Menopause
Definition
- Menopause: No period for 12 months (1 year) without any preceding pathological or physiological cause [The average age of menopause in Malaysia is 50.7 years]
- Perimenopause: The time immediately before menopause till 1 year after the last menstrual period.

During this phase, erratic peaks in serum estradiol & progesterone can bring about a wide variation in cycles and flow.
– Cycles may be initially shorter followed by longer intervals.
– The flow may vary from prolonged spotting to heavy periods with clots.
– As ovulation can be unpredictable, contraception is still required till one year after the LMP.
- Diagnosis of perimenopause is purely clinical.
- Blood investigations for anemia, thyroid dysfunction & coagulation disorders (if necessary) are advised.
- AUB during the perimenopause should always be investigated, based on the FIGO classification system of PALM-COEIN
- Sexually active women p/w AUB should have a VE, pap smear & TVS TRO pathology in the cervix, uterus & ovaries.
- Pregnancy should also be ruled out.
Clinical assessment
Detailed history
- Personal history, including menopausal Sx; Menopausal Questionnaire
- Obstetric, gynaecological history
- Menstrual & sexual history
- Previous medical (e.g. h/o blood clotting problems), surgical history
- Allergic history
- Family history – hormone related cancers, CVS disease, clotting problems, osteoporosis.
- Social history: smoking, vaping, alcohol
- Lifestyle: stress, diet, exercise
General examination
- BP
- BMI
- Breast examination
- Abdominal examination, TRO pelvic masses
- VE (if applicable): TRO infections, cervical lesions, pelvic masses & to assess pelvic floor
Recommended investigations 🔎
- FBC, RP, LFT
- FBS, FSL
- Pap smear (if applicable)
- Breast screening using USG &/or mammography
- Bone mineral density (if needed)
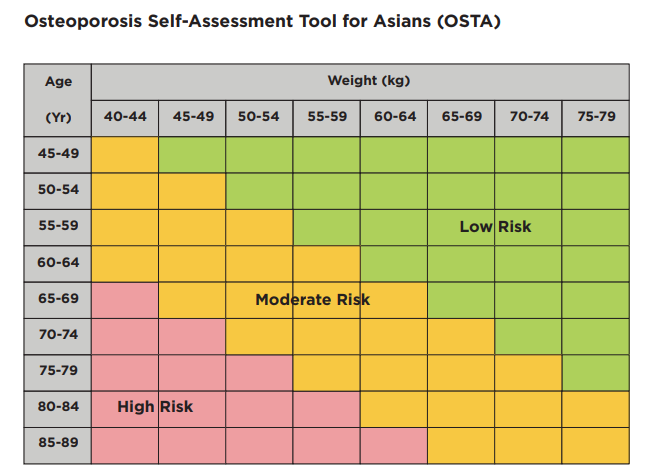
- OSTA can also be used to identify those at risk for osteoporosis.
- VE & pap smears are carried out only in women who are/have been sexually active.
- FSH should not be routinely considered when diagnosing menopause in women > 45 y/o
Management
Lifestyle changes
- Maintaining healthy weight
- Stop smoking or vaping
- Cutting down spicy food and excessive food
- Minimizing PUFA, trans fats, salt, & sugar.
- Minimizing alcohol
- BP control
- Regular exercise 5 days a week; 30 mins each time
- Sleeping soundly for 6 – 9 hours every night
- Stress reduction
- Support group programs (esp. spousal support)

Menopausal Hormonal Therapy (MHT)
Indications for MHT ✅
- Vasomotor symptoms
- Prevention of bone loss
- Hypoestrogenism due to e.g. hypogonadism, premature ovarian insufficiency, or premature surgical menopause
- Genitourinary syndrome of menopause
Contraindications of MHT 🚫
- Breast/endometrial CA (any hormone related cancer)
- Blood clots in the lungs, eyes, or deep veins
- Heart attack, stroke or TIA
- Liver disease or liver problems
- Inadequately controlled arterial HTN
- Undiagnosed uterine or vaginal bleeding
- Porphyria
- Pregnancy
Relative contraindications: Endometriosis, Fibroids (Annual pelvic USG is advised)
Types of MHT
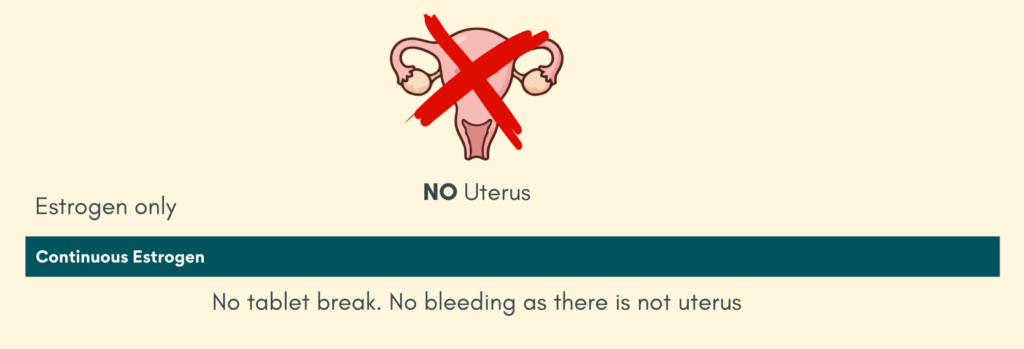
a) Hysterectomised women need only estrogen therapy
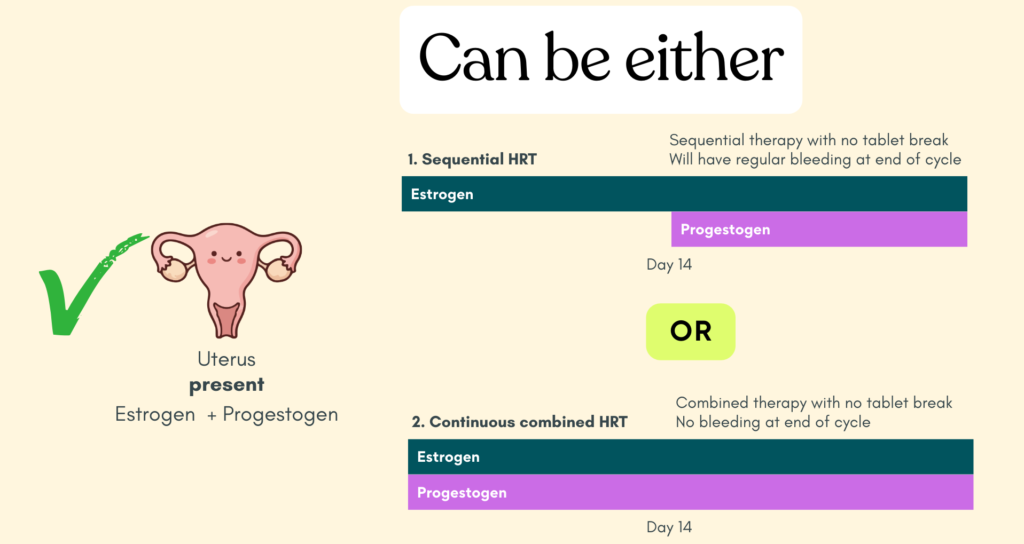
b) Non-hysterectomised women need both estrogen and progestogen. Progestogen is added for endometrial protection. Can be given as:
- Cyclical therapy – for perimenopause, will have regular period.
- Continuous combined therapy – for menopausal women, no bleed therapy
Hysterectomised women
Non-hysterectomised women
For continuous combined therapy:
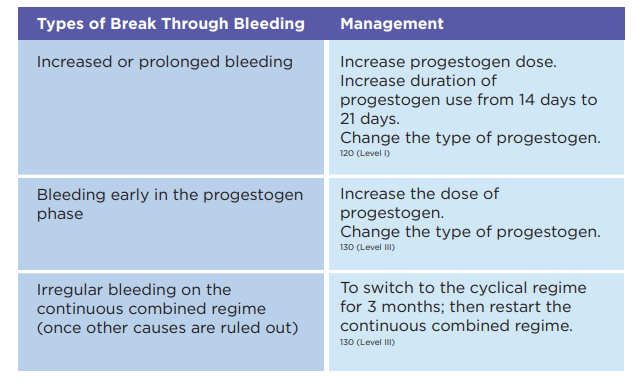
– Initial spotting or staining (break through bleeding) is common up to 6 months, after which there should not be any bleeding.
– Missing a pill/non-compliant may also cause irregular bleeding.
– Unschedule bleeding beyond 6 months should always be investigated.
Some key concept 🗝️
Benefits of MHT outweigh risks when given to healthy symptomatic women < 60 years or within 10 years of menopause & thus should be considered in these group of patients. (Women who initiate MHT 10 years after menopause have a higher absolute risk of CHD, stroke, venous thromboembolism & dementia.)
Women with perimenopausal Sx are advised either:
a) low dose COCP – acts as contraceptive, better cycle control & treats perimenopausal Sx.
b) MHT – better cycle control & treats perimenopausal Sx. Inadequate as contraceptive.
(Women above 50 years who are yet to reach menopause should be counselled about the 1% risk of pregnancy & additional contraceptive measures are to be taken)
c) LNG-IUS +- estrogen (orally or transdermal)
Low dose vaginal ET may be considered for relief of Sx of genitourinary syndrome of menopause. Additional progestogen therapy is not needed,
– Not indicated for treatment of hot flushes, prevention of osteoporosis, heart disease, or other major health conditions.
Any unscheduled vaginal bleeding should always be investigated.
Possible side effects of MHT
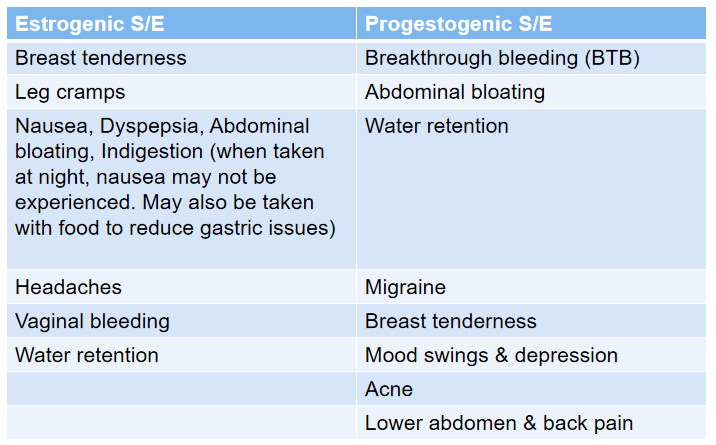
S/E are usually transient & resolves with time.
Women are encouraged to persist for at least 3 months to allow the initial S/E to settle.
Major S/E of concern:
- CVS – Stroke, CAD, Venous thromboembolism, PE
- Malignancies – Breast cancer, Endometrial cancer (increased risk if using estrogen alone in patient with intact uterus)
Management of Breakthrough Bleeding (BTB)
Follow up after starting MHT
Initial review after 3 months to check on S/E & effectiveness of treatment.
Upon a satisfactory review, annual consultation is advised.
During the f/up, things to review:
- BP, PR & BMI
- Any S/E, e.g. breast tenderness, nausea, headaches & bleeding
- Presence of any new gynecological or non-gynecological problems
- Regular breast evaluation. Mammogram &/or breast USG are carried out 1 – 2 yearly depending on screening test & risk of breast CA.
- Cervical screening (if applicable) at 1 – 3 yearly intervals
- Review & discussion on benefit-risk ratio
- Relevant blood IX, i.e. lipids & glucose.
Reason for earlier follow up
- Unscheduled vaginal bleeding
- Persistent S/E to MHT
- Persistent menopausal Sx
- Recent blood-clotting disorder
- Recent Sx of CVS disease
- Recent hormone-dependent breast CA or another hormone-dependent CA
- Any recent new gynecological or non-gynecological problem that is of concern to the individual
Factors to be considered if patient remains symptomatic whilst on MHT:
- GI disturbances leading to poor absorption
- Drug interactions leading to reduced bioavailability e.g. carbamazepine, phenytoin
- Other medical problems mimicking menopause e.g. hypothyroidism, DM
- Inadequate estrogen dose
- Patient’s expectations that all menopausal symptoms will be resolved.
Duration of use for MHT ⏰
- Presently no mandatory limitation to duration of MHT use.
- Factors to be taken into consideration of continuous use of MHT include:
– Pt’s personal preferences.
– Yearly review with benefit-risk assessment.
– Whether the primary use of MHT is for prevention or for QOL purposes. - When long term MHT(> 10 yrs) is considered, a low dose hormonal regime is advised.
- Continued use of MHT (> 10 years) is recommended in those with persistent VMS, to improve symptoms related to GSM, to increase bone density & to reduce fracture at all sites.
Reasons for stopping MHT 🛑
- New contraindications
- Risks > benefits
- Side effects
- Persistence of symptoms
- Pt’s preference
Possible of symptoms recurrence upon stopping MHT.
MHT should be ceased gradually over a period of 3 – 6 months rather than abruptly, to avoid rebound of Sx.
Alternative pharmacological therapy
Alternative treatment may be required for those who are contraindicated of MHT but having specific Sx of VMS & GSM
Alternative pharmacological therapy:
- Clonidine (anti-hypertensive)
- SNRIs (venlafaxine 100 mg/day)
- SSRIs – paroxetine, fluoxetine, citalopram & escitalopram
- Antiepileptics – gabapentin 300 mg TDS, pregabalin 75 mg BD.
Supplements
- 1200 mgs of calcium (dietary + supplements) is recommended daily for its +ve effect on BMD & fracture risk reduction.
- Adequate Vit. D supplementation (600 IU in women below 70 years & 800 IU after 70 years) reduces the risk of fracture & falls.
(Aim to achieve Vit. D levels of > 50 ng/mL)
Algorithm summary
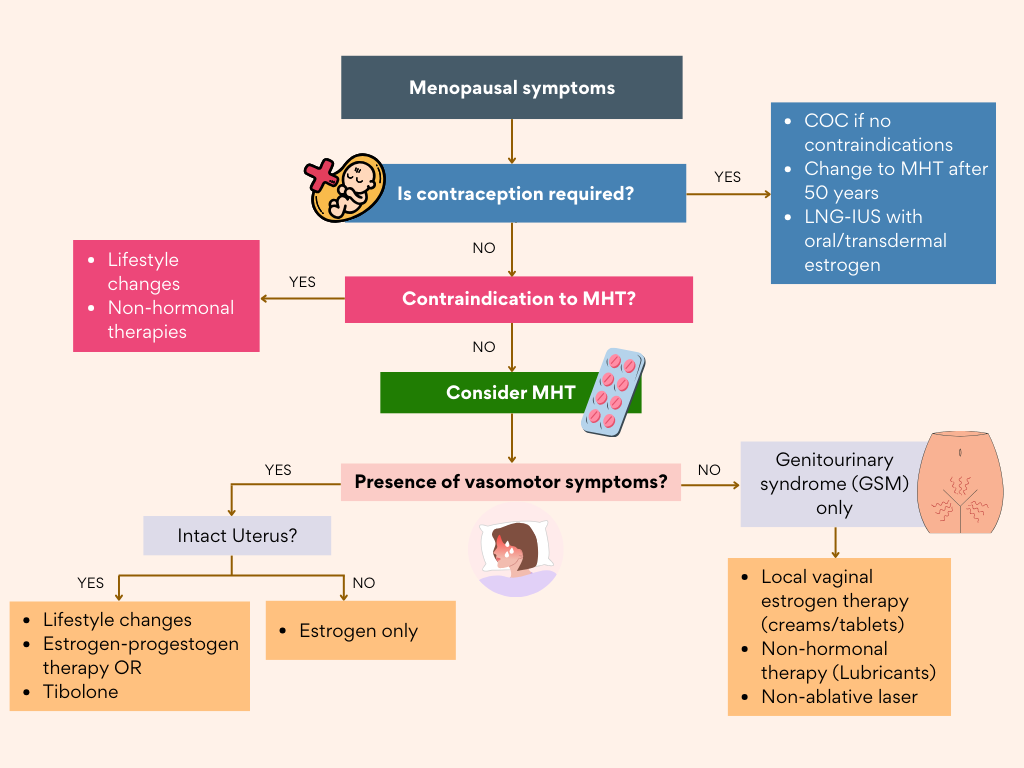
MHT: Menopausal Hormonal Therapy; GSM: Genitourinary Syndrome of Menopause;
Clickable decision making based on the above algorithm
• COC if no contraindications
• OR LNG-IUS + estrogen
• Switch to MHT after age 50
(continuous/sequential, LNG-IUS + estrogen, or tibolone)
Reference
Ministry of Health Malaysia. (2022). Clinical practice guidelines: Management of menopause in Malaysia. Putrajaya: Ministry of Health Malaysia
