H. pylori
Helicobacter pylori
Helicobacter pylori (H. pylori) is a gram negative, flagellated, spiral bacteria that primarily colonizes the stomach and is largely responsible for gastric and or duodenal ulcers.
It is also a class I carcinogen that may increase one’s risk of gastric carcinoma.
Transmission of H. pylori is thought to be via fecal-oral, oral-oral and may include gastro-oral routes.
Patients who have H. pylori infection may be asymptomatic or may present with dyspepsia symptoms (Topic on dyspepsia has been discussed in another post, click here to read more on it).
Diagnosis of H. pylori infection
Can be divided into invasive and non-invasive
|
Tests |
Comments |
|---|---|
|
Invasive | |
|
Rapid urease test (RUT) |
Patients who are undergoing gastroscopy should have biopsies for RUT. Highly sensitive and specific |
|
Culture |
Allows for determination of antibiotic susceptibilities Not widely available |
|
Histology |
In addition to detecting H. pylori, can provide more information about the degree of inflammation & associated pathology, e.g. atrophic gastritis, intestinal metaplasia, & gastric cancer. Usually reserved for those who tested negative on RUT or TRO malignancy. |
|
Non-invasive | |
|
Urea breath test |
High sensitivity and specificity Useful for diagnosing current H. pylori infection and for follow up post-treatment. Multiple point assessment may be preferred over single point test. |
|
Serological test |
Limited diagnostic accuracy Cheap and widely available Not suitable for post-eradication monitoring (antibody can remain positive post eradication) |
|
Stool antigen test |
Can be used for pre-treatment diagnosis and post-treatment monitoring |
Accuracy of these diagnostic tests mentioned above (with the exception of serological test) can be affected by treatment with antimicrobials (e.g. antibiotics or bismuth) or PPIs as they may reduce the H. pylori intragastric load leading to false negative.
Thus, to ensure a more reliable results, diagnostic tests or post-treatment tests should be delayed by at least 2 weeks if patient was on PPIs and at least 4 weeks if patient was on antibiotic.
Serological tests are not affected by PPIs or antibiotic, but as mentioned above, its accuracy is limited and cannot be used for post-treatment monitoring.
Who to test for H. pylori infection?
- Patients with current or past gastric or duodenal ulcers
- Patients with uninvestigated dyspepsia
- Patients with mucosa-associated lymphoid tissue (MALT) lymphoma
- Individuals with family history of gastric cancer [1st degree relatives of patients with gastric cancer have higher risk of developing gastric cancer]
Treatment of H. pylori infection
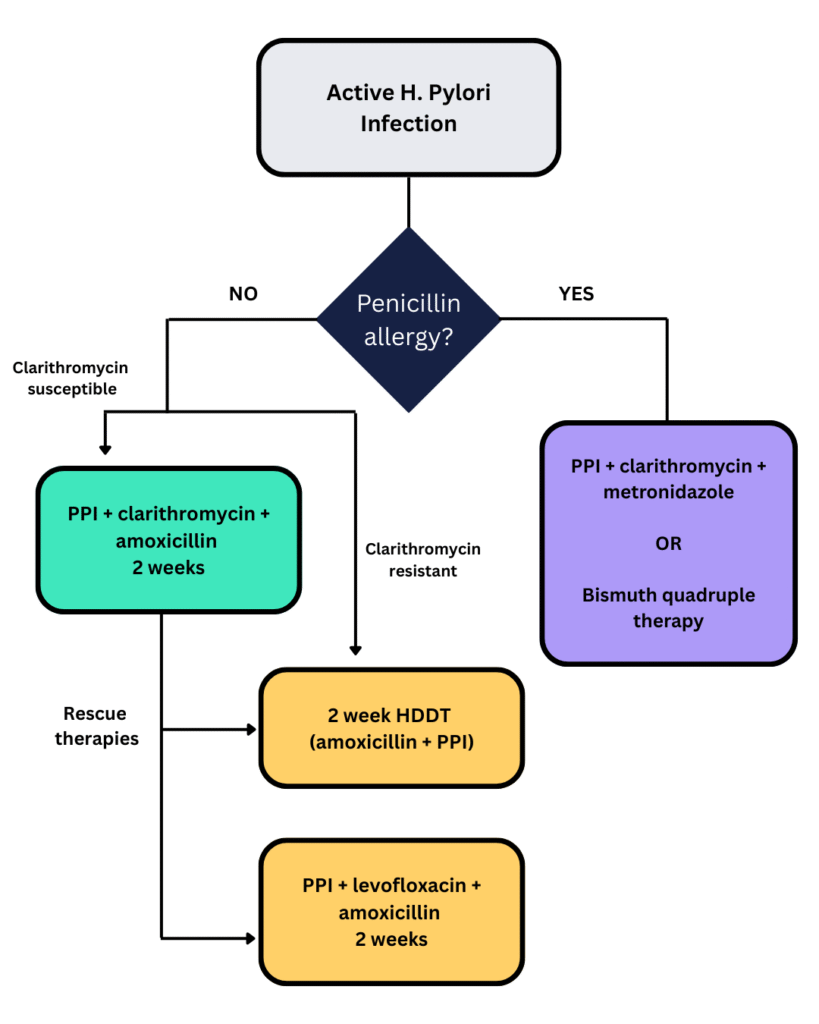
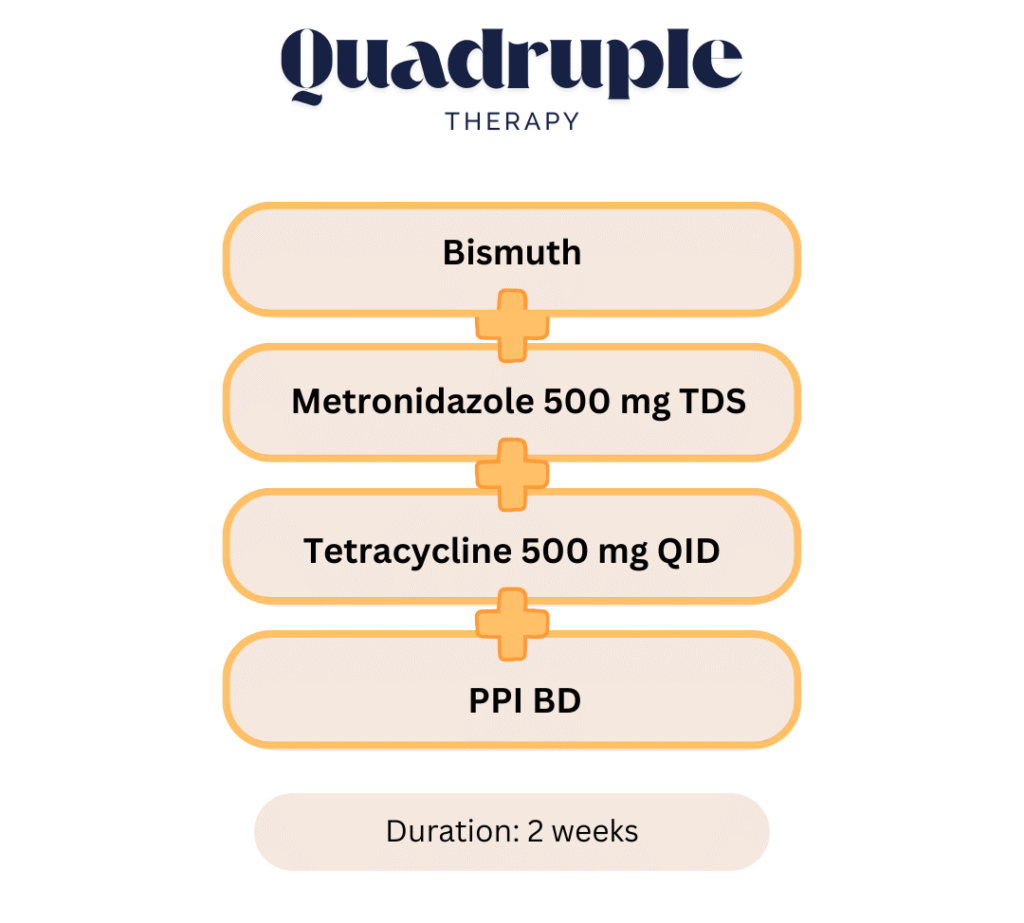
In Malaysia, triple therapy consisting of amoxicillin + clarithromycin + PPI is still considered the first line of treatment. If patient has penicillin allergy, then amoxicillin can be substituted with metronidazole or bismuth quadruple therapy can be considered, although bismuth compounds are not widely available in Malaysia.
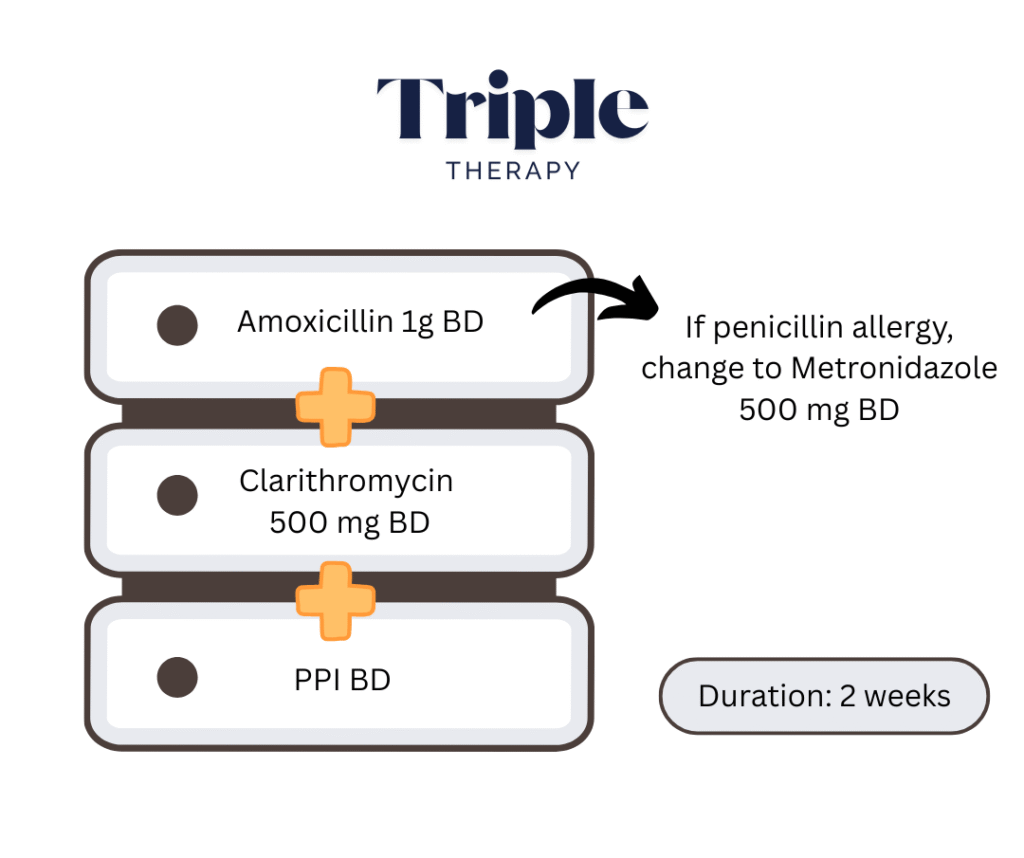
There are concerns regarding clarithromycin and metronidazole resistance, especially in the Western countries and this is reflected in the ACG/Canadian guidelines where their recommended therapy usually does not include clarithromycin unless susceptibility is confirmed.
Nevertheless, in Malaysia the resistance rate towards clarithromycin are still considered low.
There are no cases of H. pylori resistance to amoxicillin at least up to the date that the guideline was published
High dose dual therapy
High dose dual therapy can be considered in cases of clarithromycin resistance or as rescue therapy where patient has failed the standard triple therapy.
Generally consists of amoxicillin 1 g TDS + PPI TDS dose but there had been regimen that goes up to QID.
Multiple doses of amoxicillin ensure a stable above the minimum inhibitory concentration and multiple doses of PPI can provide a sustained level of acid suppression. Increasing the intragastric pH to >= 6 also increases the sensitivity of H. pylori to amoxicillin.
PCAB based treatment
Potassium-competitive acid blocker (PCAB) triple therapy or high-dose PCAB dual therapy are other promising eradication regimens.
PCAB (Drug name vonoprazam) is a new class of gastric acid suppressing agent that has shown similar efficacy when used in place of the conventional PPI in triple therapy.
The regimen generally is similar to the triple therapy where the only difference is that PCAB is used instead of PPI.
E.g. PCAB + amoxicillin + clarithromycin
Another potential benefit is that the duration of PCAB based triple therapy may be shortened to 1 week as it shows similar efficacy to the conventional 2 weeks of treatment.
Other regimens
These include:
- Sequential regimen followed by levofloxacin-based triple regimen, e.g. PPI BD + amoxicillin BD for 5 – 7 days, then PPI BD + levofloxacin + metronidazole BD for 5 – 7 days.
- Reverse hybrid therapy, e.g. PPI + amoxicillin + 2 other antibiotics (usually clarithromycin and metronidazole) for 7 days, then PPI + amoxicillin for 3 – 7 days.
These regimens have shown promising results but have not been tested in Malaysia settings.
Other than these, there are other regimens mentioned in the ACG/Canadian guidelines in which you can read up on further to know more about it. This post is mainly focusing on treatment regimen that are more relevant in the Malaysia setting in accordance to the Malaysian consensus report.
Failure of 1st line regimen
Possible cause: poor patient compliance, resistant strains of H. pylori, low intragastric pH, or high bacterial load.
Patient should not be re-treated with the same 1st line regimen.
Clarithromycin should not be consecutively administered as 2nd line regimen due to concern of therapeutic failure secondary to clarithromycin resistance.
Testing for antibiotic susceptibility is recommended but not mandatory.
Rescue therapy that can be considered include:
- 2 weeks high dose dual therapy (PPI + amoxicillin) or
- PPI-amoxicillin-levofloxacin therapy
Propose algorithm for eradication therapy