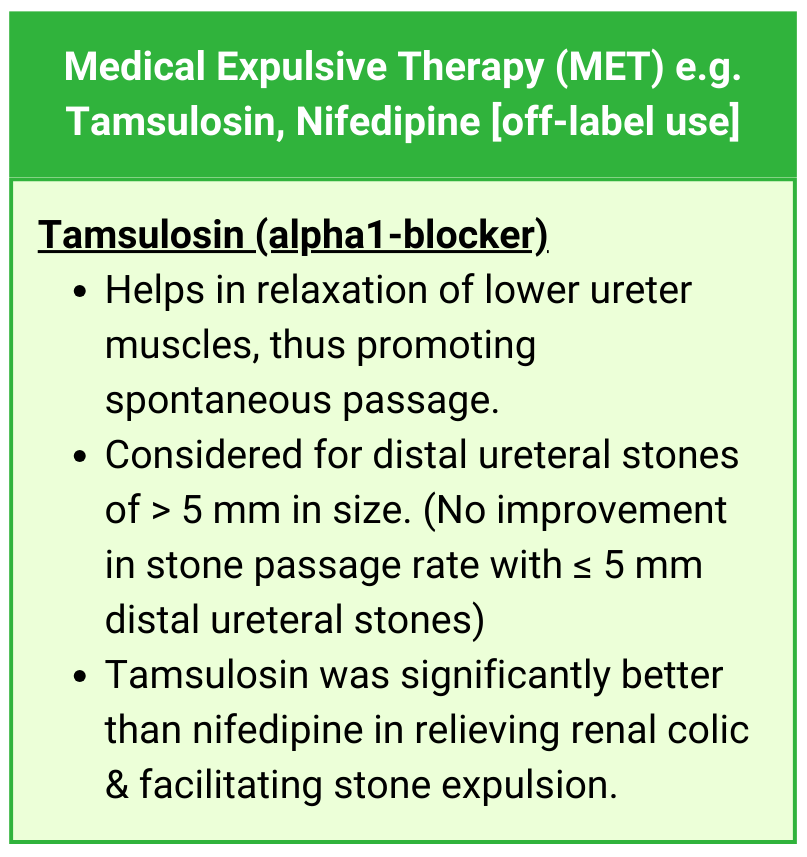
Ureteral stone
Observation with periodic evaluation is feasible in informed patients if there are no complications like infection, refractory pain or deterioration of kidney function.
Alpha-blockers (MET) can be a treatment option for distal ureter stones > 5 mm (Off-label)
Indication for active stone removal (to refer urologist):
- Stones with low likelihood of spontaneous passage
- Persistent pain despite adequate analgesia
- Persistent obstruction
- Renal insufficiency (renal failure, bilateral obstruction, single kidney)
Renal stone
Active surveillance can be offered for patients with asymptomatic renal stones.
There is still some dilemma whether all renal stones should be treated or if annual follow up is sufficient for asymptomatic calyceal stones that have remained stable for 6 months.
Indications for active stone removal include:
- Stone growth
- Stones in high-risk patients for stone formation
- Obstruction
- Infection
- Symptomatic (e.g. pain, hematuria)
- Stones > 15 mm
- Stones < 15 mm if observation is not the option of choice
- Patient preference
- Comorbidity
- Social situation of the patient (e.g. travelling or profession)
Bladder stone – will be discussed in later section
General preventive measures for stone recurrence
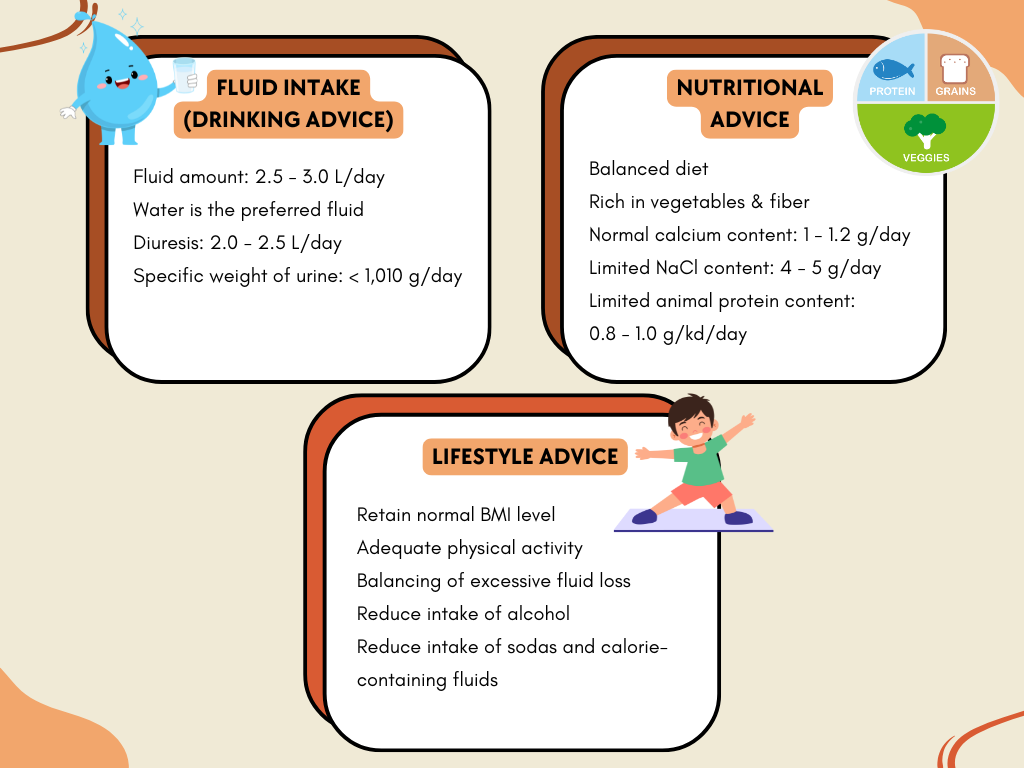
Hydration helps prevent stone formation via urine dilutional effect.
Dietary salt (NaCl) is linked to calcium excretion in urine.
- High dietary salt reduces the efficacy of reabsorption of sodium & water in renal proximal tubules, which prevents calcium reabsorption –> hypercalciuria –> facilitate stone formation.
Animal protein lowers urinary pH & increases uric acid in urine –> risk for uric acid & calcium stone formation.
Regarding supplements
- Avoid excessive Vitamin C especially for calcium oxalate stone formers. (There are studies that show this mainly applies to men, whereas women are not particularly affected – Pubmed reference)
- Normal daily calcium requirement is advised but not in excessive.
- Magnesium may have a role in preventing urinary stones as urinary magnesium forms complexes with oxalate, thus reducing calcium oxalate supersaturation in urine. However, magnesium as sole therapy is ineffective & not recommended. (Promising results have been shown when magnesium is used with other stone inhibitors).
High-risk stone formers require specific metabolic evaluation & stone analysis for appropriate preventive measures
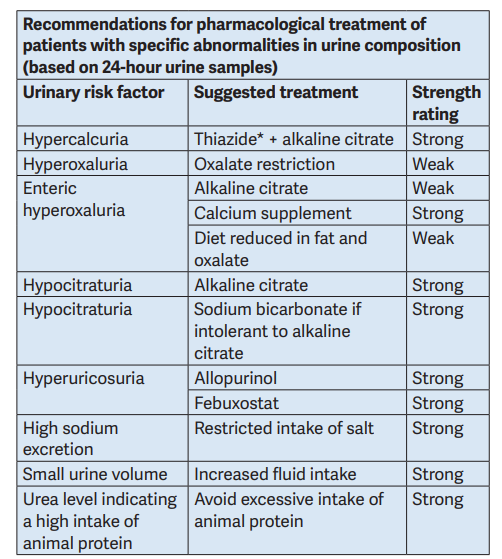
* Patients on hydrochlorothiazide should be advised to get their skin checked regularly due to higher risk of developing an NMSC and some forms of melanoma. In patients with history of skin cancer, the indication for treatment with hydrochlorothiazide should be thoroughly reviewed.
This table is just a summarization of the suggested treatment. More detailed approach and algorithm are available in the EAU guideline.
Bladder stones
Higher prevalence in males.
Classification
- Primary/endemic: Absence of other urinary tract pathology, seen in children in areas with diet deficient in animal protein, poor hydration, & recurrent diarrhea.
- Secondary: In presence of other urinary tract abnormalities e.g. bladder outlet obstruction, neurogenic bladder, chronic bacteriuria, foreign bodies including catheter, bladder diverticula, bladder augmentation or urinary diversion.
- Migratory: Stones passed from upper urinary tract into the bladder which serve as a nidus for bladder stone growth.
Diagnostic imaging
- USG as first line.
- X-ray KUB/cystoscopy/CT if there are persistent suggestive symptoms where USG is negative
Other investigations to consider
- Uroflowmetry & post-void residual
- Urine dipstick, pH, +/- culture
- Metabolic assessment & stone analysis
- Upper tract imaging (if there is h/o urolithiasis or loin pain)
- Cysto-urethroscopy or urethrogram
Management
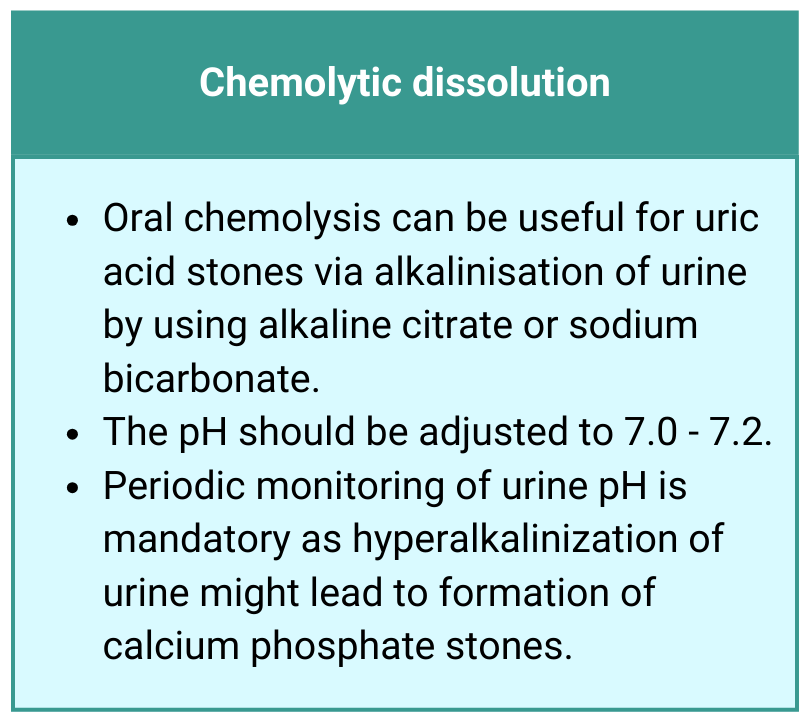
- Oral chemolysis can be considered for radiolucent/known uric acid stones.
- Irrigation chemolysis is possible for struvite or uric acid stones.
- Active removal includes open, laparoscopic, or robotic assisted laparoscopic or endoscopic (transurethral or percutaneous) surgery, or extracorporeal SWL.
References
- Taguchi K, Cho SY, Ng AC, Usawachintachit M, Tan YK, Deng YL, Shen CH, Gyawali P, Alenezi H, Basiri A, Bou S, Djojodemedjo T, Sarica K, Shi L, Singam P, Singh SK, Yasui T. The Urological Association of Asia clinical guideline for urinary stone disease. Int J Urol. 2019 Jul;26(7):688-709. doi: 10.1111/iju.13957. Epub 2019 Apr 24. PMID: 31016804.
- Skolarikos, A., Jung, H., Neisius, A., Petřík, A., Kamphuis, G. M., Davis, N. F., Somani, B., Tailly, T., Lardas, M., Gambaro, G., & Sayer, J. A. (2024). EAU guidelines on urolithiasis. European Association of Urology.
