
Atopic Eczema (Atopic Dermatitis)
Atopic dermatitis (Atopic Eczema [AE]) is a complex, chronic & recurrent inflammatory itchy skin disorder.
Starts to develop in early childhood & may persist into adulthood.
Can present with various clinical manifestations according to different age groups.
Typically an episodic disease of flares & remission.
Caused by complex interactions of genetic predispositions (filaggrin gene), environmental triggers & immune dysregulation leading to epidermal barrier defect.
Co-morbidities e.g. skin infection, atopic disease(asthma, allergic rhinitis), food allergy, CVS disease, psychological & psychosocial dysfunction (e.g. ADHD, schizophrenia & affective disorders) may co-exist in AE.
Prevalence of AE is increased with exposure to active & passive smoking.
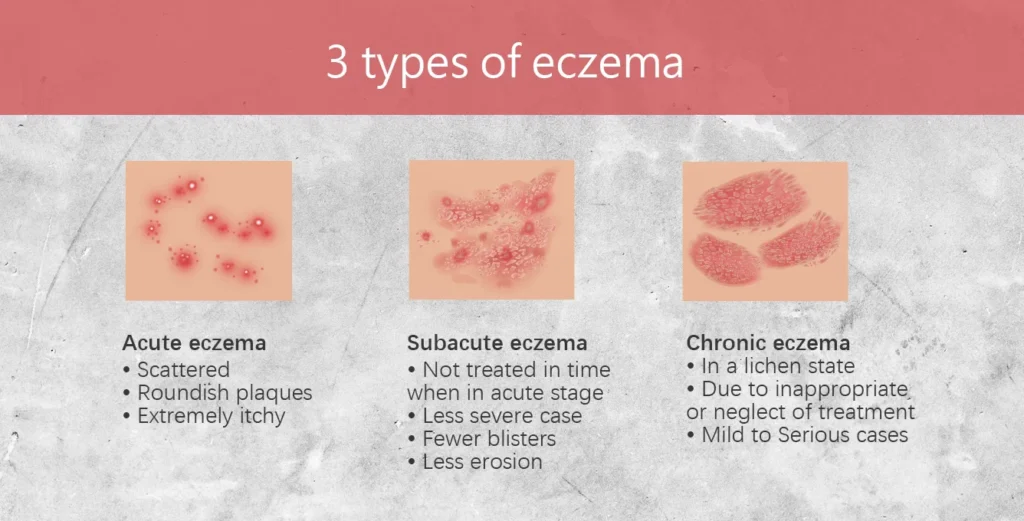
Acute vs Chronic
- Acute eczema: papulo-vesicular eruption with erythema, weeping, oedema & excoriation.
- Chronic eczema: lichenification & dry skin.
Diagnosis
Atopic eczema is a clinical diagnosis which can be aided by several validated diagnostic tools, e.g. UK Working Party’s Diagnostic Criteria, Hanifin and Rajka Diagnostic Criteria.
Serum IgE levels, skin prick test, patch test & skin biopsy should not be used as diagnostic tools for atopic eczema.
UK Working Party’s Diagnostic Criteria
Patient must have an itchy skin condition (or parental report of scratching/rubbing in a child) plus 3 or more of the following:
- History of skin creases involvement e.g. folds of elbows, behind the knees, fronts of ankles or around the neck (including cheeks in children < 10 y/o)
- Personal history of asthma or hay fever (or h/o atopic disease in a 1st degree relative in children < 4 y/o)
- History of general dry skin in the last year.
- Visible flexural eczema (or eczema involving the cheeks/forehead & outer limbs in children < 4 y/o)
- Onset under age of 2 (not used if child is under 4 y/o)
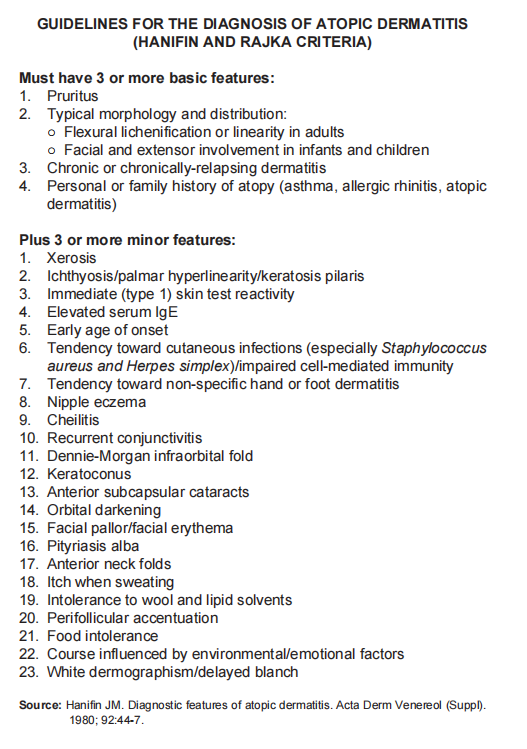
Hanifin and Rajka Diagnostic Criteria
Severity assessment
Preferred tools used for the assessment of disease severity & QOL are:
– Investigator’s Global Assessment (IGA)
– Dermatology Life Quality Index/Children’s Dermatology Life Quality Index
Aggravating/Triggering Factors
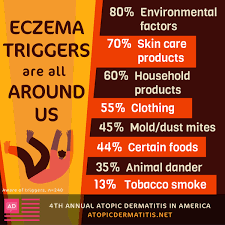
- Aeroallergen: house dust, unfamiliar pets (not own pets)
- Physical irritants: nylon/wool clothing, soaps, detergents, disinfectants, sweat, other chemical reagents etc.
- Environmental factors:
– Climate – warm & high sun exposures.
– Air pollution – indoor & outdoor - Food: May worsen AE in children < 2 y/o especially milk, egg & peanuts.
- Microbial colonisation/infection
- Patient factors (e.g. pregnancy)
– The hormonal changes in pregnancy results in predominant Th-2 response which us a/w atopy.
– There is no good quality evidence to show that stress aggravates AE.
Treatment
Topical treatment
Mainstay of treatment in atopic eczema.
Includes: emollient, topical anti-inflammatory agents & topical antiseptic/antimicrobial agents
A. Emollient/Moisturizer
- Mainstay of management in atopic eczema.
- Improves the epidermal barrier function & dryness leading to reduction in pruritus.
- Emollients have shown to enhance the effectiveness of topical corticosteroids (TCS) & have steroid-sparing property.
- Regular use of emollients improves atopic eczema & thus reduces usage of TCS.
- Different formulations:
– Ointments (e.g. petrolatum), greasy in nature
– Creams & lotions, contain water & are more user-friendly
– Creams (e.g. aqueous cream & urea cream), lotions & gels contain preservatives to protect against microbial growth in the presence of water

B. Topical corticosteroid (TCS)
- Inhibit fibroblast proliferation & collagen synthesis, causing local vasoconstriction.
- Should be used concomitantly with emollients.
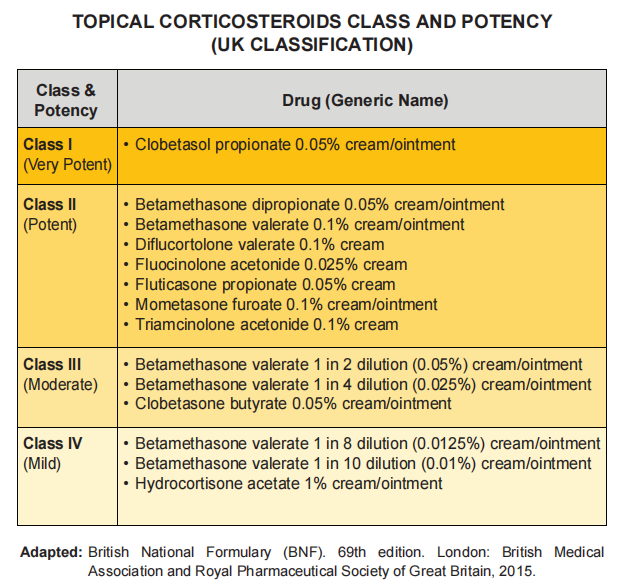
- Classification according to potency:
– Class I (very potent)
– Class II (potent)
– Class III (moderate)
– Class IV (mild) - Children have an increased absorption of TCS due to greater body surface area to weight ratio. Thus, the least potent but effective TCS should be used.
– However, during acute flare, use of short courses of moderate-very potent TCS can be considered for rapid control.
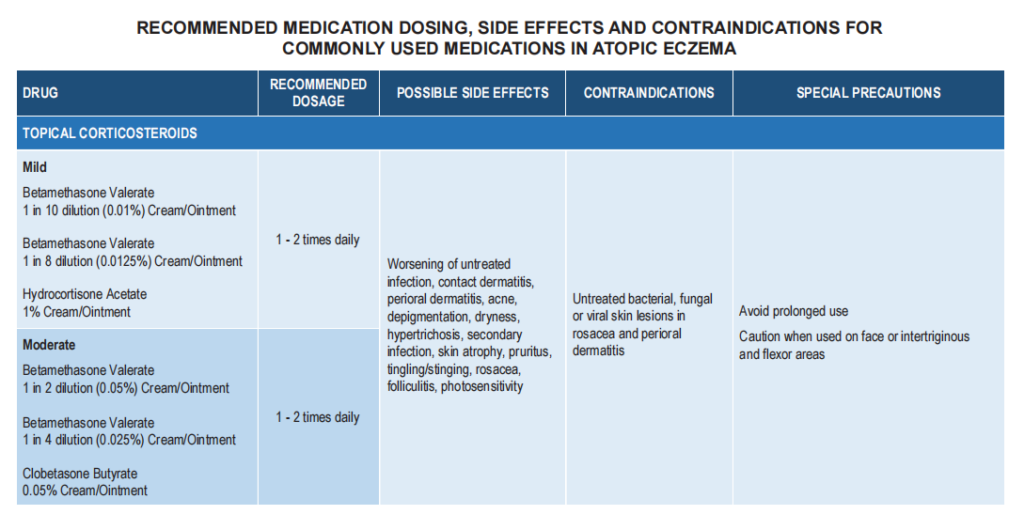
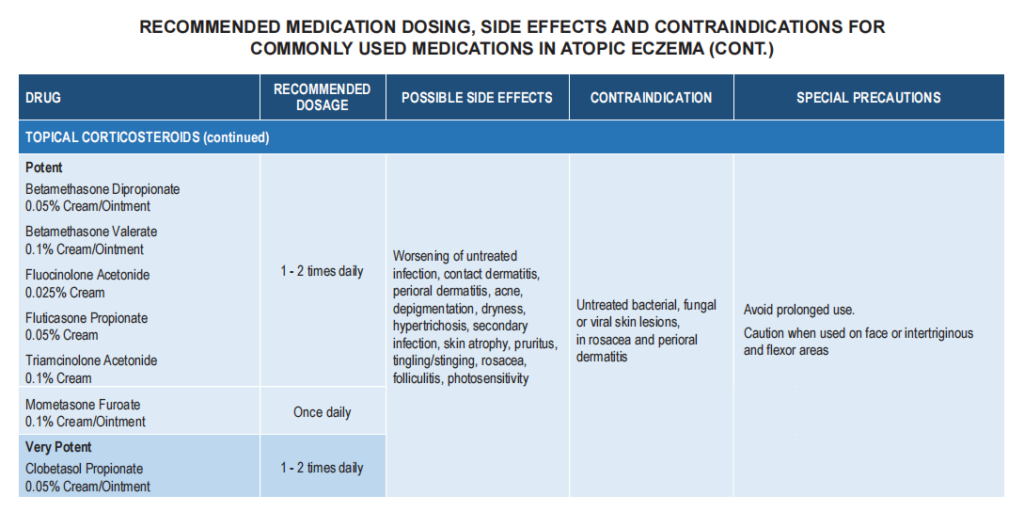
Practical guide for TCS application
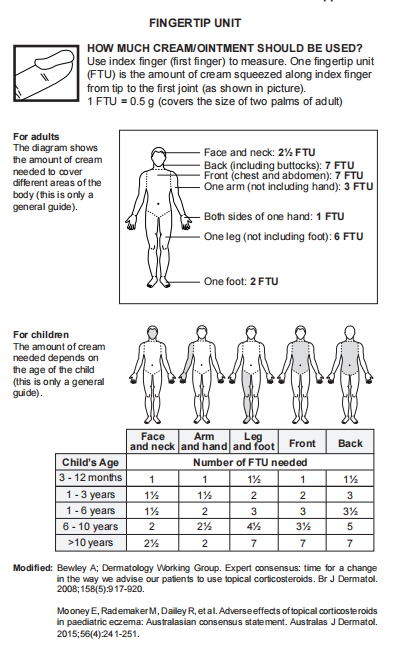
- The fingertip unit (FTU) has been used as a method of determining the amount of TCS to apply.
- Use concomitantly with emollients.
- Choice of vehicle depends on affected sites:
– Gel – scalp
– Cream – face, genital & flexural areas
– Ointment – palm & sole - Choice of potency depends on clinical severity
– Potent – very potent: thick lesions
– Mild- moderate potent: thin lesions. - After resolution of flares, discontinuation of TCS should be done gradually to avoid rebound (e.g. BD x 1/7 followed by OD x 1/7 then 1 – 3 times a week before complete discontinuation)
– Proactive therapy (mild TCS application intermittently once/twice a week) can be used to maintain remission. - Pt being treated with intermittent course of TCS should be reviewed every 3 – 6 months to ascertain response to therapy & potentially reversible atrophic changes.
C. Topical calcineurin inhibitors (TCIs)
- e.g tacrolimus & pimecrolimus
- May be considered to treat flares in patient > 2 years old
- Proactive treatment with TCIs 2 – 3 times weekly may be considered for maintenance therapy
- Most common adverse effects: burning, pruritus & skin infection
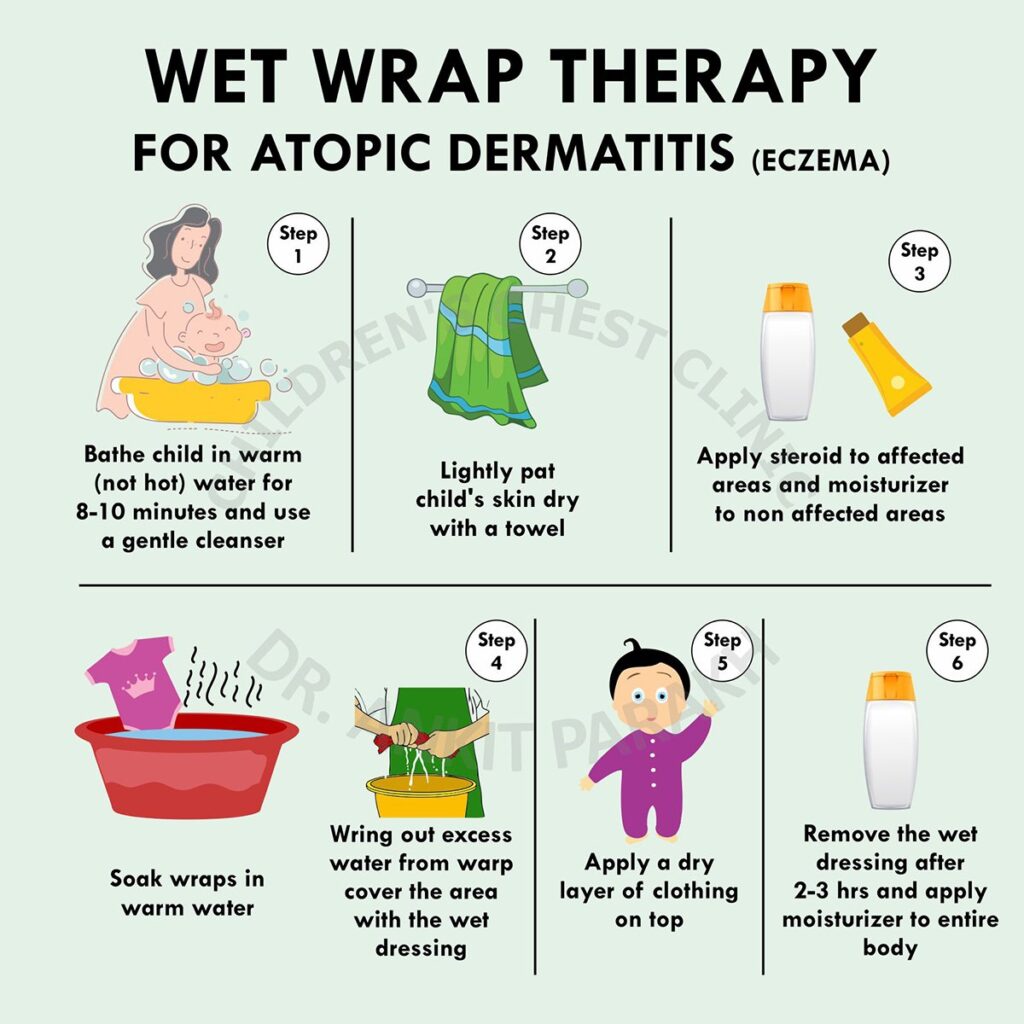
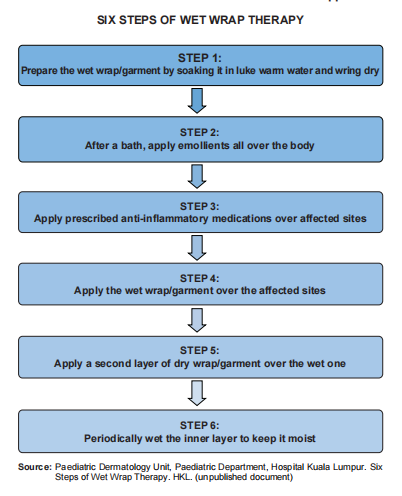
D. Wet Wrap Therapy (WWT)
- Consist of 2 layers of tubular bandage or garments with inner wet & outer dry layers, applied over moisturiser alone or in combination with TCS.
- Can be used continuously for 24 hours.
- WWT with moisturiser alone or in combination with mild-moderate potency TCS may be used in non-infected moderate to severe atopic eczema.
– The use of TCS In WWT should not > 14 days.
– WWT + emollients alone can be continued until AE is controlled.
E. Others
- Bleach bath has been shown to improve severity of AE.
- Other antiseptic baths (e.g. potassium permanganate, triclosan, chlorhexidine, NS daps/wash over the face) may be helpful in reducing bacterial colonisation of the skin.
- Long-term continuous use of antiseptics should be avoided.
Systemic therapy
Includes adjunctive treatment (e.g. antihistamines & systemic antibiotics) and specific treatment (e.g. immunomodulating agent & biologics)
A. Antihistamines
- Should not be used as monotherapy or to substitute topical therapy.
- Sedating antihistamines may be considered as short-term measure at bedtime in AE pt with sleep disturbance.
- In the absence of urticaria & other atopic conditions, non-sedating antihistamines are not recommended.
B. Immunomodulating agents
- Systemic corticosteroids may be considered for short-term control of severe acute exacerbation.
– No serious A/E when used for 2 – 4 weeks.
– Common A/E: HTN, exacerbations of AE after termination of treatment. - Azathioprine, cyclosporin A, MTX or mycophenolate may be used in the treatment of severe AE after optimization of topical treatment.
C. Biologics
- Dupilumab (monoclonal antibody that blocks IL-4 and IL-13 receptors) is a potential biologic therapy in adult pt with moderate- severe AE after optimization of conventional therapy.
– Common A/E: nasopharyngitis, headache & skin infection.
D. Antimicrobials
- Staph. aureus colonisation of skin in pt with moderate-severe AE is common. The degree of colonisation significantly correlates with clinical severity & disease exacerbation.
- Topical Abx: insufficient evidence to support
– Combination of TCA + topical Abx compared with TCS alone showed no difference in global outcome for clinically infected eczema. - Systemic Abx may be considered when there is clinical evidence of infection in pt with AE. (routine use in non-infected AE is not recommended).
There is insufficient evidence to recommend dietary supplements in the management of atopic eczema.
Educational interventions should be considered as part of the management.
Traditional and complementary medicine should not replace conventional therapy.
Phototherapy
For patient with severe atopic eczema who do not respond or develop side effects to conventional treatment.
– Ultraviolet A1 may be used to control acute flares.
– Narrow-band ultraviolet B may be offered in moderate to severe chronic atopic eczema.
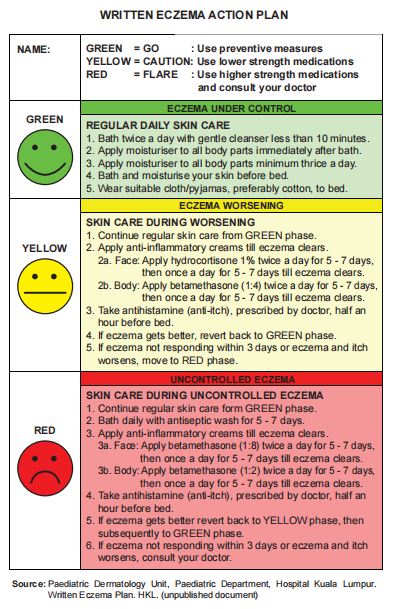
Written Eczema Action Plan
Referral
Urgent referral
- Atopic eczema with clinical suspicion of eczema herpeticum (eczema with widespread herpes simplex infection)
- Atopic eczema with severe skin bacterial infection that requires IV Abx.
- Atopic eczema with acute erythroderma where the eczema affects > 80% body surface area.
Non-urgent referral
- Diagnostic uncertainty
- Severe or uncontrolled eczema:
– Requirement of potent and very potent TCS.
– Frequent infections
– Poor sleep or excessive scratching
– Treatment failure with appropriate topical therapy regimen - Parental concern
- Need for treatment demonstration/education
- Involvement of sites that are difficult to treat.
- Psychological disturbance on the patient or family
Some learning points from CME attended
Main symptoms = pruritus
Usually will manifest as rashes by 5 years old. In infants, common site are the face and extensor surface. In older children, common site is the flexural region.
Management:
– Moisturizer and gentle cleanser (soap free cleanser) are mainstay.
– Topical steroids and topical calcineurin inhibitors can be used to bring down acute flare episodes.
– Higher than class I steroids can be applied on the face provided that the treating clinician is confident to look out for signs of skin atrophy (Early signs = telengactesia). Not recommended to use topical steroids for > 2 weeks. Moisturizer and gentle cleanser should continue on while on topical steroids.
– Calcineurin inhibitors may be more preferred as they do not have skin atrophy effect.
– Oral antibiotic may be useful for acute flares (Augmentin, Cefuroxime)